J Korean Soc Radiol.
2015 Feb;72(2):92-100. 10.3348/jksr.2015.72.2.92.
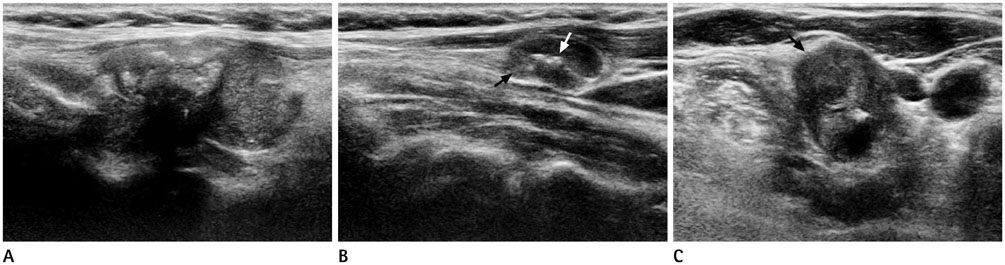
Ultrasonographic Features of Metastatic Lymph Nodes in Papillary Thyroid Microcarcinomas and Macrocarcinomas
- Affiliations
-
- 1Department of Radiology, Kosin University Gospel Hospital, Busan, Korea. soinvain@naver.com
- KMID: 2002804
- DOI: http://doi.org/10.3348/jksr.2015.72.2.92
Abstract
- PURPOSE
To analyze ultrasonographic (US) features of metastatic lymph nodes (LNs) in papillary thyroid microcarcinomas (PTMC) and in papillary thyroid macrocarcinomas.
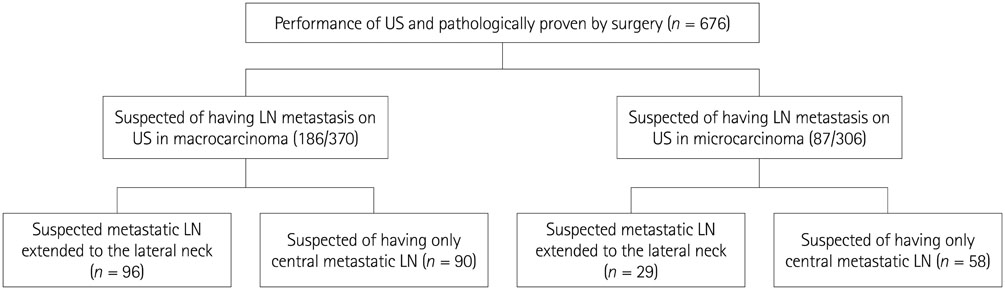
MATERIALS AND METHODS
The study reviewed US findings of 273 patients with pathologically confirmed papillary thyroid carcinoma (PTC) and metastatic LNs based on the US examination. Patients were divided into two groups: PTMC and papillary thyroid macrocarcinomas.
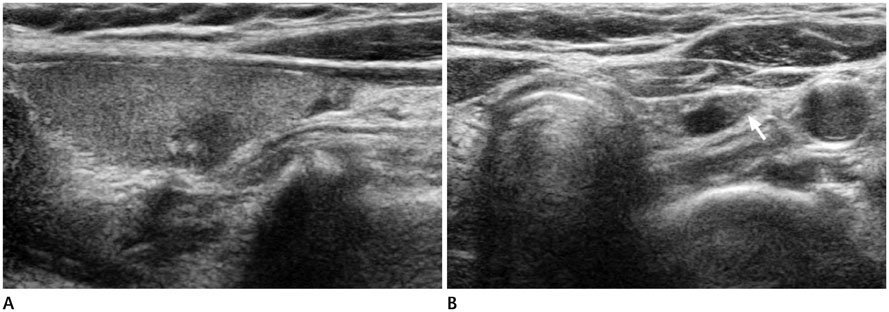
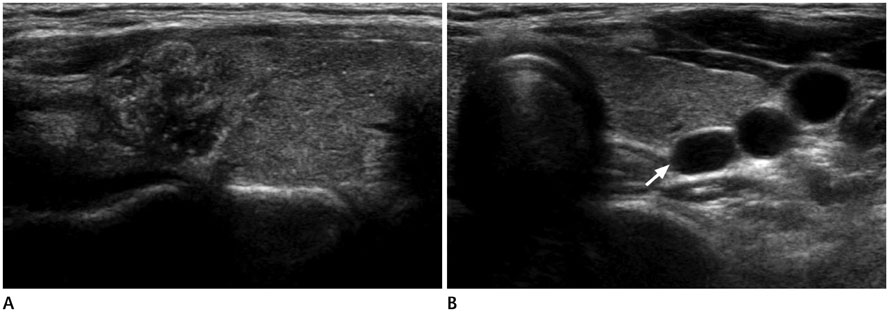
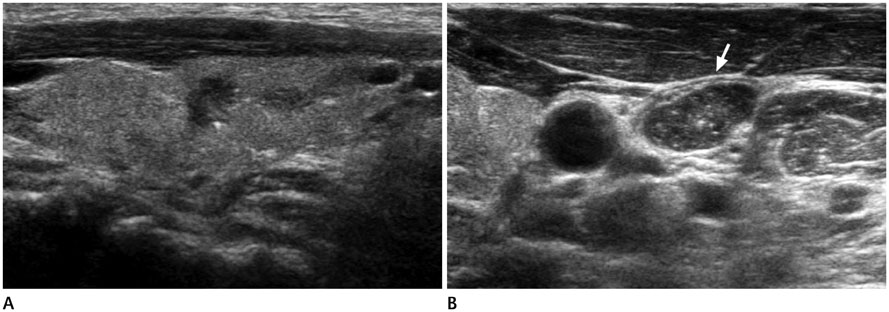
RESULTS
The 273 patients with PTC included 87 with PTMC and 186 with papillary thyroid macrocarcinoma. No significant difference of US features in patients with lateral neck node metastasis was found between PTMC (n = 96) and macrocarcinoma (n = 29). In central neck node metastasis, round shape was the most frequent findings in both groups (p < 0.001).
CONCLUSION
There was no significant difference in US features of metastatic LNs between PTMC and papillary thyroid macrocarcinomas. Therefore, careful evaluation of the whole neck should be made.
Figure
Reference
-
1. Hedinger CE, Williams ED, Sobin LH. Histologic typing of thyroid tumours. 2nd ed. Berlin: Springer-Verlag Berlin Heidelberg;1988. p. 9–10.2. Baudin E, Travagli JP, Ropers J, Mancusi F, Bruno-Bossio G, Caillou B, et al. Microcarcinoma of the thyroid gland: the Gustave-Roussy Institute experience. Cancer. 1998; 83:553–559.3. Chow SM, Law SC, Chan JK, Au SK, Yau S, Lau WH. Papillary microcarcinoma of the thyroid-Prognostic significance of lymph node metastasis and multifocality. Cancer. 2003; 98:31–40.4. Lee J, Rhee Y, Lee S, Ahn CW, Cha BS, Kim KR, et al. Frequent, aggressive behaviors of thyroid microcarcinomas in Korean patients. Endocr J. 2006; 53:627–632.5. Hartl DM, Travagli JP. The updated American Thyroid Association Guidelines for management of thyroid nodules and differentiated thyroid cancer: a surgical perspective. Thyroid. 2009; 19:1149–1151.6. Tuttle RM, Ball DW, Byrd D, Dilawari RA, Doherty GM, Duh QY, et al. Thyroid carcinoma. J Natl Compr Canc Netw. 2010; 8:1228–1274.7. British Thyroid Association. Royal College of Physicians Lodon. Guidelines for the management of thyroid cancer. 2nd ed. London: The Lavenham Press;2007. p. 13–15.8. American Thyroid Association (ATA) Guidelines Taskforce on Thyroid Nodules and Differentiated Thyroid Cancer. Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, et al. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2009; 19:1167–1214.9. Ito Y, Tomoda C, Uruno T, Takamura Y, Miya A, Kobayashi K, et al. Preoperative ultrasonographic examination for lymph node metastasis: usefulness when designing lymph node dissection for papillary microcarcinoma of the thyroid. World J Surg. 2004; 28:498–501.10. Hwang HS, Orloff LA. Efficacy of preoperative neck ultrasound in the detection of cervical lymph node metastasis from thyroid cancer. Laryngoscope. 2011; 121:487–491.11. Boland GW, Lee MJ, Mueller PR, Mayo-Smith W, Dawson SL, Simeone JF. Efficacy of sonographically guided biopsy of thyroid masses and cervical lymph nodes. AJR Am J Roentgenol. 1993; 161:1053–1056.12. Ying M, Ahuja A, Metreweli C. Diagnostic accuracy of sonographic criteria for evaluation of cervical lymphadenopathy. J Ultrasound Med. 1998; 17:437–445.13. Rosário PW, de Faria S, Bicalho L, Alves MF, Borges MA, Purisch S, et al. Ultrasonographic differentiation between metastatic and benign lymph nodes in patients with papillary thyroid carcinoma. J Ultrasound Med. 2005; 24:1385–1389.14. Vassallo P, Wernecke K, Roos N, Peters PE. Differentiation of benign from malignant superficial lymphadenopathy: the role of high-resolution US. Radiology. 1992; 183:215–220.15. Shah JP. Cervical lymph node metastases--diagnostic, therapeutic, and prognostic implications. Oncology (Williston Park). 1990; 4:61–69. discussion 72, 76.16. Som PM, Curtin HD, Mancuso AA. An imaging-based classification for the cervical nodes designed as an adjunct to recent clinically based nodal classifications. Arch Otolaryngol Head Neck Surg. 1999; 125:388–396.17. Snozek CL, Chambers EP, Reading CC, Sebo TJ, Sistrunk JW, Singh RJ, et al. Serum thyroglobulin, high-resolution ultrasound, and lymph node thyroglobulin in diagnosis of differentiated thyroid carcinoma nodal metastases. J Clin Endocrinol Metab. 2007; 92:4278–4281.18. Uruno T, Miyauchi A, Shimizu K, Tomoda C, Takamura Y, Ito Y, et al. Usefulness of thyroglobulin measurement in fine-needle aspiration biopsy specimens for diagnosing cervical lymph node metastasis in patients with papillary thyroid cancer. World J Surg. 2005; 29:483–485.19. Grodski S, Brown T, Sidhu S, Gill A, Robinson B, Learoyd D, et al. Increasing incidence of thyroid cancer is due to increased pathologic detection. Surgery. 2008; 144:1038–1043. discussion 1043.20. Pazaitou-Panayiotou K, Capezzone M, Pacini F. Clinical features and therapeutic implication of papillary thyroid microcarcinoma. Thyroid. 2007; 17:1085–1092.21. Mazzaferri EL. Managing small thyroid cancers. JAMA. 2006; 295:2179–2182.22. Vasileiadis I, Karakostas E, Charitoudis G, Stavrianaki A, Kapetanakis S, Kouraklis G, et al. Papillary thyroid microcarcinoma: clinicopathological characteristics and implications for treatment in 276 patients. Eur J Clin Invest. 2012; 42:657–664.23. Scheumann GF, Gimm O, Wegener G, Hundeshagen H, Dralle H. Prognostic significance and surgical management of locoregional lymph node metastases in papillary thyroid cancer. World J Surg. 1994; 18:559–567.24. Wada N, Duh QY, Sugino K, Iwasaki H, Kameyama K, Mimura T, et al. Lymph node metastasis from 259 papillary thyroid microcarcinomas: frequency, pattern of occurrence and recurrence, and optimal strategy for neck dissection. Ann Surg. 2003; 237:399–407.25. Arora N, Turbendian HK, Kato MA, Moo TA, Zarnegar R, Fahey TJ 3rd. Papillary thyroid carcinoma and microcarcinoma: is there a need to distinguish the two? Thyroid. 2009; 19:473–477.26. Machens A, Hinze R, Thomusch O, Dralle H. Pattern of nodal metastasis for primary and reoperative thyroid cancer. World J Surg. 2002; 26:22–28.27. Grebe SK, Hay ID. Thyroid cancer nodal metastases: biologic significance and therapeutic considerations. Surg Oncol Clin N Am. 1996; 5:43–63.28. Gimm O, Rath FW, Dralle H. Pattern of lymph node metastases in papillary thyroid carcinoma. Br J Surg. 1998; 85:252–254.29. Page C, Biet A, Boute P, Cuvelier P, Strunski V. 'Aggressive papillary' thyroid microcarcinoma. Eur Arch Otorhinolaryngol. 2009; 266:1959–1963.30. Joo JY, Park JY, Yoon YH, Choi B, Kim JM, Jo YS, et al. Prediction of occult central lymph node metastasis in papillary thyroid carcinoma by preoperative BRAF analysis using fine-needle aspiration biopsy: a prospective study. J Clin Endocrinol Metab. 2012; 97:3996–4003.31. Kim BY, Jung CH, Kim JW, Lee SW, Kim CH, Kang SK, et al. Impact of clinicopathologic factors on subclinical central lymph node metastasis in papillary thyroid microcarcinoma. Yonsei Med J. 2012; 53:924–930.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Cystic Lymph Node Metastasis from Thyroid Papillary Microcarcinoma
- The histological features of papillary thyroid carcinomas 1.5 cm and less in size
- Langerhans Cell Histiocytosis in the Thyroid and Draining Lymph Nodes: A Case Report
- A Case of Papillary Thyroid Microcarcinoma Presenting as a Contralateral Cervical Lymph Node Metastasis
- A Case of Thyroid Papillary Microcarcinoma with Submental Node Metastasis