Restor Dent Endod.
2012 Mar;37(1):41-49. 10.5395/rde.2012.37.1.41.
Evaluation of internal adaptation of dental adhesive restorations using micro-CT
- Affiliations
-
- 1Department of Conservative Dentistry, Yonsei University School of Dentistry and Oral Science Research Center, Seoul, Korea. sunghopark@yuhs.ac
- KMID: 1995683
- DOI: http://doi.org/10.5395/rde.2012.37.1.41
Abstract
OBJECTIVES
The internal adaptation of composite restorations with or without resin modified glass ionomer cement (RMGIC) was analyzed non-destructively using Microcomputed tomography (micro-CT).
MATERIALS AND METHODS
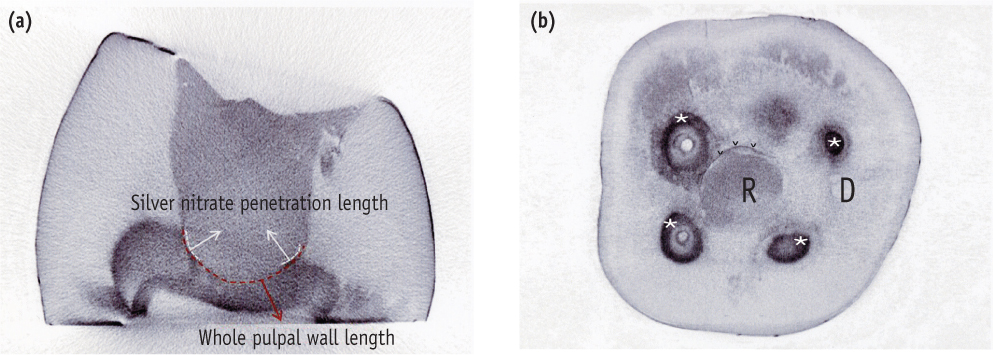
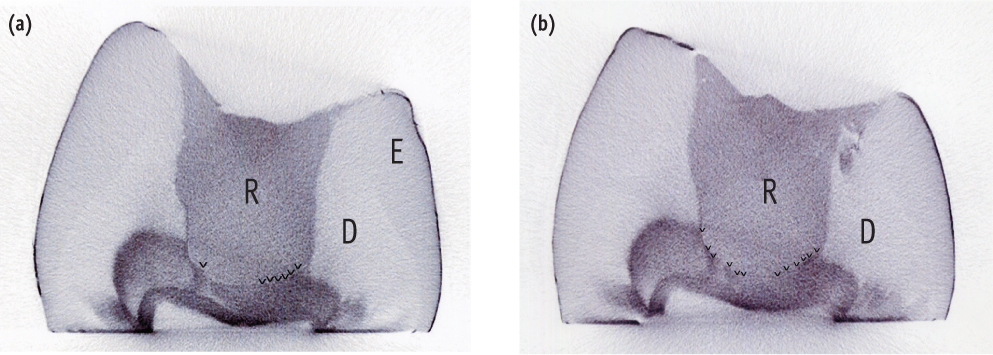
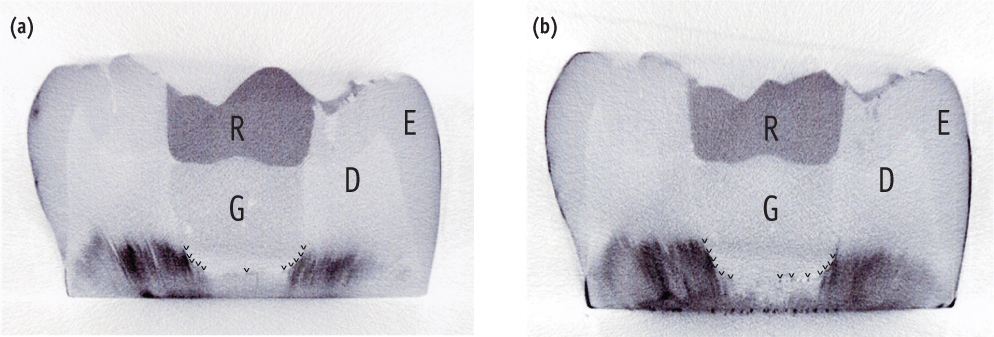
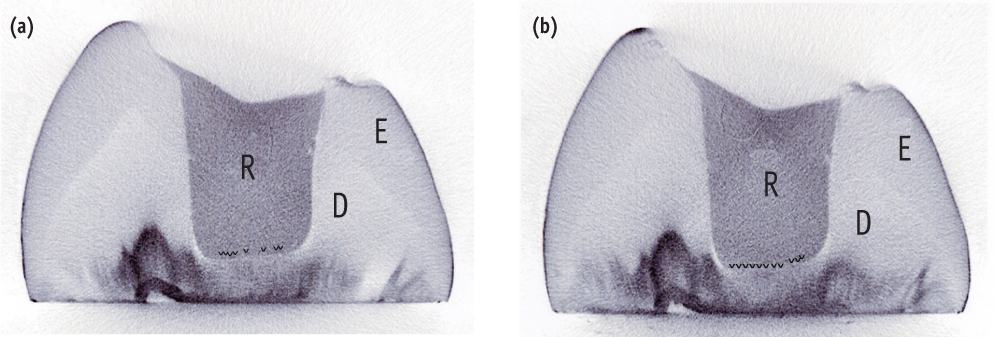
Thirty intact human teeth were used. The specimens were divided into 3 groups. In the control group, the cavities were etched with 10% phosphoric acid for 15 sec. Composite resin was filled into the cavity without adhesive. In group 1, light cured glass ionomer cement (GIC, Fuji II LC, GC) was applied as a base. The cavities were then etched, bonded, light cured and filled with composites. In group 2, the cavities were then etched, bonded, light cured and filled with composites without base application. They were immersed in a 25% silver nitrate solution. Micro-CT was performed before and after mechanical loading. One-way ANOVA with Duncan analysis was used to compare the internal adaptation between the groups before or after loading. A paired t-test was used to compare internal adaptation before and after mechanical loading. All statistical inferences were made within the 95% confidence interval.
RESULTS
The silver nitrate solution successfully penetrated into the dentinal tubules from the pulp spaces, and infiltrated into the gap between restoration and pulpal floor. Group 2 showed a lower adaptation than the control group and group 1 (p < 0.05). There was no significant difference between the control group and group 1. For all groups, there was a significant difference between before and after mechanical loading (p < 0.05).
CONCLUSIONS
The internal adaptation before and after loading was better when composites were bonded to tooth using adhesive than composites based with RMGIC.
Keyword
MeSH Terms
-
Acrylic Resins
Adhesives
Dental Cements
Dentin
Floors and Floorcoverings
Glass Ionomer Cements
Humans
Light
Phosphoric Acids
Resins, Synthetic
Silicon Dioxide
Silver Nitrate
Tooth
X-Ray Microtomography
Acrylic Resins
Adhesives
Dental Cements
Glass Ionomer Cements
Phosphoric Acids
Resins, Synthetic
Silicon Dioxide
Silver Nitrate
Figure
Cited by 1 articles
-
Micro-CT evaluation of internal adaptation in resin fillings with different dentin adhesives
Seung-Hoon Han, Sung-Ho Park
Restor Dent Endod. 2014;39(1):24-31. doi: 10.5395/rde.2014.39.1.24.
Reference
-
1. Retief DH. Do adhesives prevent microleakage? Int Dent J. 1994. 44:19–26.2. Friedl KH, Schmalz G, Hiller KA, Mortazavi F. Marginal adaptation of composite restorations versus hybrid ionomer/composite sandwich restorations. Oper Dent. 1997. 22:21–29.3. Tolidis K, Nobecourt A, Randall RC. Effect of a resin-modified glass ionomer liner on volumetric polymerization shrinkage of various composites. Dent Mater. 1998. 14:417–423.
Article4. Krejci I, Lutz F, Krejci D. The influence of different base materials on marginal adaptation and wear of conventional Class II composite resin restorations. Quintessence Int. 1988. 19:191–198.5. Unemori M, Matsuya Y, Akashi A, Goto Y, Akamine A. Composite resin restoration and postoperative sensitivity: clinical follow-up in an undergraduate program. J Dent. 2001. 29:7–13.
Article6. van Dijken JW. A 6-year clinical evaluation of Class I poly-acid modified resin composite/resin composite laminate restorations cured with a two-step curing technique. Dent Mater. 2003. 19:423–428.
Article7. Opdam NJ, Bronkhorst EM, Roeters JM, Loomans BA. Longevity and reasons for failure of sandwich and totaletch posterior composite resin restorations. J Adhes Dent. 2007. 9:469–475.8. Kwon OH, Kim DH, Park SH. The influence of elastic modulus of base material on the marginal adaptation of direct composite restoration. Oper Dent. 2010. 35:441–447.
Article9. Hayashi M, Wilson NH. Marginal deterioration as a predictor of failure of a posterior composite. Eur J Oral Sci. 2003. 111:155–162.
Article10. Souza-Junior EJ, de Souza-Régis MR, Alonso RC, de Freitas AP, Sinhoreti MA, Cunha LG. Effect of the curing method and composite volume on marginal and internal adaptation of composite restoratives. Oper Dent. 2011. 36:231–238.
Article11. Carvalho RM, Pereira JC, Yoshiyama M, Pashley DH. A review of polymerization contraction: the influence of stress development versus stress relief. Oper Dent. 1996. 21:17–24.12. Tay FR, Pashley DH. Water treeing-a potential mechanism for degradation of dentin adhesives. Am J Dent. 2003. 16:6–12.13. Ratih DN, Palamara JE, Messer HH. Minimizing dentinal fluid flow associated with gap formation. J Dent Res. 2006. 85:1027–1031.
Article14. Banomyong D, Palamara JE, Messer HH, Burrow MF. Sealing ability of occlusal resin composite restoration using four restorative procedures. Eur J Oral Sci. 2008. 116:571–578.
Article15. Ciucchi B, Bouillaguet S, Delaloye M, Holz J. Volume of the internal gap formed under composite restorations in vitro. J Dent. 1997. 25:305–312.
Article16. Peliz MI, Duarte S Jr, Dinelli W. Scanning electron microscope analysis of internal adaptation of materials used for pulp protection under composite resin restorations. J Esthet Restor Dent. 2005. 17:118–128.
Article17. Ishibashi K, Ozawa N, Tagami J, Sumi Y. Swept-source optical coherence tomography as a new tool to evaluate defects of resin-based composite restorations. J Dent. 2011. 39:543–548.
Article18. Sun J, Eidelman N, Lin-Gibson S. 3D mapping of polymerization shrinkage using X-ray micro-computed tomography to predict microleakage. Dent Mater. 2009. 25:314–320.
Article19. Zeiger DN, Sun J, Schumacher GE, Lin-Gibson S. Evaluation of dental composite shrinkage and leakage in extracted teeth using X-ray microcomputed tomography. Dent Mater. 2009. 25:1213–1220.
Article20. Kakaboura A, Rahiotis C, Watts D, Silikas N, Eliades G. 3D-marginal adaptation versus setting shrinkage in light-cured microhybrid resin composites. Dent Mater. 2007. 23:272–278.
Article21. Eden E, Topaloglu-Ak A, Cuijpers V, Frencken JE. Micro-CT for measuring marginal leakage of Class II resin composite restorations in primary molars prepared in vivo. Am J Dent. 2008. 21:393–397.22. Peters OA, Laib A, Rüegsegger P, Barbakow F. Three-dimensional analysis of root canal geometry by high-resolution computed tomography. J Dent Res. 2000. 79:1405–1409.
Article23. Hotta M, Aono M. Adaptation to the cavity floor of the light-cured glass ionomer cement base under a composite restoration. J Oral Rehabil. 1994. 21:679–685.
Article24. Oliveira LC, Duarte S Jr, Araujo CA, Abrahão A. Effect of low-elastic modulus liner and base as stress-absorbing layer in composite resin restorations. Dent Mater. 2010. 26:e159–e169.
Article25. Nomoto R, Komoriyama M, McCabe JF, Hirano S. Effect of mixing method on the porosity of encapsulated glass ionomer cement. Dent Mater. 2004. 20:972–978.
Article26. Retief DH, Mandras RS, Russell CM. Shear bond strength required to prevent microleakage of the dentin/restoration interface. Am J Dent. 1994. 7:44–46.27. Erickson RL, Glasspoole EA. Bonding to tooth structure: a comparison of glass-ionomer and composite-resin systems. J Esthet Dent. 1994. 6:227–244.
Article28. Nery S, McCabe JF, Wassell RW. A comparative study of three dental adhesives. J Dent. 1995. 23:55–61.
Article29. Tjan AH, Castelnuovo J, Liu P. Bond strength of multistep and simplified-step systems. Am J Dent. 1996. 9:269–272.30. Triolo PT Jr, Swift EJ Jr, Barkmeier WW. Shear bond strengths of composite to dentin using six dental adhesive systems. Oper Dent. 1995. 20:46–50.31. van der Vyver PJ, de Wet FA. Shear bond strength of four dentine bonding systems to dry and moist dentine. J Dent Assoc S Afr. 1997. 52:555–558.32. Eliades G, Palaghias G. In vitro characterization of visible light-cured glass ionomer liners. Dent Mater. 1993. 9:198–203.33. Cattani-Lorente MA, Dupuis V, Moya F, Payan J, Meyer JM. Comparative study of the physical properties of a polyacid-modified composite resin and a resin-modified glass ionomer cement. Dent Mater. 1999. 15:21–32.
Article34. Tam LE, McComb D, Pulver F. Physical properties of proprietary light-cured lining materials. Oper Dent. 1991. 16:210–217.35. Tam LE, Pulver E, McComb D, Smith DC. Physical properties of calcium hydroxide and glass-ionomer base and lining materials. Dent Mater. 1989. 5:145–149.
Article36. Young AM. FTIR investigation of polymerisation and polyacid neutralisation kinetics in resin-modified glass-ionomer dental cements. Biomaterials. 2002. 23:3289–3295.
Article37. Feilzer AJ, Kakaboura AI, de Gee AJ, Davidson CL. The influence of water sorption on the development of setting shrinkage stress in traditional and resin-modified glass ionomer cements. Dent Mater. 1995. 11:186–190.
Article38. Mason PN, Ferrari M. In vivo evaluation of glass-ionomer cement adhesion to dentin. Quintessence Int. 1994. 25:499–504.39. Akpata ES, Sadiq W. Post-operative sensitivity in glass-ionomer versus adhesive resin-lined posterior composites. Am J Dent. 2001. 14:34–38.40. Burrow MF, Banomyong D, Harnirattisai C, Messer HH. Effect of glass-ionomer cement lining on postoperative sensitivity in occlusal cavities restored with resin composite-a randomized clinical trial. Oper Dent. 2009. 34:648–655.
Article41. Unemori M, Matsuya Y, Akashi A, Goto Y, Akamine A. Composite resin restoration and postoperative sensitivity: clinical follow-up in an undergraduate program. J Dent. 2001. 29:7–13.
Article42. Heintze SD. Systematic reviews: I. The correlation between laboratory tests on marginal quality and bond strength. II. The correlation between marginal quality and clinical outcome. J Adhes Dent. 2007. 9:Supplement 1. 77–106.43. Heintze S, Forjanic M, Cavalleri A. Microleakage of Class II restorations with different tracers-comparison with SEM quantitative analysis. J Adhes Dent. 2008. 10:259–267.44. Chen X, Cuijpers V, Fan M, Frencken JE. Optimal use of silver nitrate and marginal leakage at the sealant-enamel interface using micro-CT. Am J Dent. 2009. 22:269–272.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Micro-CT evaluation of internal adaptation in resin fillings with different dentin adhesives
- Micro-computed tomography for assessing the internal and external voids of bulk-fill composite restorations: A technical report
- Micro-computed tomography in preventive and restorative dental research: A review
- Comparison of micro CT and cross-section technique for evaluation of marginal and internal fit of lithium disilicate crowns
- The shear bond strength of two adhesives bonded to composite resin and glass ionomer cement restorations