Korean J Pain.
2013 Apr;26(2):164-168. 10.3344/kjp.2013.26.2.164.
Searching for Hidden, Painful Osteochondral Lesions of the Ankle in Patients with Chronic Lower Limb Pain: Two Case Reports
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, School of Medicine, Pusan National University, Yangsan, Korea. pain@pusan.ac.kr
- 2Department of Anesthesiology and Pain Medicine, Chnagwon Samsung Medical Center, Changwon, Korea.
- KMID: 1978662
- DOI: http://doi.org/10.3344/kjp.2013.26.2.164
Abstract
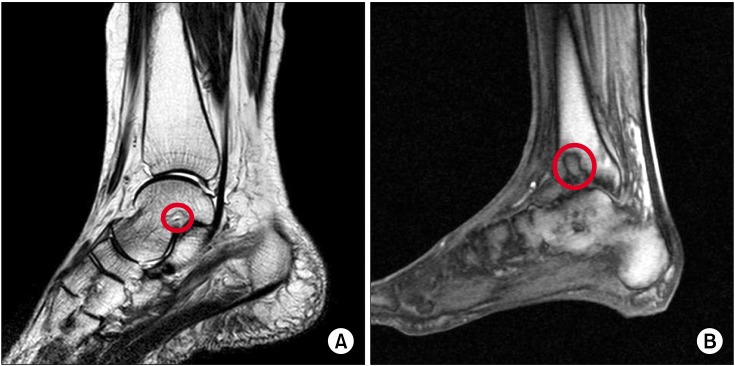
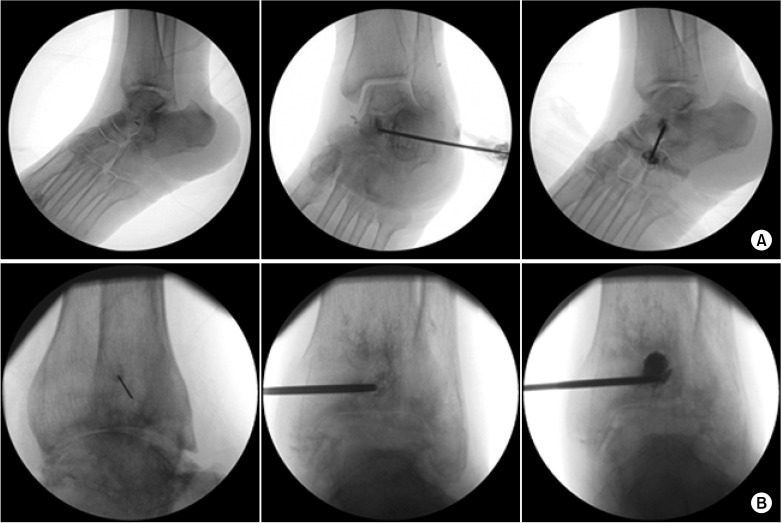
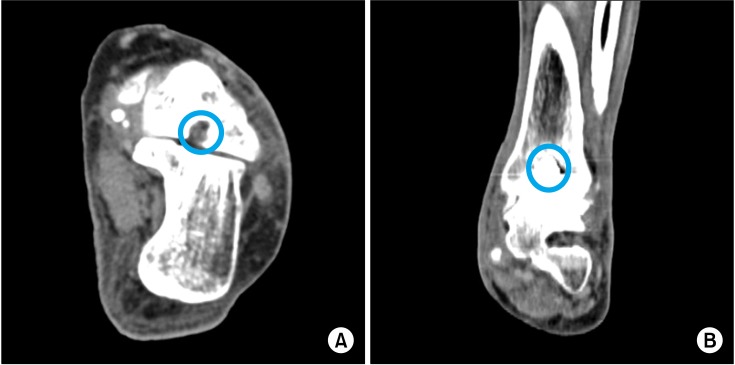
- It is easy to overlook osteochondral lesions (OCLs) of the ankle in patients with chronic lower limb pain, such as complex regional pain syndrome (CRPS) or thromboangiitis obliterans (TAO, Buerger's disease). A 57-year-old woman diagnosed with type 1 CRPS, and a 58-year-old man, diagnosed with TAO, complained of tactile and cold allodynia in their lower legs. After neurolytic lumbar sympathethic ganglion block and titration of medications for neuropathic pain, each subject could walk without the aid of crutches. However, they both complained of constant pain on the left ankle during walking. Focal tenderness was noted; subsequent imaging studies revealed OCLs of her talus and his distal tibia, respectively. Immediately after percutaneous osteoplasties, the patients could walk without ankle pain. It is important to consider the presence of a hidden OCL in chronic pain patients that develop weight-bearing pain and complain of localized tenderness on the ankle.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Percutaneous osteoplasty for painful bony lesions: a technical survey
Won-Sung Kim, Kyung-Hoon Kim
Korean J Pain. 2021;34(4):375-393. doi: 10.3344/kjp.2021.34.4.375.
Reference
-
1. Zengerink M, Struijs PA, Tol JL, van Dijk CN. Treatment of osteochondral lesions of the talus: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2010; 18:238–246. PMID: 19859695.
Article2. van Bergen CJ, de Leeuw PA, van Dijk CN. Treatment of osteochondral defects of the talus. Rev Chir Orthop Reparatrice Appar Mot. 2008; 94:398–408. PMID: 19046699.
Article3. van Dijk CN, Reilingh ML, Zengerink M, van Bergen CJ. The natural history of osteochondral lesions in the ankle. Instr Course Lect. 2010; 59:375–386. PMID: 20415393.4. Kreuz PC, Steinwachs M, Erggelet C, Lahm A, Henle P, Niemeyer P. Mosaicplasty with autogenous talar autograft for osteochondral lesions of the talus after failed primary arthroscopic management: a prospective study with a 4-year follow-up. Am J Sports Med. 2006; 34:55–63. PMID: 16157849.
Article5. Chew KT, Tay E, Wong YS. Osteochondral lesions of the talus. Ann Acad Med Singapore. 2008; 37:63–68. PMID: 18265900.6. O'Loughlin PF, Heyworth BE, Kennedy JG. Current concepts in the diagnosis and treatment of osteochondral lesions of the ankle. Am J Sports Med. 2010; 38:392–404. PMID: 19561175.7. Coderre TJ, Bennett GJ. A hypothesis for the cause of complex regional pain syndrome-type I (reflex sympathetic dystrophy): pain due to deep-tissue microvascular pathology. Pain Med. 2010; 11:1224–1238. PMID: 20704671.
Article8. Groeneweg G, Huygen FJ, Coderre TJ, Zijlstra FJ. Regulation of peripheral blood flow in complex regional pain syndrome: clinical implication for symptomatic relief and pain management. BMC Musculoskelet Disord. 2009; 10:116. PMID: 19775468.
Article9. Wasner G. Vasomotor disturbances in complex regional pain syndrome--a review. Pain Med. 2010; 11:1267–1273. PMID: 20704675.
Article10. Olin JW, Shih A. Thromboangiitis obliterans (Buerger's disease). Curr Opin Rheumatol. 2006; 18:18–24. PMID: 16344615.
Article11. Piazza G, Creager MA. Thromboangiitis obliterans. Circulation. 2010; 121:1858–1861. PMID: 20421527.
Article12. Seo SS, Park JY, Kim HJ, Yoon JW, Park SH, Kim KH. Percutaneous osteoplasty for the treatment of a painful osteochondral lesion of the talus: a case report and literature review. Pain Physician. 2012; 15:E743–E748. PMID: 22996869.13. Matsumine A, Myoui A, Kusuzaki K, Araki N, Seto M, Yoshikawa H, et al. Calcium hydroxyapatite ceramic implants in bone tumour surgery. A long-term follow-up study. J Bone Joint Surg Br. 2004; 86:719–725. PMID: 15274270.14. Yamamoto T, Onga T, Marui T, Mizuno K. Use of hydroxyapatite to fill cavities after excision of benign bone tumours. Clinical results. J Bone Joint Surg Br. 2000; 82:1117–1120. PMID: 11132269.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Osteochondral Lesion of the Calcaneus Involving the Subtalar Joint: A Case Report
- Simultaneously Occurred Medial and Lateral Osteochondral Lesions of the Talus
- Osteochondral Lesions of the Talus
- Supramalleolar Osteotomy Combined with Redo Arthroscopy for a Patient with Persistent Pain after Primary Arthroscopic Microfracture for Medial Osteochondral Lesion of the Talus: A Case Report
- Osteochondral Lesions of the Talus: Autologous Osteochondral Transplantation