Ultrasound-Guided Pain Interventions: A Review of Techniques for Peripheral Nerves
- Affiliations
-
- 1Toronto Western Hospital, University Health Network, University of Toronto, Canada. Philip.peng@uhn.ca
- KMID: 1978654
- DOI: http://doi.org/10.3344/kjp.2013.26.2.111
Abstract
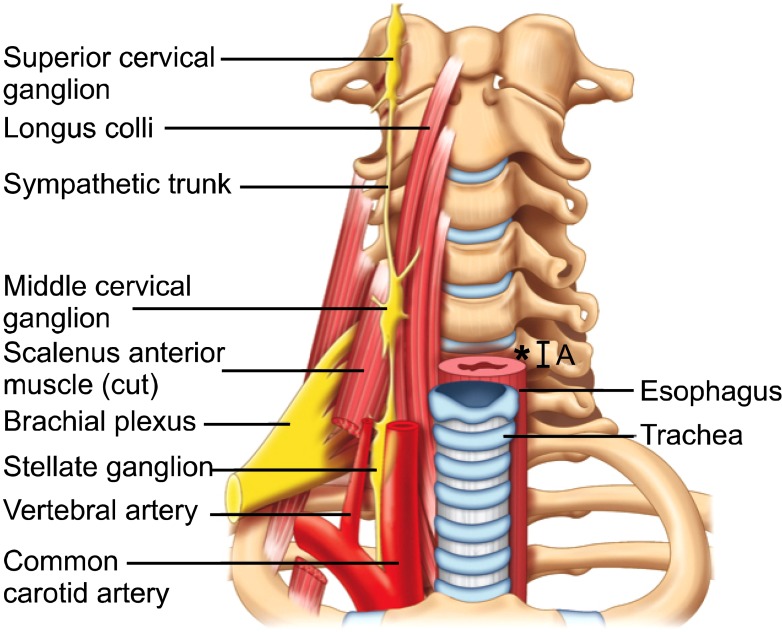
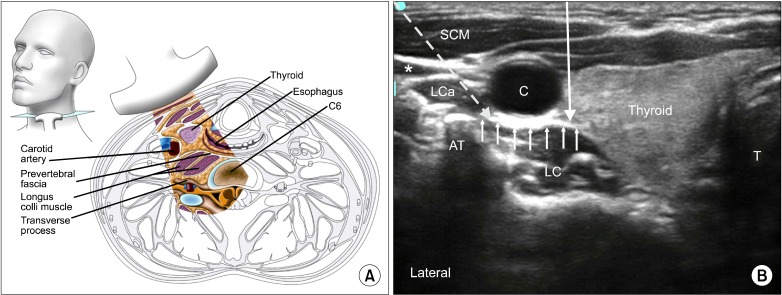
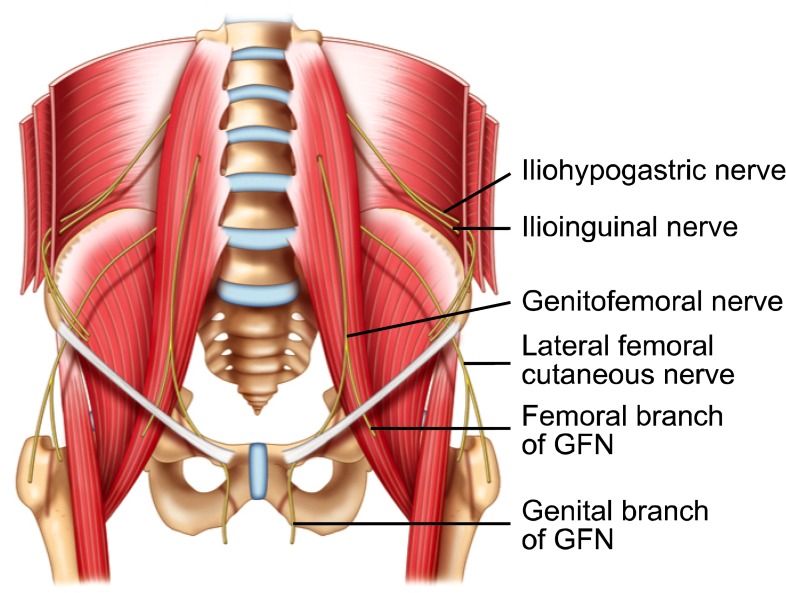
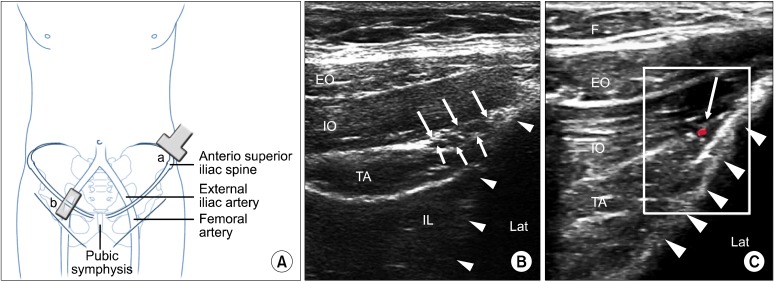
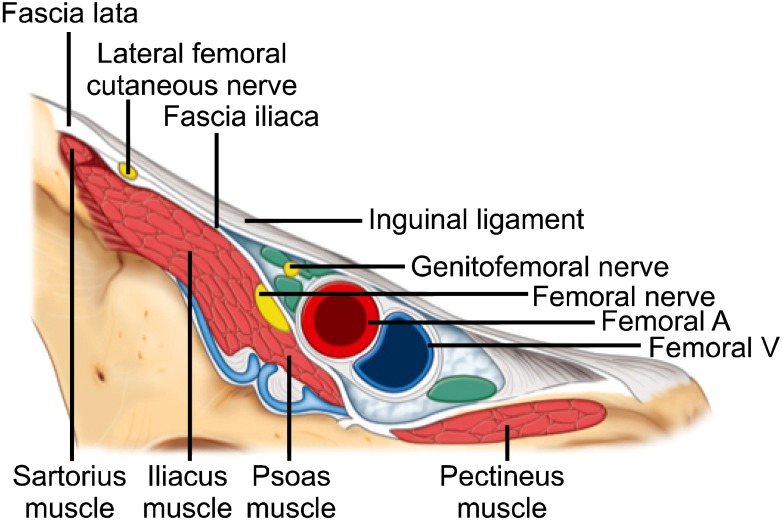
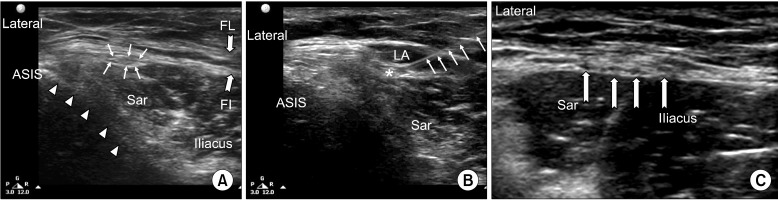
- Ultrasound has emerged to become a commonly used modality in the performance of chronic pain interventions. It allows direct visualization of tissue structure while allowing real time guidance of needle placement and medication administration. Ultrasound is a relatively affordable imaging tool and does not subject the practitioner or patient to radiation exposure. This review focuses on the anatomy and sonoanatomy of peripheral non-axial structures commonly involved in chronic pain conditions including the stellate ganglion, suprascapular, ilioinguinal, iliohypogastric, genitofemoral and lateral femoral cutaneous nerves. Additionally, the review discusses ultrasound guided intervention techniques applicable to these structures.
Keyword
Figure
Cited by 5 articles
-
Sonoanatomic Variation of Pes Anserine Bursa
Farnad Imani, Poupak Rahimzadeh, Farid Abolhasan Gharehdag, Seyed Hamid Reza Faiz
Korean J Pain. 2013;26(3):249-254. doi: 10.3344/kjp.2013.26.3.249.Ultrasound Guided Transversus Abdominis Plane Block for Anterior Cutaneous Nerve Entrapment Syndrome
Rajendra Kumar Sahoo, Abhijit S. Nair
Korean J Pain. 2015;28(4):284-286. doi: 10.3344/kjp.2015.28.4.284.A pictorial review of signature patterns living in musculoskeletal ultrasonography
Su Young Kim, Ji Hyun Cheon, Won Jun Seo, Geun Young Yang, Yun Mi Choi, Kyung Hoon Kim
Korean J Pain. 2016;29(4):217-228. doi: 10.3344/kjp.2016.29.4.217.A randomized, open labeled study comparing the serum levels of cobalamin after three doses of 500 mcg vs. a single dose methylcobalamin of 1500 mcg in patients with peripheral neuropathy
Amrita Sil, Hrishikesh Kumar, Rahul Deb Mondal, Sidharth Sankar Anand, Anirban Ghosal, Ashis Datta, Sandesh V Sawant, Vaibhavi Kapatkar, Ganesh Kadhe, Sameer Rao
Korean J Pain. 2018;31(3):183-190. doi: 10.3344/kjp.2018.31.3.183.The use of sonographic guidance in caudal epidural steroid injections
Emanuele Piraccini, Giovanni Musetti, Helen Byrne, Stefano Maitan
Korean J Pain. 2018;31(4):305-306. doi: 10.3344/kjp.2018.31.4.305.
Reference
-
1. Manchikanti L, Boswell MV, Singh V, Benyamin RM, Fellows B, Abdi S, et al. Comprehensive evidence-based guidelines for interventional techniques in the management of chronic spinal pain. Pain Physician. 2009; 12:699–802. PMID: 19644537.2. Davros WJ. Fluoroscopy: basic science, optimal use, and patient/operator protection. Tech Reg Anesth Pain Manag. 2007; 11:44–54.
Article3. Suk JI, Walker FO, Cartwright MS. Ultrasonography of peripheral nerves. Curr Neurol Neurosci Rep. 2013; 13:328. PMID: 23314937.
Article4. Bouffard JA, Lee SM, Dhanju J. Ultrasonography of the shoulder. Semin Ultrasound CT MR. 2000; 21:164–191. PMID: 10994687.
Article5. Martinoli C, Bianchi S, Gandolfo N, Valle M, Simonetti S, Derchi LE. US of nerve entrapments in osteofibrous tunnels of the upper and lower limbs. Radiographics. 2000; 20 Spec No:S199–S213. PMID: 11046171.
Article6. Bianchi S, Martinoli C, Bianchi-Zamorani M, Valle M. Ultrasound of the joints. Eur Radiol. 2002; 12:56–61. PMID: 11868074.
Article7. Barrington MJ, Wong DM, Slater B, Ivanusic JJ, Ovens M. Ultrasound-guided regional anesthesia: how much practice do novices require before achieving competency in ultrasound needle visualization using a cadaver model. Reg Anesth Pain Med. 2012; 37:334–339. PMID: 22354107.8. Aeschbach A, Mekhail NA. Common nerve blocks in chronic pain management. Anesthesiol Clin North America. 2000; 18:429–459. PMID: 10935018.
Article9. Lipov EG, Joshi JR, Sanders S, Wilcox K, Lipov S, Xie H, et al. Effects of stellate-ganglion block on hot flushes and night awakenings in survivors of breast cancer: a pilot study. Lancet Oncol. 2008; 9:523–532. PMID: 18485819.
Article10. Mulvaney SW, McLean B, de Leeuw J. The use of stellate ganglion block in the treatment of panic/anxiety symptoms with combat-related post-traumatic stress disorder; preliminary results of long-term follow-up: a case series. Pain Pract. 2010; 10:359–365. PMID: 20412504.
Article11. Elias M. Cervical sympathetic and stellate ganglion blocks. Pain Physician. 2000; 3:294–304. PMID: 16906187.
Article12. Kakazu CZ, Julka I. Stellate ganglion blockade for acute postoperative upper extremity pain. Anesthesiology. 2005; 102:1288–1289. PMID: 15915052.
Article13. Bhatia A, Flamer D, Peng PW. Evaluation of sonoanatomy relevant to performing stellate ganglion blocks using anterior and lateral simulated approaches: an observational study. Can J Anaesth. 2012; 59:1040–1047. PMID: 22956268.
Article14. Matula C, Trattnig S, Tschabitscher M, Day JD, Koos WT. The course of the prevertebral segment of the vertebral artery: anatomy and clinical significance. Surg Neurol. 1997; 48:125–131. PMID: 9242236.
Article15. Siegenthaler A, Mlekusch S, Schliessbach J, Curatolo M, Eichenberger U. Ultrasound imaging to estimate risk of esophageal and vascular puncture after conventional stellate ganglion block. Reg Anesth Pain Med. 2012; 37:224–227. PMID: 22157739.
Article16. Smith KJ, Ladak S, Choi PT, Dobranowski J. The cricoid cartilage and the esophagus are not aligned in close to half of adult patients. Can J Anaesth. 2002; 49:503–507. PMID: 11983669.
Article17. Smith KJ, Dobranowski J, Yip G, Dauphin A, Choi PT. Cricoid pressure displaces the esophagus: an observational study using magnetic resonance imaging. Anesthesiology. 2003; 99:60–64. PMID: 12826843.
Article18. Narouze S, Vydyanathan A, Patel N. Ultrasound-guided stellate ganglion block successfully prevented esophageal puncture. Pain Physician. 2007; 10:747–752. PMID: 17987096.19. Kapral S, Krafft P, Gosch M, Fleischmann D, Weinstabl C. Ultrasound imaging for stellate ganglion block: direct visualization of puncture site and local anesthetic spread. A pilot study. Reg Anesth. 1995; 20:323–328. PMID: 7577781.20. Shibata Y, Fujiwara Y, Komatsu T. A new approach of ultrasound-guided stellate ganglion block. Anesth Analg. 2007; 105:550–551. PMID: 17646541.
Article21. Christie JM, Martinez CR. Computerized axial tomography to define the distribution of solution after stellate ganglion nerve block. J Clin Anesth. 1995; 7:306–311. PMID: 7546757.
Article22. Janik JE, Hoeft MA, Ajar AH, Alsofrom GF, Borrello MT, Rathmell JP. Variable osteology of the sixth cervical vertebra in relation to stellate ganglion block. Reg Anesth Pain Med. 2008; 33:102–108. PMID: 18299089.
Article23. Narouze S. Beware of the "serpentine" inferior thyroid artery while performing stellate ganglion block. Anesth Analg. 2009; 109:289–290. PMID: 19535728.
Article24. Peng PW, Narouze S. Ultrasound-guided interventional procedures in pain medicine: a review of anatomy, sonoanatomy, and procedures: part I: nonaxial structures. Reg Anesth Pain Med. 2009; 34:458–474. PMID: 19920421.
Article25. Wertheim HM, Rovenstine EA. Suprascapular nerve block. Anesthesiology. 1941; 2:541–545.
Article26. Emery P, Bowman S, Wedderburn L, Grahame R. Suprascapular nerve block for chronic shoulder pain in rheumatoid arthritis. BMJ. 1989; 299:1079–1080. PMID: 2511970.
Article27. Jones DS, Chattopadhyay C. Suprascapular nerve block for the treatment of frozen shoulder in primary care: a randomized trial. Br J Gen Pract. 1999; 49:39–41. PMID: 10622015.28. Karataş GK, Meray J. Suprascapular nerve block for pain relief in adhesive capsulitis: comparison of 2 different techniques. Arch Phys Med Rehabil. 2002; 83:593–597. PMID: 11994796.
Article29. Shanahan EM, Ahern M, Smith M, Wetherall M, Bresnihan B, FitzGerald O. Suprascapular nerve block (using bupivacaine and methylprednisolone acetate) in chronic shoulder pain. Ann Rheum Dis. 2003; 62:400–406. PMID: 12695149.
Article30. Gleeson AP, Graham CA, Jones I, Beggs I, Nutton RW. Comparison of intra-articular lignocaine and a suprascapular nerve block for acute anterior shoulder dislocation. Injury. 1997; 28:141–142. PMID: 9205582.
Article31. Ritchie ED, Tong D, Chung F, Norris AM, Miniaci A, Vairavanathan SD. Suprascapular nerve block for postoperative pain relief in arthroscopic shoulder surgery: a new modality? Anesth Analg. 1997; 84:1306–1312. PMID: 9174311.
Article32. Neal JM, McDonald SB, Larkin KL, Polissar NL. Suprascapular nerve block prolongs analgesia after nonarthroscopic shoulder surgery but does not improve outcome. Anesth Analg. 2003; 96:982–986. PMID: 12651646.
Article33. Romeo AA, Rotenberg DD, Bach BR Jr. Suprascapular neuropathy. J Am Acad Orthop Surg. 1999; 7:358–367. PMID: 11497489.
Article34. Natsis K, Totlis T, Tsikaras P, Appell HJ, Skandalakis P, Koebke J. Proposal for classification of the suprascapular notch: a study on 423 dried scapulas. Clin Anat. 2007; 20:135–139. PMID: 16838269.
Article35. Peng PW, Wiley MJ, Liang J, Bellingham GA. Ultrasound-guided suprascapular nerve block: a correlation with fluoroscopic and cadaveric findings. Can J Anaesth. 2010; 57:143–148. PMID: 20052627.
Article36. Feigl GC, Anderhuber F, Dorn C, Pipam W, Rosmarin W, Likar R. Modified lateral block of the suprascapular nerve: a safe approach and how much to inject? A morphological study. Reg Anesth Pain Med. 2007; 32:488–494. PMID: 18035294.
Article37. Mallon WJ, Brown HR, Vogler JB 3rd, Martinez S. Radiographic and geometric anatomy of the scapula. Clin Orthop Relat Res. 1992; (277):142–154. PMID: 1555335.
Article38. Shah RV, Racz GB. Pulsed mode radiofrequency lesioning of the suprascapular nerve for the treatment of chronic shoulder pain. Pain Physician. 2003; 6:503–506. PMID: 16871304.39. Schneider-Kolsky ME, Pike J, Connell DA. CT-guided suprascapular nerve blocks: a pilot study. Skeletal Radiol. 2004; 33:277–282. PMID: 14872290.
Article40. Moore DC. Thomas CC, editor. Block of the suprascapular nerve. Regional nerve block. 1979. 4th ed. Springfield, IL: Charles C Thomas Publisher LTD;p. 300–303.41. Gofeld M. Ultrasonography in pain medicine: a critical review. Pain Pract. 2008; 8:226–240. PMID: 18513228.
Article42. Harmon D, Hearty C. Ultrasound-guided suprascapular nerve block technique. Pain Physician. 2007; 10:743–746. PMID: 17987095.43. Yücesoy C, Akkaya T, Ozel O, Cömert A, Tüccar E, Bedirli N, et al. Ultrasonographic evaluation and morphometric measurements of the suprascapular notch. Surg Radiol Anat. 2009; 31:409–414. PMID: 19142560.
Article44. Siegenthaler A, Moriggl B, Mlekusch S, Schliessbach J, Haug M, Curatolo M, et al. Ultrasound-guided suprascapular nerve block, description of a novel supraclavicular approach. Reg Anesth Pain Med. 2012; 37:325–328. PMID: 22222688.
Article45. Rab M, Ebmer J, Dellon AL. Anatomic variability of the ilioinguinal and genitofemoral nerve: implications for the treatment of groin pain. Plast Reconstr Surg. 2001; 108:1618–1623. PMID: 11711938.
Article46. Alfieri S, Rotondi F, Di Giorgio A, Fumagalli U, Salzano A, Di Miceli D, et al. Influence of preservation versus division of ilioinguinal, iliohypogastric, and genital nerves during open mesh herniorrhaphy: prospective multicentric study of chronic pain. Ann Surg. 2006; 243:553–558. PMID: 16552209.
Article47. Whiteside JL, Barber MD, Walters MD, Falcone T. Anatomy of ilioinguinal and iliohypogastric nerves in relation to trocar placement and low transverse incisions. Am J Obstet Gynecol. 2003; 189:1574–1578. PMID: 14710069.
Article48. Seid AS, Amos E. Entrapment neuropathy in laparoscopic herniorrhaphy. Surg Endosc. 1994; 8:1050–1053. PMID: 7992173.
Article49. Brandsborg B, Nikolajsen L, Kehlet H, Jensen TS. Chronic pain after hysterectomy. Acta Anaesthesiol Scand. 2008; 52:327–331. PMID: 18269384.
Article50. Aasvang E, Kehlet H. Chronic postoperative pain: the case of inguinal herniorrhaphy. Br J Anaesth. 2005; 95:69–76. PMID: 15531621.
Article51. Mandelkow H, Loeweneck H. The iliohypogastric and ilioinguinal nerves. Distribution in the abdominal wall, danger areas in surgical incisions in the inguinal and pubic regions and reflected visceral pain in their dermatomes. Surg Radiol Anat. 1988; 10:145–149. PMID: 2969627.52. al-dabbagh AK. Anatomical variations of the inguinal nerves and risks of injury in 110 hernia repairs. Surg Radiol Anat. 2002; 24:102–107. PMID: 12197017.
Article53. Liu WC, Chen TH, Shyu JF, Chen CH, Shih C, Wang JJ, et al. Applied anatomy of the genital branch of the genitofemoral nerve in open inguinal herniorrhaphy. Eur J Surg. 2002; 168:145–149. PMID: 12182238.
Article54. Katz J. Atlas of regional anesthesia. 1985. Norwalk, CT: Appleton-Century-Crofts.55. Brown D. Atlas of regional anesthesia. 1999. Philadelphia, PA: WB Saunders.56. van Schoor AN, Boon JM, Bosenberg AT, Abrahams PH, Meiring JH. Anatomical considerations of the pediatric ilioinguinal/iliohypogastric nerve block. Paediatr Anaesth. 2005; 15:371–377. PMID: 15828987.
Article57. Weintraud M, Marhofer P, Bösenberg A, Kapral S, Willschke H, Felfernig M, et al. Ilioinguinal/iliohypogastric blocks in children: where do we administer the local anesthetic without direct visualization? Anesth Analg. 2008; 106:89–93. PMID: 18165559.
Article58. Ghani KR, McMillan R, Paterson-Brown S. Transient femoral nerve palsy following ilio-inguinal nerve blockade for day case inguinal hernia repair. J R Coll Surg Edinb. 2002; 47:626–629. PMID: 12363189.59. Jöhr M, Sossai R. Colonic puncture during ilioinguinal nerve block in a child. Anesth Analg. 1999; 88:1051–1052. PMID: 10320167.
Article60. Amory C, Mariscal A, Guyot E, Chauvet P, Leon A, Poli-Merol ML. Is ilioinguinal/iliohypogastric nerve block always totally safe in children? Paediatr Anaesth. 2003; 13:164–166. PMID: 12562490.
Article61. Vaisman J. Pelvic hematoma after an ilioinguinal nerve block for orchialgia. Anesth Analg. 2001; 92:1048–1049. PMID: 11273948.
Article62. Waldman SD. Atlas of interventional pain management. 2004. 2nd ed. Philadelphia, PA: Saunders.63. Eichenberger U, Greher M, Kirchmair L, Curatolo M, Moriggl B. Ultrasound-guided blocks of the ilioinguinal and iliohypogastric nerve: accuracy of a selective new technique confirmed by anatomical dissection. Br J Anaesth. 2006; 97:238–243. PMID: 16698865.
Article64. Hu P, Harmon D, Frizelle H. Ultrasound guidance for ilioinguinal/iliohypogastric nerve block: a pilot study. Ir J Med Sci. 2007; 176:111–115. PMID: 17570011.
Article65. Gofeld M, Christakis M. Sonographically guided ilioinguinal nerve block. J Ultrasound Med. 2006; 25:1571–1575. PMID: 17121952.
Article66. Gucev G, Yasui GM, Chang TY, Lee J. Bilateral ultrasound-guided continuous ilioinguinal-iliohypogastric block for pain relief after cesarean delivery. Anesth Analg. 2008; 106:1220–1222. PMID: 18349197.
Article67. Jamieson RW, Swigart LL, Anson BJ. Points of parietal perforation of the ilioinguinal and iliohypogastric nerves in relation to optimal sites for local anaesthesia. Q Bull Northwest Univ Med Sch. 1952; 26:22–26. PMID: 14912259.68. Peng PW, Tumber PS. Ultrasound-guided interventional procedures for patients with chronic pelvic pain - a description of techniques and review of literature. Pain Physician. 2008; 11:215–224. PMID: 18354713.69. Grossman MG, Ducey SA, Nadler SS, Levy AS. Meralgia paresthetica: diagnosis and treatment. J Am Acad Orthop Surg. 2001; 9:336–344. PMID: 11575913.
Article70. Harney D, Patijn J. Meralgia paresthetica: diagnosis and management strategies. Pain Med. 2007; 8:669–677. PMID: 18028045.
Article71. Shannon J, Lang SA, Yip RW, Gerard M. Lateral femoral cutaneous nerve block revisited. A nerve stimulator technique. Reg Anesth. 1995; 20:100–104. PMID: 7605755.72. Dias Filho LC, Valença MM, Guimarães Filho FA, Medeiros RC, Silva RA, Morais MG, et al. Lateral femoral cutaneous neuralgia: an anatomical insight. Clin Anat. 2003; 16:309–316. PMID: 12794914.
Article73. de Ridder VA, de Lange S, Popta JV. Anatomical variations of the lateral femoral cutaneous nerve and the consequences for surgery. J Orthop Trauma. 1999; 13:207–211. PMID: 10206253.
Article74. Ropars M, Morandi X, Huten D, Thomazeau H, Berton E, Darnault P. Anatomical study of the lateral femoral cutaneous nerve with special reference to minimally invasive anterior approach for total hip replacement. Surg Radiol Anat. 2009; 31:199–204. PMID: 18982237.
Article75. Grothaus MC, Holt M, Mekhail AO, Ebraheim NA, Yeasting RA. Lateral femoral cutaneous nerve: an anatomic study. Clin Orthop Relat Res. 2005; (437):164–168. PMID: 16056045.76. Aszmann OC, Dellon ES, Dellon AL. Anatomical course of the lateral femoral cutaneous nerve and its susceptibility to compression and injury. Plast Reconstr Surg. 1997; 100:600–604. PMID: 9283556.
Article77. Murata Y, Takahashi K, Yamagata M, Shimada Y, Moriya H. The anatomy of the lateral femoral cutaneous nerve, with special reference to the harvesting of iliac bone graft. J Bone Joint Surg Am. 2000; 82:746–747. PMID: 10819285.
Article78. Patel NJ, Flashburg MH, Paskin S, Grossman R. A regional anesthetic technique compared to general anesthesia for outpatient knee arthroscopy. Anesth Analg. 1986; 65:185–187. PMID: 3942307.79. Hopkins PM, Ellis FR, Halsall PJ. Evaluation of local anaesthetic blockade of the lateral femoral cutaneous nerve. Anaesthesia. 1991; 46:95–96. PMID: 1872458.
Article80. Ng I, Vaghadia H, Choi PT, Helmy N. Ultrasound imaging accurately identifies the lateral femoral cutaneous nerve. Anesth Analg. 2008; 107:1070–1074. PMID: 18713931.
Article81. Bodner G, Bernathova M, Galiano K, Putz D, Martinoli C, Felfernig M. Ultrasound of the lateral femoral cutaneous nerve: normal findings in a cadaver and in volunteers. Reg Anesth Pain Med. 2009; 34:265–268. PMID: 19587628.82. Hurdle MF, Weingarten TN, Crisostomo RA, Psimos C, Smith J. Ultrasound-guided blockade of the lateral femoral cutaneous nerve: technical description and review of 10 cases. Arch Phys Med Rehabil. 2007; 88:1362–1364. PMID: 17908585.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ultrasound Guided Therapeutic Medial Branch Block for the Facet Joint Pain
- Ultrasound-guided interventions for spinal pain
- Ultrasound Guided Nerve Block at Vertebra and Lower Extremity
- Ultrasound-guided interventions for controlling the thoracic spine and chest wall pain: a narrative review
- Endoscopic ultrasound-guided vascular interventions: An overview of current and emerging techniques