J Adv Prosthodont.
2015 Feb;7(1):76-84. 10.4047/jap.2015.7.1.76.
The path of placement of a removable partial denture: a microscope based approach to survey and design
- Affiliations
-
- 1Private Practice, Manalapan, NJ, USA. mamounjo@gmail.com
- KMID: 1974895
- DOI: http://doi.org/10.4047/jap.2015.7.1.76
Abstract
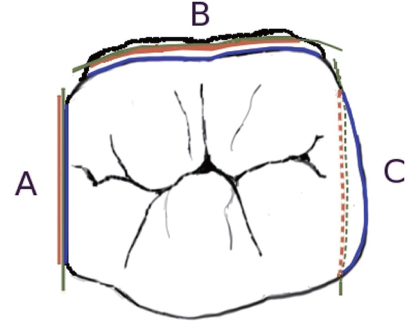
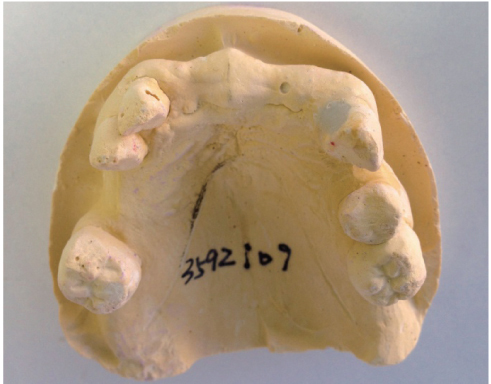
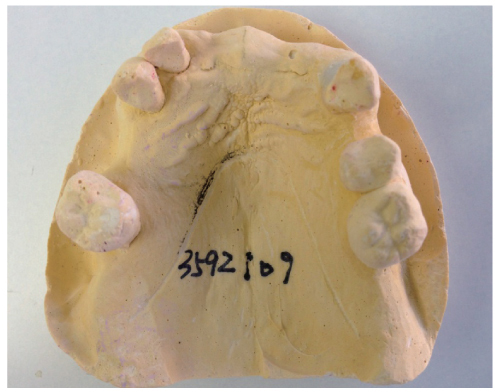
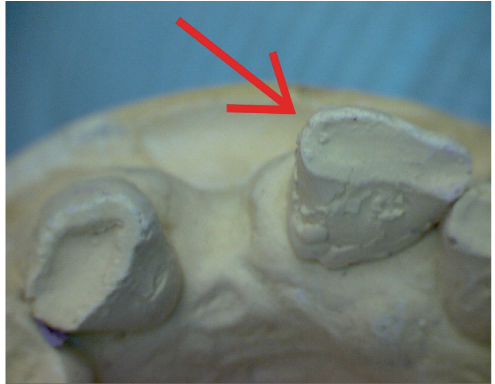
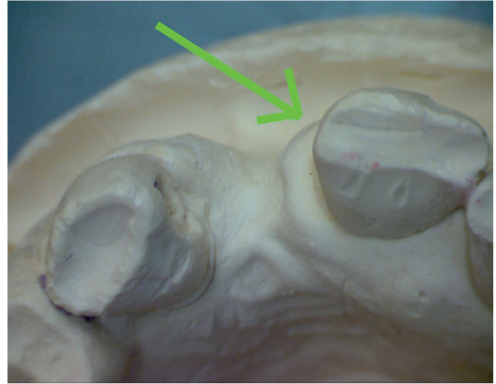
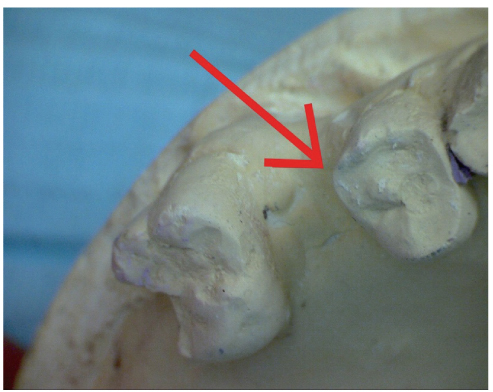
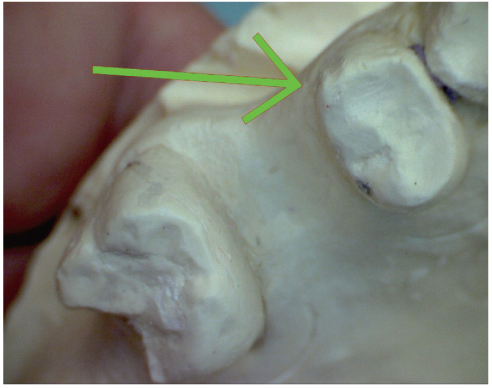
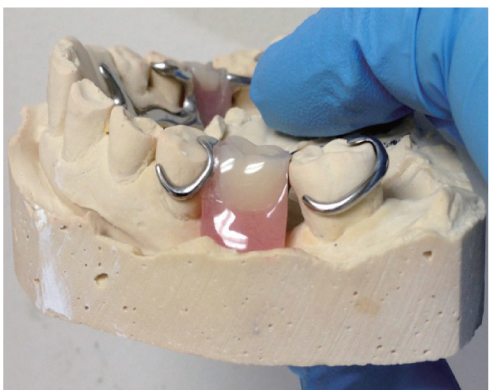
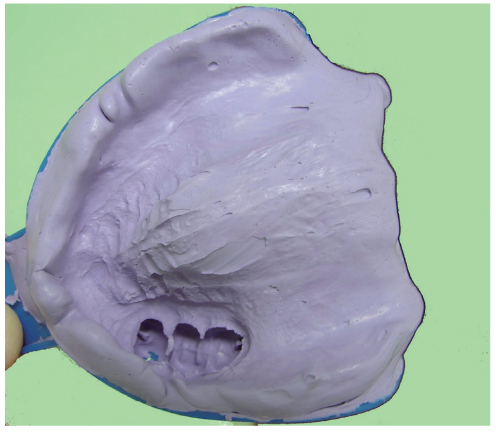
- This article reviews the topic of how to identify and develop a removable partial denture (RPD) path of placement, and provides a literature review of the concept of the RPD path of placement, also known as the path of insertion. An optimal RPD path of placement, guided by mutually parallel guide planes, ensures that the RPD flanges fit intimately over edentulous ridge structures and that the framework fits intimately with guide plane surfaces, which prevents food collecting empty spaces between the intaglio surface of the framework and intraoral surfaces, and ensures that RPD clasps engage adequate numbers of tooth undercuts to ensure RPD retention. The article covers topics such as the causes of obstructions to RPD intra-oral seating, the causes of food collecting empty spaces that may exist around an RPD, and how to identify if a guide plane is parallel with the projected RPD path of placement. The article presents a method of using a surgical operating microscope, or high magnification (6-8x or greater) binocular surgical loupes telescopes, combined with co-axial illumination, to identify a preliminary path of placement for an arch. This preliminary path of placement concept may help to guide a dentist or a dental laboratory technician when surveying a master cast of the arch to develop an RPD path of placement, or in verifying that intra-oral contouring has aligned teeth surfaces optimally with the RPD path of placement. In dentistry, a well-fitting RPD reduces long-term periodontal or structural damage to abutment teeth.
Keyword
MeSH Terms
Figure
Reference
-
1. The glossary of prosthodontic terms. J Prosthet Dent. 2005; 94:10–92.2. Carreiro Ada F, Machado AL, Giampaolo ET, Santana IL, Vergani CE. Dual path: a concept to improve the esthetic replacement of missing anterior teeth with a removable partial denture. J Prosthodont. 2008; 17:586–590.3. Krol AJ, Finzen FC. Rotational path removable partial dentures: Part 1. Replacement of posterior teeth. Int J Prosthodont. 1988; 1:17–27.4. Krol AJ, Finzen FC. Rotational path removable partial dentures: Part 2. Replacement of anterior teeth. Int J Prosthodont. 1988; 1:135–142.5. Jacobson TE, Krol AJ. Rotational path removable partial denture design. J Prosthet Dent. 1982; 48:370–376.6. Suh JS, Billy EJ. Rotational path removable partial denture (RPD): conservative esthetic treatment option for the edentulous mandibular anterior region: a case report. J Esthet Restor Dent. 2008; 20:98–105.7. Baharav H, Ben-Ur Z, Laufer BZ, Cardash HS. Removable partial denture with a lateral rotational path of insertion. Quintessence Int. 1995; 26:531–533.8. Carr AB, Borwn DT, McCracken WL. McCracken's removable partial prosthodontics. 12th ed.St. Louis, Mo.: Elsevier Mosby;2011.9. Stratton RJ, Wiebelt FJ. An atlas of removable partial denture design. Chicago: Quintessence Pub. Co.;1988.10. Davenport JC, Basker RM, Heath JR, Ralph JP, Glantz PO. The removable partial denture equation. Br Dent J. 2000; 189:414–424.11. Davenport JC, Basker RM, Heath JR, Ralph JP, Glantz PO, Hammond P. Tooth preparation. Br Dent J. 2001; 190:288–294.12. Mamoun JS. A rationale for the use of high-powered magnification or microscopes in general dentistry. Gen Dent. 2009; 57:18–26.13. van As G. Magnification and the alternatives for microdentistry. Compend Contin Educ Dent. 2001; 22:1008–1012. 1014–1016.14. Napoletano D. Dental Operating Microscopes: Don't Equip an Operatory Without One. Inside Dent. 2007; 3(5):Available form: http://www.dentalaegis.com/id/2007/05/dental-operating-microscopes-do-not-equip-an-operatory-without-one.15. Owall B, Budtz-Jörgensen E, Davenport J, Mushimoto E, Palmqvist S, Renner R, Sofou A, Wöstmann B. Removable partial denture design: a need to focus on hygienic principles? Int J Prosthodont. 2002; 15:371–378.16. Rudd RW, Bange AA, Rudd KD, Montalvo R. Preparing teeth to receive a removable partial denture. J Prosthet Dent. 1999; 82:536–549.17. Bezzon OL, Mattos MG, Ribeiro RF. Surveying removable partial dentures: the importance of guiding planes and path of insertion for stability. J Prosthet Dent. 1997; 78:412–418.18. Zarb G, Watson RM, Hobkirk J. Guide planes. In : In : Bates JF, Neill DJ, Preiskel HW, editors. Restoration of the Partially Dentate Mouth. Proceedings of the International Prosthodontic Symposium of 1982; London: Quintessence;1984. p. 193–201.19. Waghorn S, Kuzmanovic DV. Technique for preparation of parallel guiding planes for removable partial dentures. J Prosthet Dent. 2004; 92:200–201.20. Mamoun J. Preparing fixed partial denture abutments such that they provide a path of placement free of undercuts. Gen Dent. 2012; 60:519–525.21. Bennani V, Shahmiri R. A simple method to transfer the selected path of insertion of a removable partial denture intraorally. J Prosthet Dent. 2009; 101:73–74.22. Burns DR, Unger JW. The construction of crowns for removable partial denture abutment teeth. Quintessence Int. 1994; 25:471–475.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A photoelastic study on the stress analysis under mandibular distal-extension removable partial denture with different design of the major connector
- Clinical application of mandibular removable partial denture using implant-supported surveyed crown: A case report
- A PHOTOELASTIC ANALYSIS ON TOOTH SUPPORTING STRUCTURE AND RESIDUAL RIDGE ACCORDING TO DENTURE DESIGN FOR REMAINING MANDIBULAR CANINES
- STRESS ANALYSIS AT SUPPORTING TISSUE OF ABUTMENT TEETH AND RESIDUAL RIDGE ACCORDING TO DENTURE DESIGN WITH REMAINING UNILATERAL POSTERIOR TEETH
- Implant-assisted removable partial denture using digital guide surgery in partially edentulous mandible: A case report