Clin Exp Otorhinolaryngol.
2015 Mar;8(1):7-12. 10.3342/ceo.2015.8.1.7.
Single-Center 10-Year Experience in Treating Patients With Vascular Tinnitus: Diagnostic Approaches and Treatment Outcomes
- Affiliations
-
- 1Department of Otorhinolaryngology-Head and Neck Surgery, College of Medicine, The Catholic University of Korea, Seoul, Korea. snparkmd@catholic.ac.kr sypak@catholic.ac.kr
- KMID: 1973481
- DOI: http://doi.org/10.3342/ceo.2015.8.1.7
Abstract
OBJECTIVES
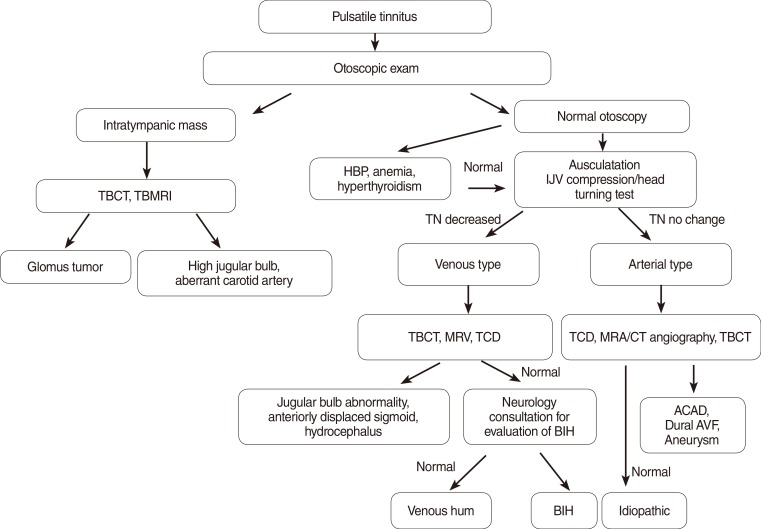
Vascular tinnitus is the most common form of pulsatile tinnitus, particularly when the tinnitus corresponds with the pulse of patients. In this study, we reviewed the 10-year clinical data on vascular tinnitus of our tinnitus clinic to investigate the frequency of the underlying etiologies, to introduce a diagnostic protocol, and to evaluate the treatment outcomes.
METHODS
We retrospectively collected the data of 57 patients who were diagnosed as vascular tinnitus between April 2001 and December 2011. Careful history taking, otoscopy, thorough physical examinations, audiometry, laboratory tests, as well as radiologic examinations were performed according to our diagnostic protocol to find the origin of pulsatile tinnitus. Treatment options were individualized based on the specific etiology, and the outcomes were assessed using patient's subjective reports at the follow-up interviews.
RESULTS
High jugular bulb was the most common cause (47.4%) of vascular tinnitus, and venous hum was the next (17.5%). Dural arteriovenous fistula, intracranial aneurysm, atherosclerotic carotid artery disease, and hypertension were less common causes. Vascular tinnitus was alleviated in most patients after the appropriate treatment: surgical intervention, tinnitus retraining therapy, reassurance, and medications.
CONCLUSION
Vascular tinnitus can be successfully diagnosed by the regular use of the suggested protocol. Many patients with vascular tinnitus have treatable underlying etiologies. Treatment of those etiologies or at least counseling about the tinnitus itself can benefit the patients with troublesome vascular tinnitus.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Tinnitus: Overview
Chul Won Park
Hanyang Med Rev. 2016;36(2):79-80. doi: 10.7599/hmr.2016.36.2.79.Objective Tinnitus
Shi Nae Park
Hanyang Med Rev. 2016;36(2):99-108. doi: 10.7599/hmr.2016.36.2.99.
Reference
-
1. Stouffer JL, Tyler RS. Characterization of tinnitus by tinnitus patients. J Speech Hear Disord. 1990; 8. 55(3):439–453. PMID: 2381186.
Article2. Liyanage SH, Singh A, Savundra P, Kalan A. Pulsatile tinnitus. J Laryngol Otol. 2006; 2. 120(2):93–97. PMID: 16359136.
Article3. Sismanis A. Pulsatile tinnitus: A 15-year experience. Am J Otol. 1998; 7. 19:472–477. PMID: 9661757.4. Durcan FJ, Corbett JJ, Wall M. The incidence of pseudotumour cerebri: Population studies in Iowa and Louisiana. Arch Neurol. 1988; 8. 45(8):875–877. PMID: 3395261.5. Radhakrishnan K, Thacker AK, Bohlaga NH, Maloo JC, Gerryo SE. Epidemiology of idiopathic intracranial hypertension: a prospective and case-control study. J Neurol Sci. 1993; 5. 116(1):18–28. PMID: 8509801.
Article6. Overton SB, Ritter FN. A high placed jugular bulb in the middle ear: a clinical and temporal bone study. Laryngoscope. 1973; 12. 83(12):1986–1991. PMID: 4772103.
Article7. Subotic R. The high position of jugular bulb. Acta Otolaryngol. 1979; Mar-Apr. 87(3-4):340–344. PMID: 443015.8. Weiss RL, Zahtz G, Goldofsky E, Parnes H, Shikowitz MJ. High jugular bulb and conductive hearing loss. Laryngoscope. 1997; 3. 107(3):321–327. PMID: 9121306.
Article9. Yoo HJ, Park SN, Kim DK, Park KH, Kim MJ, Kim JE. Incidence and clinical characteristics of patients with tinnitus according to diagnostic classification. Korean J Otorhinolaryngol-Head Neck Surg. 2011; 6. 54(6):392–398.
Article10. Huang BR, Wang CH, Young YH. Dehiscent high jugular bulb: a pitfall in middle ear surgery. Otol Neurotol. 2006; 10. 27(7):923–927. PMID: 16788425.11. Buckwalter JA, Sasaki CT, Viraponse C. Pulsatile tinnitus arising from jugular megabulb deformity: a treatment rationale. Laryngoscope. 1983; 12. 93(12):1534–1539. PMID: 6645753.
Article12. Yoon BN, Lee TH, Kong SK. Management of high jugular bulb with tinnitus: transvenous stent-assisted coil embolization. Otolaryngol Head Neck Surg. 2008; 11. 139(5):740–741. PMID: 18984278.
Article13. Couloigner V, Grayeli AB, Bouccara D, Julien N, Sterkers O. Surgical treatment of the high jugular bulb in patients with Meniere's disease and pulsatile tinnitus. Eur Arch Otorhinolaryngol. 1999; 256(5):224–229. PMID: 10392295.14. Kondoh K, Kitahara T, Mishiro Y, Okumura S, Kubo T. Management of hemorrhagic high jugular bulb with adhesive otitis media in an only hearing ear: transcatheter endovascular embolization using detachable coils. Ann Otol Rhinol Laryngol. 2004; 12. 113(12):975–979. PMID: 15633900.
Article15. Arenberg IK, McCreary HS. Objective tinnitus aurium and dural arteriovenous malformations of the posterior fossa. Ann Otol Rhinol Laryngol. 1971; 2. 80(1):111–120. PMID: 5100337.
Article16. Chandler JR. Diagnosis and cure of venous hum tinnitus. Laryngoscope. 1983; 7. 93(7):892–895. PMID: 6865626.
Article17. Engstrom H, Graf W. On objective tinnitus and its recording. Acta Otolaryngol Suppl. 1950; 95:127–137. PMID: 14884974.
Article18. Hentzer E. Objective tinnitus of vascular type: A follow-up study. Acta Otolaryngol. 1968; 10. 66(4):273–281. PMID: 5734496.19. Piippo A, Laakso A, Seppa K, Rinne J, Jaaskelainen JE, Hernesniemi J, et al. Early and long-term excess mortality in 227 patients with intracranial dural arteriovenous fistulas. J Neurosurg. 2013; 7. 119(1):164–171. PMID: 23600937.
Article20. Hashimoto T, Meng H, Young WL. Intracranial aneurysms: Links among inflammation, hemodynamics and vascular remodeling. Neurol Res. 2006; 6. 28(4):372–380. PMID: 16759441.
Article21. Mizutani T, Kojima H, Asamoto S, Miki Y. Pathological mechanism and three-dimensional structure of cerebral dissecting aneurysms. J Neurosurg. 2001; 5. 94(5):712–717. PMID: 11354401.
Article22. Tulamo R, Frosen J, Hernesniemi J, Niemela M. Inflammatory changes in the aneurysm wall: a review. J Neurointerv Surg. 2010; 6. 2(2):120–130. PMID: 21990591.
Article23. Juvela S. Prevalence of risk factors for intracranial aneurysms. Lancet Neurol. 2011; 7. 10(7):595–597. PMID: 21641283.