Cancer Res Treat.
2009 Dec;41(4):205-210.
Biopsy Related Prostate Status Does Not Affect on the Clinicopathological Outcome of Robotic Assisted Laparoscopic Radical Prostatectomy
- Affiliations
-
- 1Department of Urology, MIS & Robotic Urologic Surgery Center, Korea University School of Medicine, Seoul, Korea. urokyh@naver.com
- 2Global Robotics Institute, University of Central Florida, Florida Hospital, Orlando, FL, USA.
Abstract
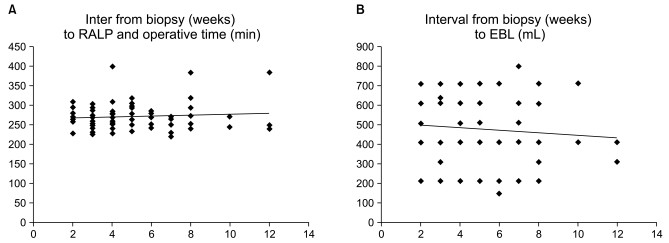
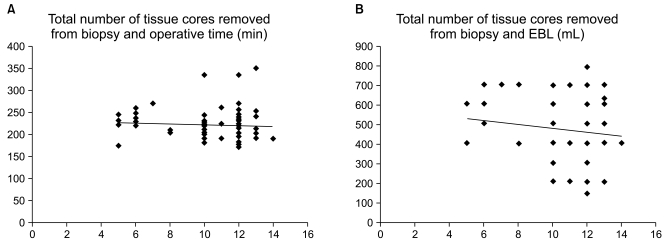
- PURPOSE
To determine whether the biopsy core number and time interval between prostate biopsy and radical prostatectomy affect the operative and oncologic outcome of robot assisted laparoscopic radical prostatectomy (RALP). MATERIALS AND METHODS: From January 2008 to April 2009, a single surgeon performed 72 RALPs after an initial learning period of 30 cases. The relationship between time from biopsy to prostatectomy and biopsy core number with operative time and estimated blood loss (EBL) were initially evaluated with a linear regression model. These patients were classified into groups according to whether the interval from biopsy to RALP was within four weeks or not, and whether there were less than or greater than 10 core specimens removed. RESULTS: RALP was performed in 34 patients within four weeks of biopsy, and in 38 patients more than 4 weeks after biopsy. According to the number of core specimens removed, less than 10 cores were performed in 10 patients, and more than 10 cores were performed in 62 patients. Using an interval of 4 weeks as the cutoff point, early surgery was associated with longer operating time (232.6 vs 208.8 min) and increased estimated blood loss (305.1 vs 276.9 mL). For cases with more than 10 biopsy cores, there was a slight increase in operative time (229.2 vs 210.3 min). None of these differences were statistically significant by multivariate analysis. CONCLUSION: Our data suggests that there is no reason to delay RALP to more than 4 weeks after prostate biopsy. It also revealed that the number of biopsy cores (up to 14) did not influence operative outcome. Thus, RALP is a feasible procedure regardless of the biopsy related prostate state.
Keyword
MeSH Terms
Figure
Reference
-
1. Joseph JV, Vicente I, Madeb R, Erturk E, Patel HR. Robot-assisted vs pure laparoscopic radical prostatectomy: are there any differences? BJU Int. 2005; 96:39–42. PMID: 15963117.
Article2. Nelson JB. Debate: Open radical prostatectomy vs. laparoscopic vs. robotic. Urol Oncol. 2007; 25:490–493. PMID: 18047958.
Article3. Sokoloff MH, Brendler CB. Indications and contraindications for nerve-sparing radical prostatectomy. Urol Clin North Am. 2001; 28:535–543. PMID: 11590812.
Article4. Menon M, Tewari A, Peabody JO, Shrivastava A, Kaul S, Bhandari A, et al. Vattikuti Institute prostatectomy, a technique of robotic radical prostatectomy for management of localized carcinoma of the prostate: experience of over 1100 cases. Urol Clin North Am. 2004; 31:701–717. PMID: 15474597.
Article5. Ban JH, Ko YH, Kang SH, Park HS, Cheon J. Learning curve with robotic-assisted laparoscopic radical prostatectomy: a prospective study. Korean J Urol. 2009; 50:140–147.
Article6. Beahrs OH, Henson DE, Hutter RVP, Kennedy BJ. American Joint Committee on Cancer. Manual for staging of cancer. 1992. 4th ed. Philadelphia: JB Lippincott;p. 239.7. Patel VR. Robotic Urologic Surgery. 2007. 1st ed. London: Springer;p. 81.8. Stolzenburg JU, Anderson C, Rabenalt R, Do M, Ho K, Truss MC. Endoscopic extraperitoneal radical prostatectomy in patients with prostate cancer and previous laparoscopic inguinal mesh placement for hernia repair. World J Urol. 2005; 23:295–299. PMID: 16133559.
Article9. Kaji Y, Kurhanewicz J, Hricak H, Sokolov DL, Huang LR, Nelson SJ, et al. Localizing prostate cancer in the presence of postbiopsy changes on MR images: role of proton MR spectroscopic imaging. Radiology. 1998; 206:785–790. PMID: 9494502.
Article10. Oesterling JE, Rice DC, Glenski WJ, Bergstralh EJ. Effect of cystoscopy, prostate biopsy, and transurethral resection of prostate on serum prostate-specific antigen concentration. Urology. 1993; 42:276–282. PMID: 7691013.
Article11. Lee DK, Allareddy V, O'donnell MA, Williams RD, Konety BR. Does the interval between prostate biopsy and radical prostatectomy affect the immediate postoperative outcome? BJU Int. 2006; 97:48–50. PMID: 16336327.
Article12. Eggener SE, Yossepowitch O, Serio AM, Vickers AJ, Scardino PT, Eastham JA. Radical prostatectomy shortly after prostate biopsy does not affect operative difficulty or efficacy. Urology. 2007; 69:1128–1133. PMID: 17572200.
Article13. Singh A, Fagin R, Shah G, Shekarriz B. Impact of prostate size and body mass index on perioperative morbidity after laparoscopic radical prostatectomy. J Urol. 2005; 173:552–554. PMID: 15643251.
Article14. Hsu EI, Hong EK, Lepor H. Influence of body weight and prostate volume on intraoperative, perioperative, and postoperative outcomes after radical retropubic prostatectomy. Urology. 2003; 61:601–606. PMID: 12639655.
Article15. Boorjian SA, Bianco FJ Jr, Scardino PT, Eastham JA. Does the time from biopsy to surgery affect biochemical recurrence after radical prostatectomy? BJU Int. 2005; 96:773–776. PMID: 16153197.16. Khan MA, Mangold LA, Epstein JI, et al. Impact of surgical delay on long-term cancer control for clinically localized prostate cancer. J Urol. 2004; 172:1835–1839. PMID: 15540733.
Article17. Presti JC Jr, Chang JJ, Bhargava V, Shinohara K. The optimal systematic prostate biopsy scheme should include 8 rather than 6 biopsies: results of a prospective clinical trial. J Urol. 2000; 163:163–166. PMID: 10604337.
Article18. Gore JL, Shariat SF, Miles BJ, Kadmon D, Jiang N, Wheeler TM, et al. Optimal combinations of systematic sextant and laterally directed biopsies for the detection of prostate cancer. J Urol. 2001; 165:1554–1559. PMID: 11342916.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Robot-Assisted Laparoscopic Radical Prostatectomy
- Radical Prostatectomy
- Changes in Patterns of Radical Prostatectomy due to Diffusion of Robotic Surgical System: A Nationwide Study Using Health Insurance Claims Data
- Two Different Surgical Approaches for Prostatic Stromal Sarcoma: Robot-Assisted Laparoscopic Radical Prostatectomy and Open Radical Cysto-Prostatectomy With Ileal Conduit
- A Case of Robot-Assisted Laparoscopic Radical Prostatectomy in Primary Small Cell Prostate Cancer