J Korean Soc Radiol.
2015 Aug;73(2):116-123. 10.3348/jksr.2015.73.2.116.
Clinical Usefulness of C-Arm Cone-Beam CT in Percutaneous Drainage of Inaccessible Abscess
- Affiliations
-
- 1Department of Radiology, Seoul Metropolitan Government Seoul National University Boramae Medical Center, Seoul, Korea. sorock71@snu.ac.kr
- 2Department of Radiology, National Cancer Center, Goyang, Korea.
- KMID: 1964263
- DOI: http://doi.org/10.3348/jksr.2015.73.2.116
Abstract
- PURPOSE
The objective of this study was to evaluate the usefulness of C-arm cone-beam CT (CBCT) in drainage of inaccessible abscesses.
MATERIALS AND METHODS
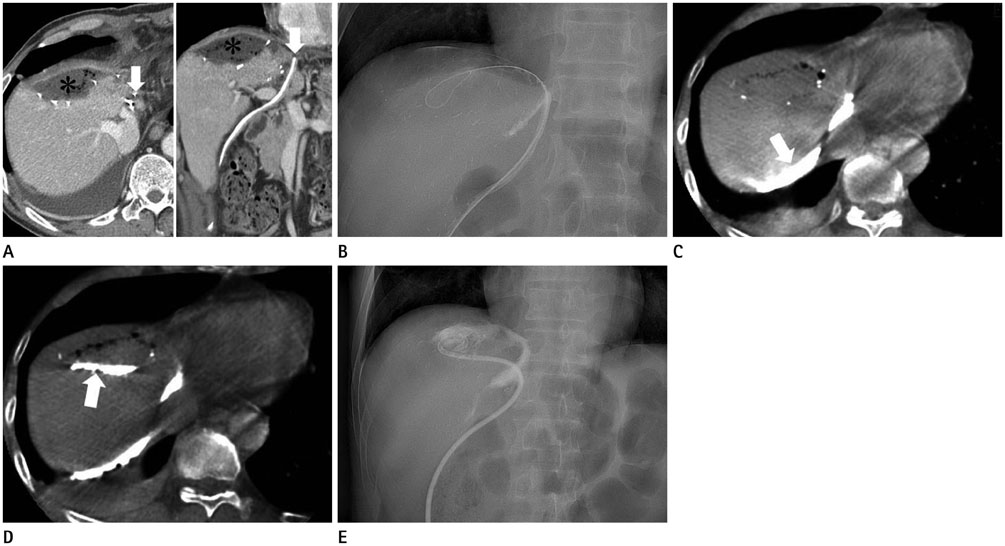
To identify the trajectory of the needle or guide wire, CBCT was performed on 21 patients having an inaccessible abscess. CBCT was repeated until proper targeting of the abscess was achieved, before the insertion of a large bore catheter. The etiology, location of the abscess, causes of inaccessibility, radiation dose, technical and clinical success rates of drainage, and any complications confronted, were evaluated.
RESULTS
A total of 29 CBCTs were performed for 21 abscesses. Postoperative and non-postoperative abscesses were 9 (42.9%) and 12 (57.1%) in number, respectively. Direct puncture was performed in 18 cases. In 3 cases, the surgical drain or the fistula opening was used as an access route. The causes of inaccessibility were narrow safe window due to adjacent or overlying organs (n = 9), irregularly dispersed abscess (n = 7), deep location with poor sonographic visualization (n = 4), and remote location of the abscess from surgical drain (n = 1). Technical and clinical successes were 95.5% and 100%, respectively. Cumulative air kerma and dose-area product were 21.62 +/- 5.41 mGy and 9179.87 +/- 2337.70 mGycm2, respectively. There were no procedure related complications.
CONCLUSION
CBCT is a useful technique for identifying the needle and guide wire during drainage of inaccessible abscess.
MeSH Terms
Figure
Reference
-
1. Montgomery RS, Wilson SE. Intraabdominal abscesses: image-guided diagnosis and therapy. Clin Infect Dis. 1996; 23:28–36.2. Men S, Akhan O, Köroğlu M. Percutaneous drainage of abdominal abcess. Eur J Radiol. 2002; 43:204–218.3. Mueller PR, Ferrucci JT Jr, Simeone JF, Butch RJ, Wittenberg J, White M, et al. Lesser sac abscesses and fluid collections: drainage by transhepatic approach. Radiology. 1985; 155:615–618.4. Maher MM, Gervais DA, Kalra MK, Lucey B, Sahani DV, Arellano R, et al. The inaccessible or undrainable abscess: how to drain it. Radiographics. 2004; 24:717–735.5. vanSonnenberg E, Mueller PR, Ferrucci JT Jr. Percutaneous drainage of 250 abdominal abscesses and fluid collections. Part I: Results, failures, and complications. Radiology. 1984; 151:337–341.6. Duszak RL Jr, Levy JM, Akins EW, Bakal CW, Denny DD Jr, Martin LG, et al. Percutaneous catheter drainage of infected intra-abdominal fluid collections. American College of Radiology. ACR Appropriateness Criteria. Radiology. 2000; 215:Suppl. 1067–1075.7. Gerzof SG, Robbins AH, Johnson WC, Birkett DH, Nabseth DC. Percutaneous catheter drainage of abdominal abscesses: a five-year experience. N Engl J Med. 1981; 305:653–657.8. Lambiase RE, Deyoe L, Cronan JJ, Dorfman GS. Percutaneous drainage of 335 consecutive abscesses: results of primary drainage with 1-year follow-up. Radiology. 1992; 184:167–179.9. Civardi G, Fornari F, Cavanna L, Sbolli G, Di Stasi M, Buscarini L. Ultrasonically guided percutaneous drainage of abdominal fluid collections: a long-term study of its therapeutic efficacy. Gastrointest Radiol. 1990; 15:245–250.10. vanSonnenberg E, Wittich GR, Goodacre BW, Casola G, D'Agostino HB. Percutaneous abscess drainage: update. World J Surg. 2001; 25:362–369. discussion 370-37211. Kim YJ, Han JK, Lee JM, Kim SH, Lee KH, Park SH, et al. Percutaneous drainage of postoperative abdominal abscess with limited accessibility: preexisting surgical drains as alternative access route. Radiology. 2006; 239:591–598.12. Gupta R, Cheung AC, Bartling SH, Lisauskas J, Grasruck M, Leidecker C, et al. Flat-panel volume CT: fundamental principles, technology, and applications. Radiographics. 2008; 28:2009–2022.13. Rafferty MA, Siewerdsen JH, Chan Y, Moseley DJ, Daly MJ, Jaffray DA, et al. Investigation of C-arm cone-beam CT-guided surgery of the frontal recess. Laryngoscope. 2005; 115:2138–2143.14. Reichardt B, Sarwar A, Bartling SH, Cheung A, Grasruck M, Leidecker C, et al. Musculoskeletal applications of flat-panel volume CT. Skeletal Radiol. 2008; 37:1069–1076.15. Hirota S, Nakao N, Yamamoto S, Kobayashi K, Maeda H, Ishikura R, et al. Cone-beam CT with flat-panel-detector digital angiography system: early experience in abdominal interventional procedures. Cardiovasc Intervent Radiol. 2006; 29:1034–1038.16. Kim HC, Chung JW, Park JH, An S, Son KR, Seong NJ, et al. Transcatheter arterial chemoembolization for hepatocellular carcinoma: prospective assessment of the right inferior phrenic artery with C-arm CT. J Vasc Interv Radiol. 2009; 20:888–895.17. Wallace MJ, Kuo MD, Glaiberman C, Binkert CA, Orth RC, Soulez G. Technology Assessment Committee of the Society of Interventional Radiology. Three-dimensional C-arm cone-beam CT: applications in the interventional suite. J Vasc Interv Radiol. 2008; 19:799–813.18. Jin KN, Park CM, Goo JM, Lee HJ, Lee Y, Kim JI, et al. Initial experience of percutaneous transthoracic needle biopsy of lung nodules using C-arm cone-beam CT systems. Eur Radiol. 2010; 20:2108–2115.19. Hangiandreou NJ. AAPM/RSNA physics tutorial for residents. Topics in US: B-mode US: basic concepts and new technology. Radiographics. 2003; 23:1019–1103.20. Braak SJ, van Strijen MJ, van Leersum M, van Es HW, van Heesewijk JP. Real-Time 3D fluoroscopy guidance during needle interventions: technique, accuracy, and feasibility. AJR Am J Roentgenol. 2010; 194:W445–W451.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Percutaneous drainage of abdominal abscess
- Percutaneous catheter drainage of intraabdominal abscess
- Treatment of P yogenic Liver Abscess by Percutaneous Needle Aspiration and / or Percutaneous Catheter Drainage
- Role of C-Arm Cone-Beam CT in Chemoembolization for Hepatocellular Carcinoma
- Percutaneous Drainage of Emphysematous Pyelonephritis Associated with Abscess: Report of 2 cases