J Korean Soc Radiol.
2015 Aug;73(2):91-99. 10.3348/jksr.2015.73.2.91.
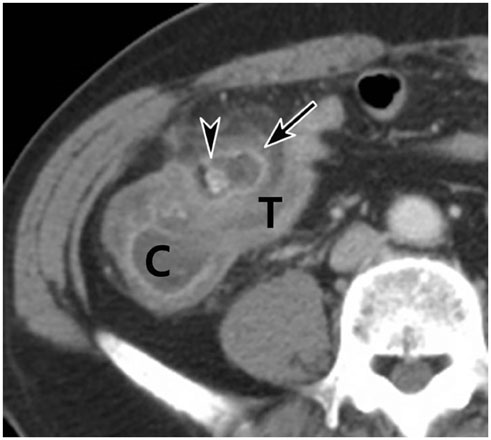
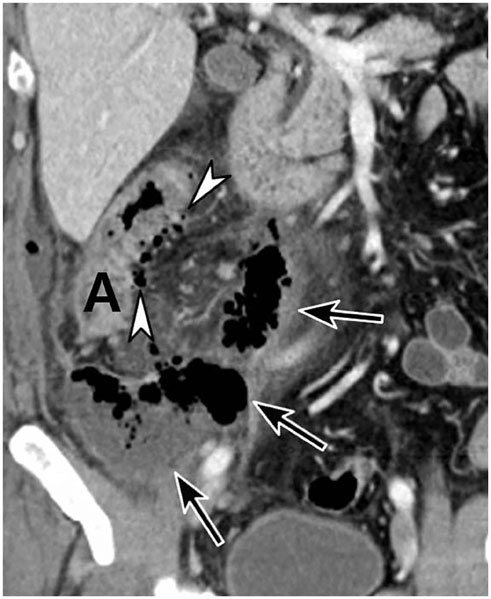
The Surgical Rate and Recurrence Rate in Right Colonic Diverticulitis Using the CT-Based Modified Hinchey Classification
- Affiliations
-
- 1Department of Radiology, Daejin Medical Center Bundang Jesaeng General Hospital, Seongnam, Korea. hyukjungk@naver.com
- 2Department of Radiology, Seoul National University Bundang Hospital, Seongnam, Korea.
- 3Program in Biomedical Radiation Sciences, Department of Transdisciplinary Studies, Graduate School of Convergence Science and Technology, Seoul National University, Seoul, Korea.
- KMID: 1964258
- DOI: http://doi.org/10.3348/jksr.2015.73.2.91
Abstract
- PURPOSE
The purpose of this report is to retrospectively analyze the need for surgery, and the recurrence rate, using a CT-based method in patients with right colonic diverticulitis.
MATERIALS AND METHODS
For the purposes of our study, we included 416 patients with a mean age of 41.9 (238 of which were men), with a diagnosis of colonic diverticulitis that was based on CT findings. These findings were reviewed by two independent radiologists, who localized diverticulitis and determined it using a modified Hinchey classification. We were able to follow-up with 384 patients over a period of 30 months.
RESULTS
Out of the 416 patients, 396 of them had right colonic diverticulitis. In right colonic diverticulitis, the kappa value in determining the modified Hinchey classification was 0.80. 98.2% (389/396) of the patients with right colonic diverticulitis had stages Ia-II. The surgery rate was 4.6% (17/366) and 28% (5/18) for right and left colonic diverticulitis, respectively (p < 0.001). In the instances of right colonic diverticulitis, the surgery rate was 2.8% (10/359) for stages Ia-II, while all seven patients with stage III or IV underwent surgery. The recurrence rate was 6.5% (23/356) and 15% (2/13) for right and left colonic diverticulitis, respectively (p = 0.224).
CONCLUSION
The CT-based modified Hinchey classification of right colonic diverticulitis showed good interobserver agreement. Most patients with right colonic diverticulitis had lower stages (Ia-II) at the point of CT, rarely needed surgery, and had a low recurrence rate.
MeSH Terms
Figure
Reference
-
1. Lo CY, Chu KW. Acute diverticulitis of the right colon. Am J Surg. 1996; 171:244–246.2. Katz DS, Lane MJ, Ross BA, Gold BM, Jeffrey RB Jr, Mindelzun RE. Diverticulitis of the right colon revisited. AJR Am J Roentgenol. 1998; 171:151–156.3. Law WL, Lo CY, Chu KW. Emergency surgery for colonic diverticulitis: differences between right-sided and left-sided lesions. Int J Colorectal Dis. 2001; 16:280–284.4. Komuta K, Yamanaka S, Okada K, Kamohara Y, Ueda T, Makimoto N, et al. Toward therapeutic guidelines for patients with acute right colonic diverticulitis. Am J Surg. 2004; 187:233–237.5. Goh V, Halligan S, Taylor SA, Burling D, Bassett P, Bartram CI. Differentiation between diverticulitis and colorectal cancer: quantitative CT perfusion measurements versus morphologic criteria--initial experience. Radiology. 2007; 242:456–462.6. Kim K, Kim YH, Kim SY, Kim S, Lee YJ, Kim KP, et al. Low-dose abdominal CT for evaluating suspected appendicitis. N Engl J Med. 2012; 366:1596–1605.7. Ferzoco LB, Raptopoulos V, Silen W. Acute diverticulitis. N Engl J Med. 1998; 338:1521–1526.8. Jang HJ, Lim HK, Lee SJ, Choi SH, Lee MH, Choi MH. Acute diverticulitis of the cecum and ascending colon: thin-section helical CT findings. AJR Am J Roentgenol. 1999; 172:601–604.9. Kaiser AM, Jiang JK, Lake JP, Ault G, Artinyan A, Gonzalez-Ruiz C, et al. The management of complicated diverticulitis and the role of computed tomography. Am J Gastroenterol. 2005; 100:910–917.10. Jacobs DO. Clinical practice. Diverticulitis. N Engl J Med. 2007; 357:2057–2066.11. Sheth AA, Longo W, Floch MH. Diverticular disease and diverticulitis. Am J Gastroenterol. 2008; 103:1550–1556.12. Ambrosetti P, Chautems R, Soravia C, Peiris-Waser N, Terrier F. Long-term outcome of mesocolic and pelvic diverticular abscesses of the left colon: a prospective study of 73 cases. Dis Colon Rectum. 2005; 48:787–791.13. Ambrosetti P, Becker C, Terrier F. Colonic diverticulitis: impact of imaging on surgical management -- a prospective study of 542 patients. Eur Radiol. 2002; 12:1145–1149.14. Wasvary H, Turfah F, Kadro O, Beauregard W. Same hospitalization resection for acute diverticulitis. Am Surg. 1999; 65:632–635. discussion 63615. Werner A, Diehl SJ, Farag-Soliman M, Düber C. Multi-slice spiral CT in routine diagnosis of suspected acute left-sided colonic diverticulitis: a prospective study of 120 patients. Eur Radiol. 2003; 13:2596–2603.16. Klarenbeek BR, de Korte N, van der Peet DL, Cuesta MA. Review of current classifications for diverticular disease and a translation into clinical practice. Int J Colorectal Dis. 2012; 27:207–214.17. Cohen J. Weighted kappa: nominal scale agreement with provision for scaled disagreement or partial credit. Psychol Bull. 1968; 70:213–220.18. Tan KK, Wong J, Sim R. Non-operative treatment of right-sided colonic diverticulitis has good long-term outcome: a review of 226 patients. Int J Colorectal Dis. 2013; 28:849–854.19. Park SJ, Choi SI, Lee SH, Lee KY. Image-guided conservative management of right colonic diverticulitis. World J Gastroenterol. 2009; 15:5838–5842.20. Feingold D, Steele SR, Lee S, Kaiser A, Boushey R, Buie WD, et al. Practice parameters for the treatment of sigmoid diverticulitis. Dis Colon Rectum. 2014; 57:284–294.21. Chabok A, Påhlman L, Hjern F, Haapaniemi S, Smedh K. AVOD Study Group. Randomized clinical trial of antibiotics in acute uncomplicated diverticulitis. Br J Surg. 2012; 99:532–539.22. Reisman Y, Ziv Y, Kravrovitc D, Negri M, Wolloch Y, Halevy A. Diverticulitis: the effect of age and location on the course of disease. Int J Colorectal Dis. 1999; 14:250–254.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Predictive factors for conservative treatment failure of right colonic diverticulitis
- Risk Factors for Severe Diverticulitis in Computed Tomography-Confirmed Acute Diverticulitis in Korea
- Management of Colonic Diverticulitis Tailored to Location and Severity: Comparison of the Right and the Left Colon
- Right-sided acute diverticulitis in the West: experience at a university hospital in Argentina
- Analysis on the Surgical Treatment of Colonic Diverticulitis