J Cerebrovasc Endovasc Neurosurg.
2014 Sep;16(3):200-208. 10.7461/jcen.2014.16.3.200.
Endovascular Treatment of the Distal Internal Carotid Artery Large Aneurysm
- Affiliations
-
- 1Department of Neurosurgery, Uijongbu St. Mary's Hospital, School of Medicine, The Catholic University, Uijongbu, Korea. yooman@catholic.ac.kr
- KMID: 1963157
- DOI: http://doi.org/10.7461/jcen.2014.16.3.200
Abstract
OBJECTIVE
According to the development of endovascular technique and devices, larger aneurysms on the distal internal carotid artery (ICA) can be treated using a less invasive method. The authors report on clinical and angiographic outcomes of these aneurysms treated using an endovascular technique.
MATERIALS AND METHODS
Data on 21 patients with large aneurysms at distal ICA treated by endovascular method between January 2005 and December 2012 were included in this retrospective analysis.
RESULTS
Clinical outcome of patients showed strong correlation with the initial neurologic status (p < 0.05). Aneurysm morphology showed saccular, fusiform, and wide-neck in 12, six and three patients. Six patients underwent stent assisted coiling and the other 15 patients underwent simple coiling. Aneurysm occlusion was performed immediately after embolization with near-complete (Raymond class 1-2) in 20 patients (95.2%) and incomplete (Raymond class 3) in one patient (4.8%). Delayed thrombotic occlusion occurred in two patients and their clinical result was fatal. Another five patients died in the hospital, from massive brain edema and/or increased intracranial pressure due to initial subarachnoid hemorrhage. Overall mortality was 30% (seven out of 21). Fatal complication related to the endovascular procedure occurred in two patients with thrombosis at middle cerebral artery (one with stent, the other without it).
CONCLUSION
Recent developed endovascular device and technique is safe enough and a less invasive method for distal large or giant aneurysms. Based on our analysis of the study, we suspect that coil embolization of large distal ICA aneurysms (with or without stenting) is effective and safe.
Keyword
MeSH Terms
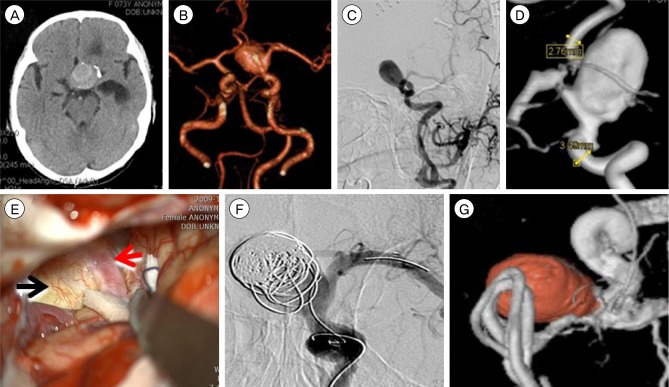
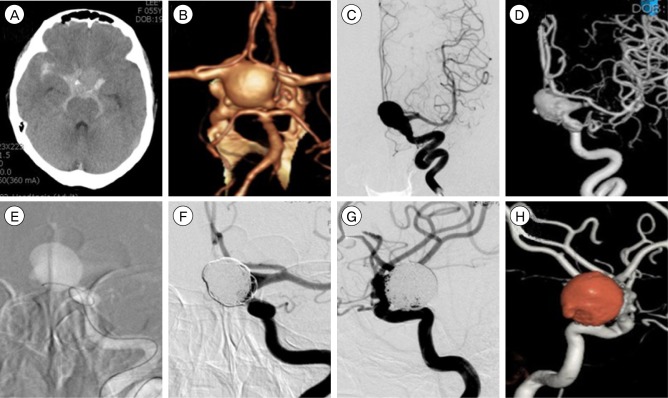
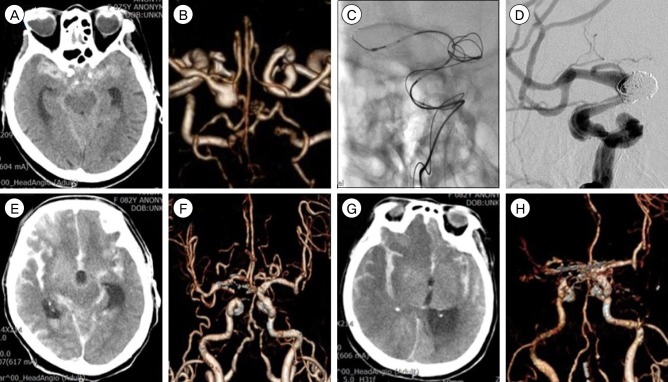
Figure
Cited by 1 articles
-
Endovascular management of large and giant intracranial aneurysms: Experience from a tertiary care neurosurgery institute in India
Gautam Dutta, Daljit Singh, Anita Jagetia, Arvind K Srivastava, Hukum Singh, Anil Kumar
J Cerebrovasc Endovasc Neurosurg. 2021;23(2):99-107. doi: 10.7461/jcen.2021.E2020.08.008.
Reference
-
1. Unruptured intracranial aneurysms-risk of rupture and risks of surgical intervention. International study of unruptured intracranial aneurysms investigators. N Engl J Med. 1998; 12. 339(24):1725–1733. PMID: 9867550.2. Becske T, Kallmes DF, Saatci I, McDougall CG, Szikora I, Lanzino G, et al. Pipeline for uncoilable or failed aneurysms: results from a multicenter clinical trial. Radiology. 2013; 6. 267(3):858–868. PMID: 23418004.
Article3. Cekirge HS, Saatci I, Ozturk MH, Cil B, Arat A, Mawad M, et al. Late angiographic and clinical follow-up results of 100 consecutive aneurysms treated with Onyx reconstruction: largest single-center experience. Neuroradiology. 2006; 2. 48(2):113–126. PMID: 16391915.
Article4. Colby GP, Lin LM, Gomez JF, Paul AR, Huang J, Tamargo RJ, et al. Immediate procedural outcomes in 35 consecutive pipeline embolization cases: a single-center, single-user experience. J Neurointerv Surg. 2013; 5. 5(3):237–246. PMID: 22459178.
Article5. Fiorella D, Albuquerque F, Gonzalez F, McDougall CG, Nelson PK. Reconstruction of the right anterior circulation with the Pipeline embolization device to achieve treatment of a progressively symptomatic, large carotid aneurysm. J Neurointerv Surg. 2010; 3. 2(1):31–37. PMID: 21990555.
Article6. Geyik S, Yavuz K, Cekirge S, Saatci I. Endovascular treatment of basilar and ICA termination aneurysms: effects of the use of HydroCoils on treatment stability in a subgroup of patients prone to a higher recurrence rate. Neuroradiology. 2007; 12. 49(12):1015–1021. PMID: 17909777.
Article7. Hauck EF, Welch BG, White JA, Replogle RE, Purdy PD, Pride LG, et al. Stent/coil treatment of very large and giant unruptured ophthalmic and cavernous aneurysms. Surg Neurol. 2009; 1. 71(1):19–24. discussion 24. PMID: 18423540.
Article8. lshikawa T, Kamiyama H, Kobayashi N, Tanikawa R, Takizawa K, Kazumata K. Experience from "double-insurance bypass." Surgical results and additional techniques to achieve complex aneurysm surgery in a safer manner. Surg Neurol. 2005; 5. 63(5):485–490. discussion 490. PMID: 15883084.
Article9. Lylyk P, Miranda C, Ceratto R, Ferrario A, Scrivano E, Luna HR, et al. Curative endovascular reconstruction of cerebral aneurysms with the pipeline embolization device: the Buenos Aires experience. Neurosurgery. 2009; 4. 64(4):632–642. discussion 642-3; quiz N6. PMID: 19349825.10. Mack WJ, Ducruet AF, Angevine PD, Komotar RJ, Shrebnick DB, Edwards NM, et al. Deep hypothermic circulatory arrest for complex cerebral aneurysms: lessons learned. Neurosurgery. 2007; 5. 60(5):815–827. discussion 815-27. PMID: 17460516.
Article11. Molyneux A, Kerr R, Stratton I, Sandercock P, Clarke M, Shrimpton J, et al. International Subarachnoid Aneurysm Trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomized trial. J Stroke Cerebrovasc Dis. 2002; Nov-Dec. 11(6):304–314. PMID: 17903891.
Article12. Nelson PK, Lylyk P, Szikora I, Wetzel SG, Wanke I, Fiorella D. The pipeline embolization device for the intracranial treatment of aneurysms trial. AJNR Am J Neuroradiol. 2011; 1. 32(1):34–40. PMID: 21148256.
Article13. Roski RA, Spetzler RF. Carotid ligation. In : Wilkins RH, Rengachary SS, editors. Neurosurgery. 2nd ed. New York: McGraw-Hill, Health Professions Division;1996. p. 002E 2333-40.14. Ryttlefors M, Enblad P, Kerr RS, Molyneux AJ. International subarachnoid aneurysm trial of neurosurgical clipping versus endovascular coiling: subgroup analysis of 278 elderly patients. Stroke. 2008; 10. 39(10):2720–2726. PMID: 18669898.15. Saatci I, Cekirge HS, Ozturk MH, Arat A, Ergungor F, Sekerci Z, et al. Treatment of internal carotid artery aneurysms with a covered stent: experience in 24 patients with mid-term follow-up results. AJNR Am J Neuroradiol. 2004; Nov-Dec. 25(10):1742–1749. PMID: 15569740.16. Sanus GZ, Akar Z, Tanriverdi T, Tutunculer B, Uzan M, Islak C, et al. Bypass to the intracranial giant or large internal carotid artery aneurysms: superficial temporal artery to middle cerebral artery bypass re-visited. Turk Neurosurg. 2007; 17(1):60–65. PMID: 17918682.17. Schaller B. Extracranial-intracranial bypass to reduce the risk of ischemic stroke in intracranial aneurysms of the anterior cerebral circulation: a systematic review. J Stroke Cerebrovasc Dis. 2008; 9. 17(5):287–298. PMID: 18755409.
Article18. Schaller B, Graf R. Cerebral ischemia and reperfusion: the pathophysiologic concept as a basis for clinical therapy. J Cereb Blood Flow Metab. 2004; 4. 24(4):351–371. PMID: 15087705.
Article19. Schaller B, Lyrer P. Focal neurological deficits following spontaneous thrombosis of unruptured giant aneurysms. Eur Neurol. 2002; 47(3):175–182. PMID: 11914557.
Article20. Siddiqui AH, Kan P, Abla AA, Hopkins LN, Levy EI. Complications after treatment with pipeline embolization for giant distal intracranial aneurysms with or without coil embolization. Neurosurgery. 2012; 8. 71(2):E509–E513. discussion E513. PMID: 22710418.
Article21. Sluzewski M, Menovsky T, van Rooij WJ, Wijnalda D. Coiling of very large or giant cerebral aneurysms: long-term clinical and serial angiographic results. AJNR Am J Neuroradiol. 2003; 2. 24(2):257–262. PMID: 12591644.22. Sorteberg A, Bakke SJ, Boysen M, Sorteberg W. Angiographic balloon test occlusion and therapeutic sacrifice of major arteries to the brain. Neurosurgery. 2008; 10. 63(4):651–660. discussion 660-1. PMID: 18824944.
Article23. Spetzler RF, Carter LP. Revascularization and aneurysm surgery: current status. Neurosurgery. 1985; 1. 16(1):111–116. PMID: 3883217.
Article24. Szikora I, Berentei Z, Kulcsar Z, Marosfoi M, Vajda ZS, Lee W, et al. Treatment of intracranial aneurysms by functional reconstruction of the parent artery: the Budapest experience with the pipeline embolization device. AJNR Am J Neuroradiol. 2010; 6. 31(6):1139–1147. PMID: 20150304.
Article25. van Doormaal TP, van der Zwan A, Verweij BH, Han KS, Langer DJ, Tulleken CA. Treatment of giant middle cerebral artery aneurysms with a flow replacement bypass using the excimer laser-assisted nonocclusive anastomosis technique. Neurosurgery. 2008; 7. 63(1):12–20. discussion 20-2. PMID: 18728564.
Article26. van Doormaal TP, van der Zwan A, Verweij BH, Langer DJ, Tulleken CA. Treatment of giant and large internal carotid artery aneurysms with a high-flow replacement bypass using the excimer laser-assisted nonocclusive anastomosis technique. Neurosurgery. 2006; 10. 59(4 Suppl 2):ONS328–ONS334. discussion ONS34-5. PMID: 17041501.
Article27. Wang JB, Li MH, Fang C, Wang W, Cheng YS, Zhang PL, et al. Endovascular treatment of giant intracranial aneurysms with willis covered stents: technical case report. Neurosurgery. 2008; 5. 62(5):E1176–E1177. discussion E1177. PMID: 18580791.28. Xu BN, Sun ZH, Romani R, Jiang JL, Wu C, Zhou DB, et al. Microsurgical management of large and giant paraclinoid aneurysms. World Neurosurg. 2010; 3. 73(3):137–146. discussion e17, e19. PMID: 20860951.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endovascular Treatment of a Fusiform Aneurysm Involving a Premammillary Artery Originating from the Internal Carotid Artery: A Case Report
- Aneurysm at the Origin of the Uncal Artery Arising from the Internal Carotid Artery
- Retrograde Suction Decompression with an Inahara Carotid Shunt for Clipping a Large Distal Internal Carotid Artery Aneurysm
- Stent-Assisted Coil Trapping in a Manual Internal Carotid Artery Compression Test for the Treatment of a Fusiform Dissecting Aneurysm
- Supraclinoid Internal Carotid Artery Fenestration Harboring an Unruptured Aneurysm and Another Remote Ruptured Aneurysm: Case Report and Review of the Literature