J Korean Med Assoc.
2005 Sep;48(9):808-821. 10.5124/jkma.2005.48.9.808.
Guidelines for Cardiac Rehabilitation
- Affiliations
-
- 1Sports and Health Medicine Center, Ulsan University College of Medicine, Asan Medical Center, Korea. ysjin@amc.seoul.kr
- KMID: 1958305
- DOI: http://doi.org/10.5124/jkma.2005.48.9.808
Abstract
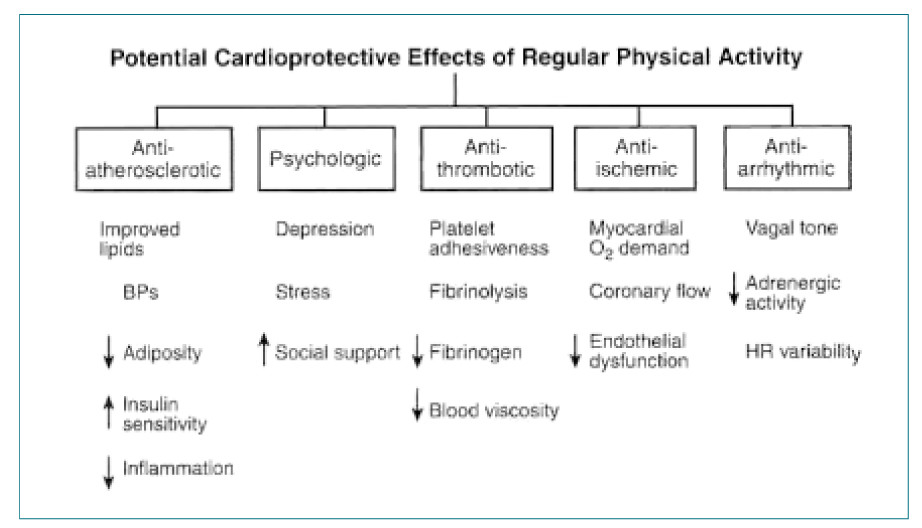
- Changes in cardiac rehabilitation in the 1990s involved the development of different patterns of the delivery of rehabilitative care. Patients were offered with a choice of individual versus group and center-based versus home-based physical activity programs. The recent application of risk-stratification procedures for coronary patients has brought major changes in the delivery of cardiac rehabilitation exercise training. Patients considered at low risk are able to undertake less supervised rehabilitation in a safe manner. Contemporary cardiac rehabilitation programs provide several important core components, including baseline patient assessment, nutrition counseling, risk factor management, psychosocial management, and activity counseling. However, appropriately prescribed exercise therapy remains the cornerstone of these programs. Cardiac rehabilitation programs have been categorized as phase I (inpatient), phase II (up to 12 weeks of ECG monitoring), phase II (no ECG monitoring under clinical supervision), and phase IV(no ECG monitoring, professional supervision). Cardiac patients who have specific needs to consider when formulating the exercise prescription include those with a history of myocardial infarction and angina, congestive heart failure, mitral valve stenosis and cardiac transplantation. Finally, the goals of rehabilitative care should include improvement of the functional capacity to achieve functional independence with an emphasis on quality of life.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Effects of Tai Chi Exercises on Cardiovascular Risks, Recurrence Risk, and Quality of Life in Patients with Coronary Artery Disease
Rha Yun Song, Moon Kyoung Park, Jin-Ok Cheong, Jae-Hyeong Park, In-Whan Seong
Korean J Adult Nurs. 2013;25(5):515-526. doi: 10.7475/kjan.2013.25.5.515.
Reference
-
1. Levin SA, Lown B. The 'chair treatment' of acute coronary thrombosis. Trans Assoc Am Physicians. 1951. 64:316–326.2. Chapman CB, Fraser RS. Studies on the effect of exercise on cardiovascular response to exercise on cardiovascular function. III. Cardiovascular response to exercise in pateint with healded myocardial infarction. Circulation. 1954. 9:347–351.
Article3. American College of Sports Medicine. Guidelines for Graded Exercise Testing and Exercise Prescription. 1975. Philadelphia: Lea & Febiger.4. American Heart Association. The Exercise Standards Book. 1979. Dallas: American Heart Association.5. AACVPR. Guidelines for cardiac rehabilitation and secondary prevention programs. 1999. Human Kintics.6. ACSM. ACSM's guidelines for exercise testing and prescription. 2005. 7th ed. LWW;174–204.7. DeBusk RF, Haskell WL, Miller NH, Berra K, Taylor CB, Lew H, et al. Medically directed at-home rehabilitation after uncomplicated acute myocardial infarction: a new model for patient care. Am J Cardiol. 1985. 55:251–257.
Article8. Fletcher BJ, Dunbar SB, Felner JM, Jensen BE, Almon L, Fletcher GF, et al. Exercise testing and training in physically disabled men with clinical evidence of coronary artery disease. Am J Cardiol. 1994. 73:170–174.
Article9. Hedback B, Perk J, Engvall J. Pedictive factors for return to work after coronary artery bypass grafting: the role of cardiac rehabilitation. Int J Rehabil Med. 1990. 22:15–20.10. Raineri A, Assennato P, Candela B, Messina L. Short and long term results of early rehabilitation after myocardial infarction: physical fitness, hemodynamic assessments and psychological aspects. Cardiology. 1982. 69:231–241.
Article11. Tran ZV, Weltman A. Differential effects of exercise on serum lipid and lipoprotein levels seen with changes in body weight: A meta-analysis. JAMA. 1985. 254:919–924.
Article12. ACSM. ACSM's guidelines for exercise testing and prescription. 2005. 7th ed. LWW;188.13. Van Camp SP, Peterson RA. Cardiovascular complication of outpatient cardiac rehabilitation pregrams. JAMA. 1986. 256:1160–1163.
Article14. Hossack KF, Hartwig R. Cardiac arrest associated with supervised cardiac rehabilitation. J Cardiac Rehabil. 1982. 2:402–408.15. Jugdutt BI, Michorowski BL, Kappagoda CT. Exercise training after anterior Q wave myocardial infarction: importance of regional left ventricular function and topography. J Am Coll Cardiol. 1988. 12:362–372.
Article16. Rowe MH, Jelinek MV, Liddell N, Hugens M. Effect of rapid mobilization on ejection fractions and ventricular volume after acute myocardial infarction. Am J Cardiol. 1989. 63:1037–1041.
Article17. American Association of Cardiovascular and Pulmonary Rehabilitation. Guidelines for Cardiac Rehabilitation and Secondary Prevention Programs. 2003. 4th ed. Champaign, IL: Human Kinetics.18. ACSM. ACSM's guidelines for exercise testing and prescription. 2005. 7th ed. LWW;22–27.19. ACSM. ACSM's guidelines for exercise testing and prescription. 2005. 7th ed. LWW;178–180.20. Pollack ML, Franklin BA, Balady GJ. Resistance exercise in individuals with and without cardiovascular disease: benefits, rationale, safety and prescription. Circulation. 2000. 101:828–833.
Article21. Hickson RC, Rosenkoetter MA, Brown MM. Strength training effects on aerobic power and short term endurance. Med Sci Sports Exerc. 1980. 12:336–339.22. McCartney N, McKelvie R, Haslam D, Jones N. Usefulness of weightlifting training in improving strength and maximal power output in coronary artery disease. Am J Cardiology. 1991. 67:939–945.
Article23. Franklin B, Bonzheim K, Gordon S, Timmis G. Resistence training in cardiac rehabilitation. J Cardiopulmonary Rehabil. 1991. 11:99–107.24. Verril D, Ribisl P. Resistive exercise training in cardiac rehabilitation. An update. Sports Med. 2001. 5:347–383.25. American Association of Cardiovascular and Pulmonary Rehabilitation. Guidelines for Cardiac Rehabilitation and Secondary Prevention Programs. 2003. 4th ed. Champaign, IL: Human Kinetics.26. ACSM. ACSM's guidelines for exercise testing and prescription. 2005. 7th ed. LWW;190.27. Schuler G, Hambrecht R, Schlierf G, et al. Regular physical exercise and low-fat diet. Effects on Progression of coronary artery disease. Circulation. 1992. 86:1–11.
Article28. Gitkin A, Ganulette M, Friedman D. Durstine JL, Moore GE, editors. Angina and silent is chemia. American College of Sports Medicine's Exercise Management for Persons with Chronic Disease and Disabilities. 2003. 2nd ed. Champaign, IL: Human Kinetics;64–69.29. Hoberg E, Schuler G, Kunze B, et al. Silent myocardial ischemia as a potential link between lack of premonitoring symptoms and increased risk of cardiac arrest during physical stress. Am J Cardiol. 1990. 65:583–589.
Article30. Lee AP, Ice RG, Blessey RL, et al. Long term effects of physical training on coronary patients with impaired ventricular function. Circulation. 1979. 60:1519–1526.
Article31. Sullivan MJ, Higginbotham MB, Cobb FR. Exercise training in patients with severe left ventricular dysfunction: hemodynamic and metabolic effects. Circulation. 1988. 78:506–515.
Article32. Coats AJS, Adamopoulos S, Meyer TE, et al. Effects of exercise training in chronic heart failure. Lancet. 1990. 263:3029–3042.33. Coats AJS, Adamopoulos S, Radaelli A, et al. Controlled trial of physical training in chronic heart failure: exercise performance, hemodynamics, ventilation and autonomic function. Circulation. 1992. 85:2119–2131.
Article34. Myers JN, Brubaker PH. Durstin JL, Moore GE, editors. Chronic heart failure. American College of Sports Medicine's Exercise Management for Persons with Chronic Disease and Disabilities. 2003. 2nd ed. Champaign IL: Human Kinetics;64–69.35. Meyer K, Samek L, Schwaibold M, Westbrook S, Hajric R, Lehmann M, et al. Physical responses to different modes of interval exercise in patients with chronic heart failure-application to exercise training. Er Heart J. 1996. 17:1040–1047.
Article36. McKay CR, Kawanishi DT, Kotlewski A, et al. Improvement in exercise capacity and exercise hemodynamics 3 month after double-ballon, catheter ballon valvuoplasty treatment of patients with symptomatic mitral stenosis. Circulation. 1988. 77:1013–1021.
Article37. Kasalicky J, Hurych J, Widmsky J, Dejdar R, Metys R, Stanek V. Left heart hemodynamics at rest during exercise hemodynamics in patients with mitral stenosis. Br Heart J. 1968. 30:188–195.
Article38. Stefandes C, Stratos C, Pitsavos C, et al. Retrograde nontranseptal ballon mitral valvuloplasty: immediate results and long-term follow-up. Circulation. 1992. 85:1760–1767.
Article39. Douard H, Chevalier L, Labbe L, Choussat A, Brouster JP. Physical training improves exercise capacity in patients with mitral stenosis after ballonvalvuloplasty. Er Heart J. 1997. 18(3):464–469.
Article40. Lim HY, Jin YS, Lee CW, Park SW, Kim JJ, Song JK, et al. Kinetics of recovery oxygen consumption after maximal graded exercise in patients with mitral stenosis: Effects of percutaneous ballon mitral valvuoplasty and exercise training. In press.41. Squires RW. Cardiac rehabilitation issues for heart transplantation patients. J Cardiopulm Rehabil. 1990. 10:159–168.
Article42. Keteyian S, Ehrman M, Fedel F, Rhoads K. Heart rate perceived exertion relationship during exercise in orthotopic heart transplantation patients. J Cardiopulm Rehabil. 1990. 10:287–293.
Article43. Kappagoda CT, Haennel RG, Serrano-fiz S, Davies DH, English TA. The hemodynamic responses to upright exercise after orthotopic cardiac transplant. Arch Phy Med Rehabil. 1993. 74:484–489.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Integrating Cardiac Rehabilitation with Neurorehabilitation in a Patient with Ischemic Stroke after Cardiac Surgery: a Case Report
- Analyses of Studies on Cardiac Rehabilitation for Patients with Cardiovascular Disease in Korea
- Fact Sheet on Cardiac Rehabilitation for Cardiovascular Disease in South Korea
- Cardiac Rehabilitation After Acute Myocardial Infarction Resuscitated From Cardiac Arrest
- Cardiac rehabilitation