Infect Chemother.
2011 Aug;43(4):367-371. 10.3947/ic.2011.43.4.367.
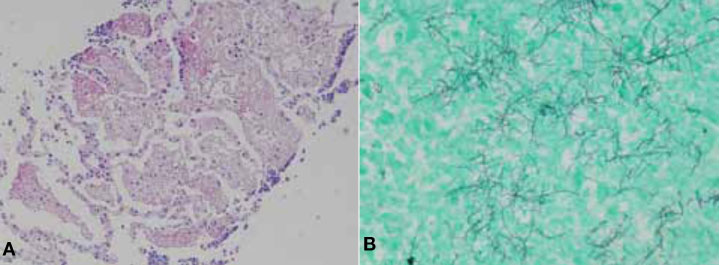
A Case of Disseminated Nocardiosis by Nocardia brasiliensis after Steroid Injection
- Affiliations
-
- 1Department of Internal Medicine, Chosun University, School of Medicine, Gwangju, Korea. drongkim@chosun.ac.kr
- 2Department of Laboratory Medicine, Chosun University, School of Medicine, Gwangju, Korea.
- 3Department of Pathology, Chosun University, School of Medicine, Gwangju, Korea.
- KMID: 1936076
- DOI: http://doi.org/10.3947/ic.2011.43.4.367
Abstract
- Nocardiosis in the immunocompromised host is a rare but life-threatening infection. Nocardia farcinica and N. asteroides have been reported as the most common causative pathogens of disseminated nocardiosis. It is well known that infection of N. brasiliensis can cause cutaneous nocardiosis mainly, but is rarely known to cause disseminated nocardiosis. We report a case of disseminated nocardiosis by N. brasiliensis. A 68-year-old male subject with no underlying disease developed painful swelling on both lower legs, as well as dyspnea. He was diagnosed with intramuscular abscess, pneumonia and brain abscess by N. brasiliensis. He underwent incision and drainage for intramuscular abscess, as well as antibiotic therapy, and was successfully treated.
Keyword
MeSH Terms
Figure
Reference
-
1. Brown-Elliott BA, Brown JM, Conville PS, Wallace RJ Jr. Clinical and laboratory features of the Nocardia spp. based on current molecular taxonomy. Clin Microbiol Rev. 2006. 19:259–282.
Article2. Lerner PI. Nocardiosis. Clin Infect Dis. 1996. 22:891–903. quiz 904-5.
Article3. Agterof MJ, van der Bruggen T, Tersmette M, ter Borg EJ, van den Bosch JM, Biesma DH. Nocardiosis: a case series and a mini review of clinical and microbiological features. Neth J Med. 2007. 65:199–202.4. Amatya R, Koirala R, Khanal B, Dhakal SS. Nocardia brasiliensis primary pulmonary nocardiosis with subcutaneous involvement in an immunocompetent patient. Indian J Med Microbiol. 2011. 29:68–70.
Article5. Shin JU, Kwon YS, Kim HJ, Park Y, Lee K, Lee KH. A case of disseminated cutaneous nocardiosis due to Nocardia brasiliensis diagnosed by fine needle aspiration biopsy and 16S ribosomal RNA sequencing. Korean J Dermatol. 2009. 47:1024–1028.6. Sim SH, Park HC, Kim CJ, Jeon JH, Kim EC, Oh MD, Kim NJ, Choe KW. A case of Nocardia farcinica brain abscess in the patient receiving steroid treatment. Infect Chemother. 2008. 40:301–304.
Article7. Han ST, Kim YS, Song SH, Uh Y, Han BG, Choi SO, Yang JW. A case of Nocardia farcinica brain abscess in a focal segmental glomerulosclerosis patient after steroid treatment. Korean J Nephrol. 2011. 30:98–101.8. Lee SH, Park BH, Son JY, Jung JY, Kim EY, Lim JE, Lee JH, Hyun SY, Lee SH, Lee SK, Kim SY, Lee KJ, Kang YA, Kim YS, Kim SK, Chang J, Seo YK, Lee KW, Park MS. A case of pneumonia with septic shock due to Nocardia farcinia in liver transplant patient. Tuberc Respir Dis. 2010. 69:469–473.
Article9. Park KH, Ko SY, Oh R, Kim T, Cho OH, Kim YS, Woo JH, Han DJ, Sung H, Kim MN. A case of lung abscess caused by Nocardia elegans in a kidney transplantation recipient. Infect Chemother. 2008. 40:116–120.
Article10. Tan CK, Lai CC, Lin SH, Liao CH, Chou CH, Hsu HL, Huang YT, Hsueh PR. Clinical and microbiological characteristics Nocardiosis including those caused by emerging Nocardia species in Taiwan, 1998-2008. Clin Microbiol Infect. 2010. 16:966–972.
Article11. Tremblay J, Thibert L, Alarie I, Valiquette L, Pépin J. Nocardiosis in Quebec, Canada, 1988-2008. Clin Microbiol Infect. 2011. 17:690–696.
Article12. Steer A. Focal pulmonary alveolar proteinosis in pulmonary tuberculosis. Arch Pathol. 1969. 87:347–352.13. Kawkitinarong K, Sittipunt C, Wongtim S, Udompanich V. Pulmonary alveolar proteinosis: a report of seven patients from King Chulalongkorn memorial hospital. J Med Assoc Thai. 2005. 88:Suppl 4. S312–S316.14. Mandell GL, Bennett GE, Dolin R, editors. Principles and Practice of Infectious disease. 2009. 7th ed. Philedelphia: Churchill Livingstone;3199–3208.15. Minero MV, Marín M, Cercenado E, Rabadán PM, Bouza E, Muñoz P. Nocardiosis at the turn of the century. Medicine (Baltimore). 2009. 88:250–261.
Article16. Uhde KB, Pathak S, McCullum I Jr, Jannat-Khah DP, Shadomy SV, Dykewicz CA, Clark TA, Smith TL, Brown JM. Antimicrobial-resistant Nocardia isolates, United States, 1995-2004. Clin Infect Dis. 2010. 51:1445–1448.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Disseminated Cutaneous Nocardiosis due to Nocardia brasiliensis Diagnosed by Fine Needle Aspiration Biopsy and 16S Ribosomal RNA Sequencing
- Primary Cutaneous Nocardiosis Caused by Nocardia brasiliensis
- Primary Cutaneous Nocardiosis Caused by Nocardia farcinica
- A Case of Disseminated Nocardiosis Secondary to the Skin Nodules in an Elderly Woman
- Primary Cutaneous Nocardiosis Caused by Nocardia niigatensis