Korean J Perinatol.
2014 Mar;25(1):1-8. 10.14734/kjp.2014.25.1.1.
Pathophysiology and Risk Factors of Pulmonary Hypertension in Infants with Bronchopulmonary Dysplasia
- Affiliations
-
- 1Department of Pediatrics, Dongguk University Ilsan Hospital, Goyang, Korea. dayeong1@dumc.or.kr
- KMID: 1917226
- DOI: http://doi.org/10.14734/kjp.2014.25.1.1
Abstract
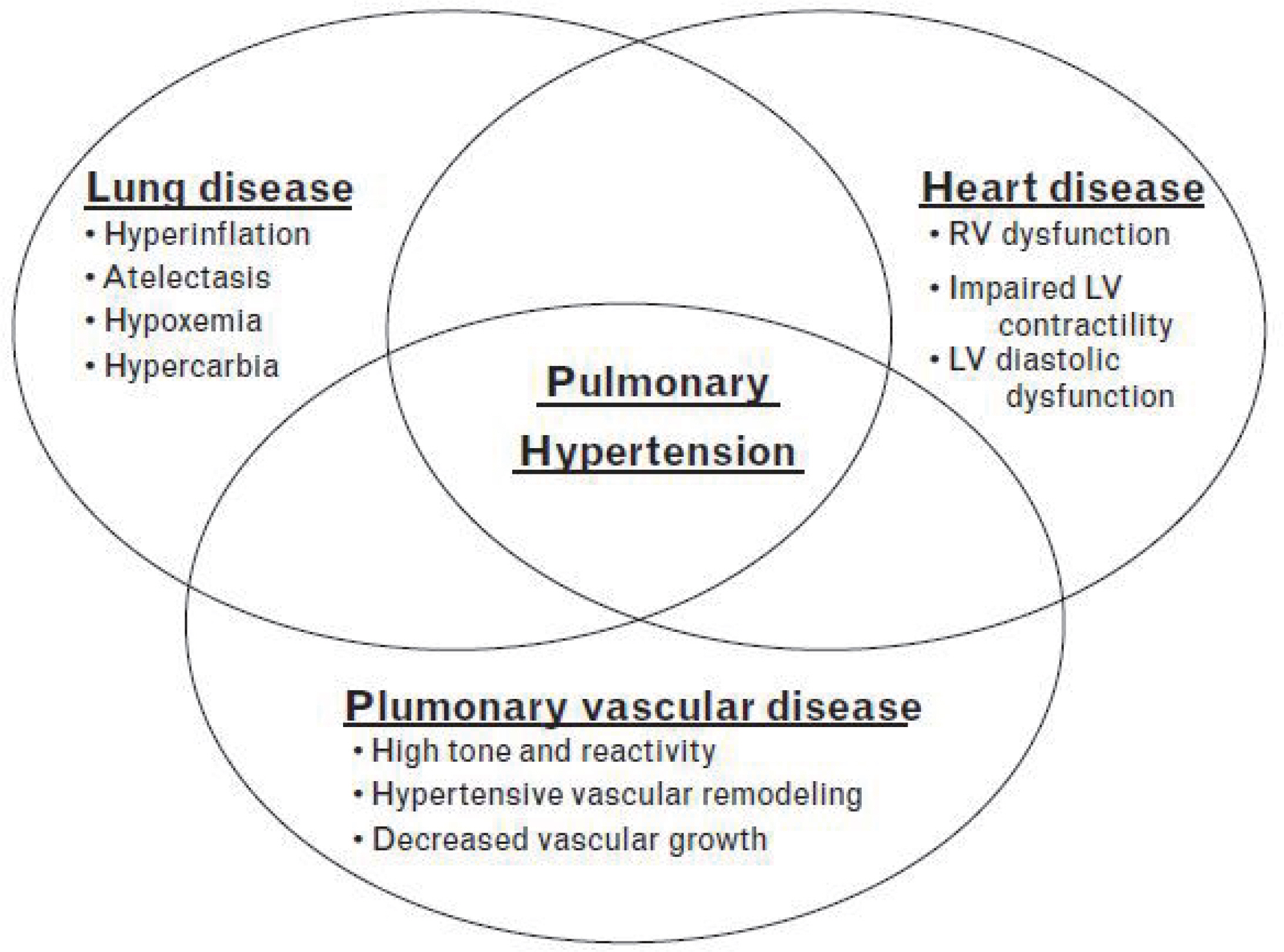
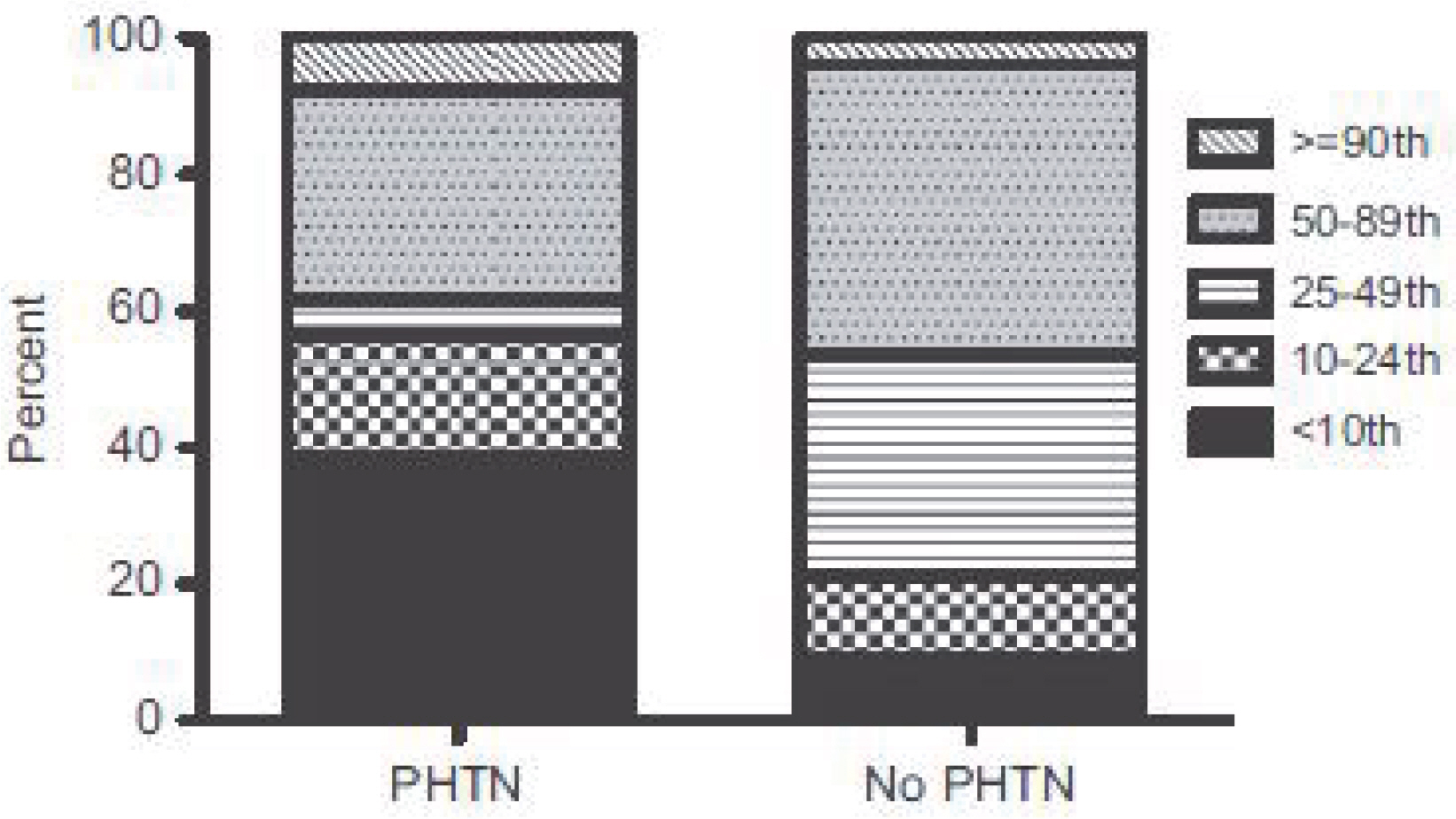
- Early injury to the lung circulation leads to the rapid development of pulmonary hypertension (PH) after premature birth. PH in bronchopulmonary dysplasia (BPD) results from increased vascular tone and abnormal vasoreactivity, hypertensive remodeling, and decreased vascular growth. The development of PH is sometimes a serious complication of BPD that can significantly impact the morbidity and mortality rates of preterm infants. Despite a gradual reduction in pulmonary arterial pressure postnatally, approximately a quarter of BPD infants have echocardiographic evidence of PH later. The pathogenesis of PH in BPD is very complex and multifactorial, often resulting from interactions between genetic and environmental or acquired factors (both prenatal and postnatal). Antenatal risk factors such as intrauterine growth retardation, maternal preeclampsia, and oligohydramnios suggest compelling evidence for the fetal origins of PH. Despite the potential importance of PH in preterm infants, the pathophysiology and the risk factors of PH in infants with BPD are still poorly understood. I have reviewed recent progress in research concerning the pathophysiology including the risk factors of PH in infants with BPD.
MeSH Terms
Figure
Reference
-
1.Berger RM., Beghetti M., Humpl T., Raskob GE., Ivy DD., Jing ZC, et al. Clinical features of paediatric pulmonary hypertension: a registry study. Lancet. 2012. 379:537–46.
Article2.Hwang JH. Neonatal pulmonary hypertension. Korean J Perinatol. 2013. 24:1–10.
Article3.An HS., Bae EJ., Kim GB., Kwon BS., Beak JS., Kim EK, et al. Pulmonary hypertension in preterm infants with bronchopulmonary dysplasia. Korean Circ J. 2010. 40:131–6.
Article4.Slaughter JL., Pakrashi T., Jones DE., South AP., Shah TA. Echocardiographic detection of pulmonary hypertension in extremely low birth weight infants with bronchopulmonary dysplasia requiring prolonged positive pressure ventilation. J Perinatol. 2011. 31:635–40.
Article5.DH Kim, HS Kim, CW Choi, EK Kim, BI Kim, JH Choi. Risk factors for pulmonary artery hypertension in preterm infants with moderate or severe bronchopulmonary dysplasia. Neonataology. 2012. 101:40–6.6.Bhat R., Salas AA., Foster C., Carlo WA., Ambalavanan N. Prospective analysis of pulmonary hypertension in extremely low birth weight infants. Pediatrics. 2012. 129:e682–9.
Article7.Khemani E., McElhinney DB., Rhein L., Andrade O., Lacro RV., Thomas KC, et al. Pulmonary artery hypertension in formerly premature infants with bronchopulmonary dysplasia: clinical features and outcomes in the surfactant era. Pediatrics. 2007. 120:1260–9.
Article8.Collaco JM., Romer LH., Stuart BD., Coulson JD., Everett AD., Lawson EE, et al. Frontiers in pulmonary hypertension in infants and children with bronchopulmonary dysplasia. Pediatr Pulmonol. 2012. 47:1042–53.
Article9.Northway WH Jr., Rosan RC., Porter DY. Pulmonary disease following respiratory therapy of hyaline-membrane disease. Bronchopulmonary dysplasia. N Engl J Med. 1967. 276:35768.10.Charafeddine L., D'Angio CT., Phelps DL. Atypical chronic lung disease patterns in neonates. Pediatrics. 1999. 103:75965.
Article11.Jobe AH., Bancalari E. Bronchopulmonary dysplasia. NICHD-NHLBI-ORD Workshop. Am J Respir Crit Care Med. 2001. 163:1723–9.12.Bancalari E., Claure N., Sosenko IR. Bronchopulmonary dysplasia: changes in pathogenesis, epidemiology and definition. Semin Neonatol. 2003. 8:63–71.
Article13.Husain AN., Siddiqui NH., Stocker JT. Pathology of arrested acinar development in postsurfactant bronchopulmonary dysplasia. Hum Pathol. 1998. 29:710–7.
Article14.Jobe AH. The new BPD: an arrest of lung development. Pediatr Res. 1999. 66:641–3.
Article15.Abman SH., Wolfe RR., Accurso FJ., Koops BL., Bowman CM., Wiggins JW Jr. Pulmonary vascular response to oxygen in infants with severe bronchopulmonary dysplasia. Pediatrics. 1985. 75:80–4.
Article16.Mourani PM., Ivy DD., Gao D., Abman SH. Pulmonary vascular effects of inhaled nitric oxide and oxygen tension in bronchopulmonary dysplasia. Am J Respir Crit Care Med. 2004. 170:1006–13.
Article17.Jakkula M., Le Cras TD., Gebb S., Hirth KP., Tuder RM., Voelkel NF, et al. Inhibition of angiogenesis decreases alveolarization in the developing rat lung. Am J Physiol Lung Cell Mol Physiol. 2000. 279:L600–7.
Article18.Le Cras TD., Markham NE., Tuder RM., Voelkel NF., Abman SH. Treatment of newborn rats with a VEGF receptor inhibitor causes pulmonary hypertension and abnormal lung structure. Am J Physiol Lung Cell Mol Physiol. 2002. 283:L555–62.19.Hislop AA., Haworth SG. Pulmonary vascular damage and the development of cor pulmonale following hyaline membrane disease. Pediatr Pulmonol. 1990. 9:152–61.
Article20.Mourani PM., Abman SH. Pulmonary vascular disease in bronchopulmonary dysplasia: pulmonary hypertension and beyond. Curr Opin Pediatr. 2013. 25:329–37.21.Stenmark KR., Abman SH. Lung vascular development: implications for the pathogenesis of bronchopulmonary dysplasia. Annu Rev Physiol. 2005. 67:623–61.
Article22.Abman SH. Impaired vascular endothelial growth factor signaling in the pathogenesis of neonatal pulmonary vascular disease. Adv Exp Med Biol. 2010. 661:323–35.
Article23.Wang CN., Chang SD., Peng HH., Lee YS., Chang YL., Cheng PJ, et al. Change in amniotic fluid levels of multiple antiangiogenic proteins before development of preeclampsia and intrauterine growth restriction. J Clin Endocrinol Metab. 2010. 95:1431–41.
Article24.Tang JR., Karumanchi SA., Seedorf G., Markham N., Abman SH. Excess soluble vascular endothelial growth factor receptor-1 in amniotic fluid impairs lung growth in rats: linking preeclampsia with bronchopulmonary dysplasia. Am J Physiol Lung Cell Mol Physiol. 2012. 302:L36–46.
Article25.Rozance PJ., Seedorf GJ., Brown A., Roe G., O'Meara MC., Gien J, et al. Intrauterine growth restriction decreases pulmonary alveolar and vessel growth and causes pulmonary artery endothelial cell dysfunction in vitro in fetal sheep. Am J Physiol Lung Cell Mol Physiol. 2011. 301:L860–71.
Article26.Afshar S., Gibson LL., Yuhanna IS., Sherman TS., Kerecman JD., Grubb PH, et al. Pulmonary NO synthase expression is attenuated in a fetal baboon model of chronic lung disease. Am J Physiol Lung Cell Mol Physiol. 2003. 284:L749–58.27.Farrow KN., Steinhorn RH. Phosphodiesterases: emerging therapeutic targets for neonatal pulmonary hypertension. Handb ExpPharmacol. 2011. 204:251–77.
Article28.Abdollahi A., Hahnfeldt P., Maercker C., Gröne HJ., Debus J., Ansorge W, et al. Endostatin's antiangiogenic signaling network. Mol Cel. 2004. 13:649–63.
Article29.Janér J., Andersson S., Kajantie E., Lassus P. Endostatin concentration in cord plasma predicts the development of bronchopulmonary dysplasia in very low birth weight infants. Pediatrics. 2009. 123:1142–6.30.DH Kim, HS Kim. Serial changes of serum endostatin and angiopoietin-1 levels in preterm infants with severe bronchopulmonary dysplasia and subsequent pulmonary artery hypertension. Neonatology. In press. 2014.31.Gien J., Tseng N., Seedorf G., Roe G., Abman SH. Endothelin-1 impairs angiogenesis in vitro through Rho-kinase activation after chronic intrauterine pulmonary hypertension in fetal sheep. Pediatr Res. 2013. 73:252–62.
Article32.Grover TR., Parker TA., Balasubramaniam V., Markham NE., Abman SH. Pulmonary hypertension impairs alveolarization and reduces lung growth in the ovine fetus. Am J Physiol Lung Cell Mol Physiol. 2005. 288:L648–54.
Article33.Saugstad OD. Oxygen and oxidative stress in bronchopulmonary dysplasia. J Perinat Med. 2010. 38:571–7.
Article34.Nozik-Grayck E., Stenmark KR. Role of reactive oxygen species in chronic hypoxia-induced pulmonary hypertension and vascular remodeling. Adv Exp Med Biol. 2007. 618:10112.
Article35.Jones R., Zapol WM., Reid L. Pulmonary artery remodeling and pulmonary hypertension after exposure to hyperoxia for 7 days. A morphometric and hemodynamic study. Am J Pathol. 1984. 117:273–85.36.Farquhar M., Fitzgerald DA. Pulmonary hypertension in chronic neonatal lung disease. Paediatr Respir Rev. 2010. 11:149–153.
Article37.Berkelhamer SK., Mestan KK., Steinhorn RH. Pulmonary hypertension in bronchopulmonary dysplasia. Semin Perinatol. 2013. 37:124–31.
Article38.Yoo HS., Kim MJ., Kang JM., Lee CG., Kim JK., Ahn SY, et al. Pulmonary hypertension secondary to bronchopulmonary dysplasia in very low birth weight infants (<1,500 g). Korean Soc Neonatol. 2011. 18:96–103.39.Check J., Gotteiner N., Liu X., Su E., Porta N., Steinhorn R, et al. Fetal growth restriction and pulmonary hypertension in premature infants with bronchopulmonary dysplasia. J Perinatol. 2013. 33:553–7.
Article40.Hansen AR., Barnes CM., Folkman J., McElrath TF. Maternal preeclampsia predicts the development of bronchopulmonary dysplasia. J Pediatr. 2010. 156:532–6.
Article41.Lapaire O., Shennan A., Stepan H. The preeclampsia biomarkers soluble fms-like tyrosine kinase-1 and placental growth factor: current knowledge, clinical implications and future application. Eur J Obstet Gynecol Reprod Biol. 2010. 151:122–9.
Article42.Kumar VH., Hutchison AA., Lakshminrusimha S., Morin FC III., Wynn RJ., Ryan RM. Characteristics of pulmonary hypertension in preterm neonates. J Perinatol. 2007. 27:214–9.
Article43.Cerro MJ., Abman S., Diaz G., Freudenthal AH., Freudenthal F., Harikrishnan S, et al. A consensus approach to the classification of pediatric pulmonary hypertensive vascular disease: report from the PVRI pediatric taskforce, Panama 2011. Pulm Circ. 2011. 1:286–98.
Article44.Mourani PM., Mullen M., Abman SH. Pulmonary hypertension in bronchopulmonary dysplasia. Progress in Pediatric Cardiology. 2009. 27:43–8.
Article45.Kim GB. Pulmonary hypertension in infants with bronchopulmonary dysplasia. Korean J Pediatr. 2010. 53:688–93.
Article46.Barst RJ. Classification of pediatric pulmonary hypertensive vascular disease: does it need to be different from the adult classification? Pulm Circ. 2011. 1:134–7.
Article47.Ra JJ., Lee SM., Eun HS., Park MS., Park KI., Namgung R, et al. Risk factors of pulmonary hypertension in preterm infants with chronic lung disease. Neonatal Med. 2013. 20:75–80.
Article48.Bhandari V., Bizzarro MJ., Shetty A., Zhong X., Page GP., Zhang H, et al. Neonatal Genetics Study Group. Familial and genetic susceptibility to major neonatal morbidities in preterm twins. Pediatrics. 2006. 117:1901–6.49.Lavoie PM., Pham C., Jang KL. Heritability of bronchopulmonary dysplasia, defined according to the consensus statement of the national institutes of health. Pediatrics. 2008. 122:479–85.
Article50.Li M., Riddle SR., Frid MG., El Kasmi KC., McKinsey TA., Sokol RJ, et al. Emergence of fibroblasts with a proinflammatory epigenetically altered phenotype in severe hypoxic pulmonary hypertension. J Immunol. 2011. 187:2711–22.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Characteristics, Presentation, and Outcomes of Bronchopulmonary Dysplasia-Associated Pulmonary Hypertension
- Survival of the Infants with Bronchopulmonary Dysplasia and Congenital Heart Disease
- Epidemiology, Clinical Characteristics, and Pathophysiology of Bronchopulmonary Dysplasia
- Neonatal Pulmonary Hypertension
- Use of Inhaled Iloprost in an Infant With Bronchopulmonary Dysplasia and Pulmonary Artery Hypertension