J Periodontal Implant Sci.
2014 Apr;44(2):94-99. 10.5051/jpis.2014.44.2.94.
Simultaneous placement of an interpositional free gingival graft with nonsubmerged implant placement
- Affiliations
-
- 1Department of Periodontology, Research Institute for Periodontal Regeneration, Yonsei University College of Dentistry, Seoul, Korea.
- 2Department of Periodontology, Research Institute for Periodontal Regeneration, Oral Science Research Center, Yonsei University College of Dentistry, Seoul, Korea. dentall@yuhs.ac
- KMID: 1914510
- DOI: http://doi.org/10.5051/jpis.2014.44.2.94
Abstract
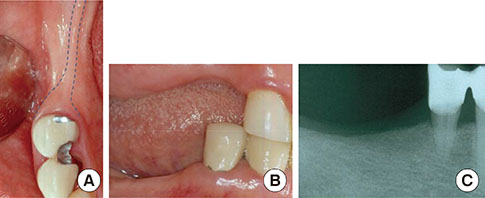
- PURPOSE
Various surgical techniques target achieving adequate keratinized tissue around dental implants; however, these techniques are usually performed before implant placement or upon the exposure of submerged implants. The aim of this case report is to describe a simultaneous placement of an interpositional free gingival graft (iFGG) with that of nonsubmerged implants in a patient lacking keratinized tissue and to assess the long-term outcome of this grafted gingiva.
METHODS
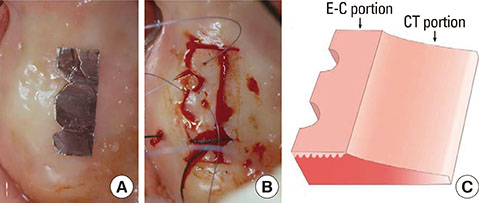
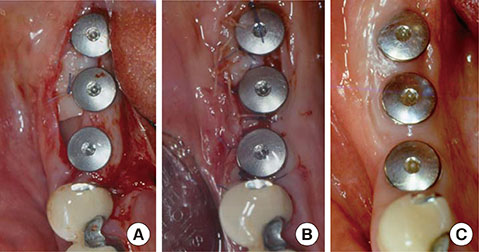
A wedge-shaped free gingnival graft (FGG), including an epithelium-connective tissue (E-C) portion and a connective-tissue-only (CT) portion, was harvested from the palate. The CT portion was inserted under the buccal flap, and the E-C portion was secured tightly around the implants and to the lingual flap.
RESULTS
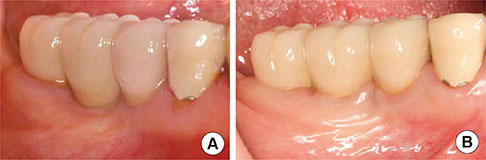
At the 8-year follow-up, the gingival graft remained firmly attached and was well maintained, with no conspicuous shrinkage or reported discomfort during oral hygiene procedures. The use of an iFGG at a nonsubmerged implant placement minimizes the required number of surgical steps and patient discomfort while providing adequate buccal keratinized tissue.
CONCLUSIONS
Therefore, the technique could be considered an alternative method in increasing the keratinized tissue for cases that have a minimal amount of keratinized tissue.
MeSH Terms
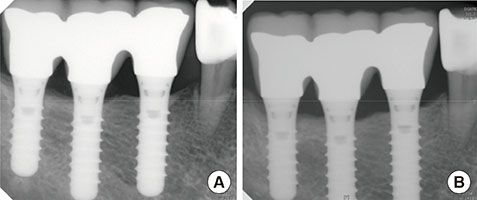
Figure
Reference
-
1. Ericsson I, Lindhe J. Probing depth at implants and teeth. An experimental study in the dog. J Clin Periodontol. 1993; 20:623–627.
Article2. Salonen MA, Oikarinen K, Virtanen K, Pernu H. Failures in the osseointegration of endosseous implants. Int J Oral Maxillofac Implants. 1993; 8:92–97.
Article3. Wennstrom JL, Bengazi F, Lekholm U. The influence of the masticatory mucosa on the peri-implant soft tissue condition. Clin Oral Implants Res. 1994; 5:1–8.
Article4. Adell R, Eriksson B, Lekholm U, Branemark PI, Jemt T. Long-term follow-up study of osseointegrated implants in the treatment of totally edentulous jaws. Int J Oral Maxillofac Implants. 1990; 5:347–359.5. Lekholm U, Adell R, Lindhe J, Branemark PI, Eriksson B, Rockler B, et al. T. Marginal tissue reactions at osseointegrated titanium fixtures. (II) A cross-sectional retrospective study. Int J Oral Maxillofac Surg. 1986; 15:53–61.6. Schou S, Holmstrup P, Hjorting-Hansen E, Lang NP. Plaque-induced marginal tissue reactions of osseointegrated oral implants: a review of the literature. Clin Oral Implants Res. 1992; 3:149–161.
Article7. Block MS, Kent JN. Factors associated with soft- and hard-tissue compromise of endosseous implants. J Oral Maxillofac Surg. 1990; 48:1153–1160.
Article8. Chung DM, Oh TJ, Shotwell JL, Misch CE, Wang HL. Significance of keratinized mucosa in maintenance of dental implants with different surfaces. J Periodontol. 2006; 77:1410–1420.
Article9. Listgarten MA, Lang NP, Schroeder HE, Schroeder A. Periodontal tissues and their counterparts around endosseous implants [corrected and republished with original paging, article orginally printed in Clin Oral Implants Res 1991 Jan-Mar;2(1):1-19]. Clin Oral Implants Res. 1991; 2:1–19.10. Zigdon H, Machtei EE. The dimensions of keratinized mucosa around implants affect clinical and immunological parameters. Clin Oral Implants Res. 2008; 19:387–392.
Article11. Bengazi F, Lang NP, Caroprese M, Urbizo Velez J, Favero V, Botticelli D. Dimensional changes in soft tissues around dental implants following free gingival grafting: an experimental study in dogs. Clin Oral Implants Res. 2013; 10. 24. [Epub]. http://dx.doi.org/10.1111/clr.12280.
Article12. Lin GH, Chan HL, Wang HL. The significance of keratinized mucosa on implant health: a systematic review. J Periodontol. 2013; 84:1755–1767.
Article13. Cario E. Barrier-protective function of intestinal epithelial Toll-like receptor 2. Mucosal Immunol. 2008; 1:Suppl 1. S62–S66.
Article14. Warrer K, Buser D, Lang NP, Karring T. Plaque-induced peri-implantitis in the presence or absence of keratinized mucosa. An experimental study in monkeys. Clin Oral Implants Res. 1995; 6:131–138.
Article15. Cairo F, Pagliaro U, Nieri M. Soft tissue management at implant sites. J Clin Periodontol. 2008; 35:8 Suppl. 163–167.
Article16. Lee KH, Kim BO, Jang HS. Clinical evaluation of a collagen matrix to enhance the width of keratinized gingiva around dental implants. J Periodontal Implant Sci. 2010; 40:96–101.
Article17. Park JC, Yang KB, Choi Y, Kim YT, Jung UW, Kim CS, et al. A simple approach to preserve keratinized mucosa around implants using a pre-fabricated implant-retained stent: a report of two cases. J Periodontal Implant Sci. 2010; 40:194–200.
Article18. Bouri A Jr, Bissada N, Al-Zahrani MS, Faddoul F, Nouneh I. Width of keratinized gingiva and the health status of the supporting tissues around dental implants. Int J Oral Maxillofac Implants. 2008; 23:323–326.19. Kim BS, Kim YK, Yun PY, Yi YJ, Lee HJ, Kim SG, et al. Evaluation of peri-implant tissue response according to the presence of keratinized mucosa. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009; 107:e24–e28.
Article20. Schrott AR, Jimenez M, Hwang JW, Fiorellini J, Weber HP. Five-year evaluation of the influence of keratinized mucosa on peri-implant soft-tissue health and stability around implants supporting full-arch mandibular fixed prostheses. Clin Oral Implants Res. 2009; 20:1170–1177.
Article21. Langer B, Langer L. Overlapped flap: a surgical modification for implant fixture installation. Int J Periodontics Restorative Dent. 1990; 10:208–215.22. Langer B, Sullivan DY. Osseointegration: its impact on the interrelationship of periodontics and restorative dentistry: Part I. Int J Periodontics Restorative Dent. 1989; 9:84–105.23. Tinti C, Parma-Benfenati S. Coronally positioned palatal sliding flap. Int J Periodontics Restorative Dent. 1995; 15:298–310.24. Sanz M, Lorenzo R, Aranda JJ, Martin C, Orsini M. Clinical evaluation of a new collagen matrix (Mucograft prototype) to enhance the width of keratinized tissue in patients with fixed prosthetic restorations: a randomized prospective clinical trial. J Clin Periodontol. 2009; 36:868–876.
Article25. Agudio G, Nieri M, Rotundo R, Cortellini P, Pini Prato G. Free gingival grafts to increase keratinized tissue: a retrospective long-term evaluation (10 to 25 years) of outcomes. J Periodontol. 2008; 79:587–594.
Article26. Hatipoglu H, Keceli HG, Guncu GN, Sengun D, Tozum TF. Vertical and horizontal dimensional evaluation of free gingival grafts in the anterior mandible: a case report series. Clin Oral Investig. 2007; 11:107–113.
Article27. Landi L, Sabatucci D. Plastic surgery at the time of membrane removal around mandibular endosseous implants: a modified technique for implant uncovering. Int J Periodontics Restorative Dent. 2001; 21:280–287.28. Seibert JS, Louis JV. Soft tissue ridge augmentation utilizing a combination onlay-interpositional graft procedure: a case report. Int J Periodontics Restorative Dent. 1996; 16:310–321. Erratum in: Int J Periodontics Restorative Dent 1996;16:521.29. Mormann W, Schaer F, Firestone AR. The relationship between success of free gingival grafts and transplant thickness. Revascularization and shrinkage: a one year clinical study. J Periodontol. 1981; 52:74–80.30. Orsini M, Orsini G, Benlloch D, Aranda JJ, Lazaro P, Sanz M. Esthetic and dimensional evaluation of free connective tissue grafts in prosthetically treated patients: a 1-year clinical study. J Periodontol. 2004; 75:470–477.
Article31. Barone R, Clauser C, Grassi R, Merli M, Prato GP. A protocol for maintaining or increasing the width of masticatory mucosa around submerged implants: a 1-year prospective study on 53 patients. Int J Periodontics Restorative Dent. 1998; 18:377–387.32. Park JB. Increasing the width of keratinized mucosa around endosseous implant using acellular dermal matrix allograft. Implant Dent. 2006; 15:275–281.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Free gingival graft for the increase of peri-implant attached keratinized mucosa decreased after guided bone regeneration
- The Clinical View of Immediate Implant Placement: Case Series
- Ridge Augmentation Using Vascularized Interpositional Periosteal- Connective Tissue (VIP-CT) in Conjunction with Anterior Implant Placement in Maxilla: Report of Three Cases
- Free Gingival Graft to Gain Peri-implant Keratinized Mucosa
- Bone-added osteotome sinus floor elevation with simultaneous placement of non-submerged sand blasted with large grit and acid etched implants: a 5-year radiographic evaluation