J Periodontal Implant Sci.
2014 Apr;44(2):50-56. 10.5051/jpis.2014.44.2.50.
Location of maxillary intraosseous vascular anastomosis based on the tooth position and height of the residual alveolar bone: computed tomographic analysis
- Affiliations
-
- 1Department of Periodontology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. pkoyang@skku.edu
- KMID: 1914504
- DOI: http://doi.org/10.5051/jpis.2014.44.2.50
Abstract
- PURPOSE
The aims of this study were to measure the distance of the intraosseous vascular anastomosis in the anterolateral wall of the maxillary sinus from different reference points, and to correlate the location of the intraosseous vascular anastomosis with the tooth position and the residual bone height of the maxilla.
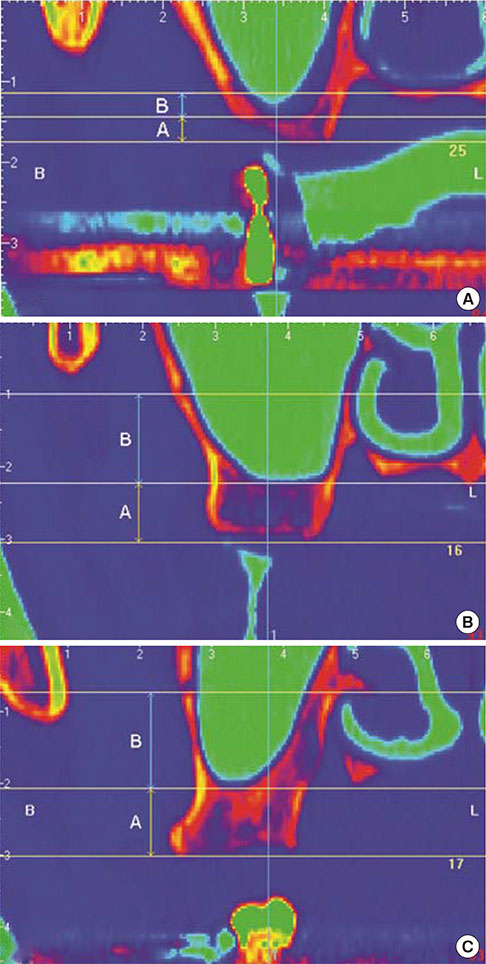
METHODS
Computed tomography (CT) images were taken from 283 patients undergoing dental implants placement in the posterior maxilla. Three horizontal lines were drawn at the ridge crest, maxillary sinus floor, and the position of the anastomosis. A vertical second line at the center of each tooth was drawn perpendicular to the horizontal lines. The distance from the ridge crest to the maxillary sinus floor and the distance from the maxillary sinus floor to the bony canal were measured from the intersections of the horizontal and vertical lines. The residual alveolar bone height was used to categorize three groups: group 1,<4 mm; group 2, between 4 and 8 mm; and group 3, >8 mm.
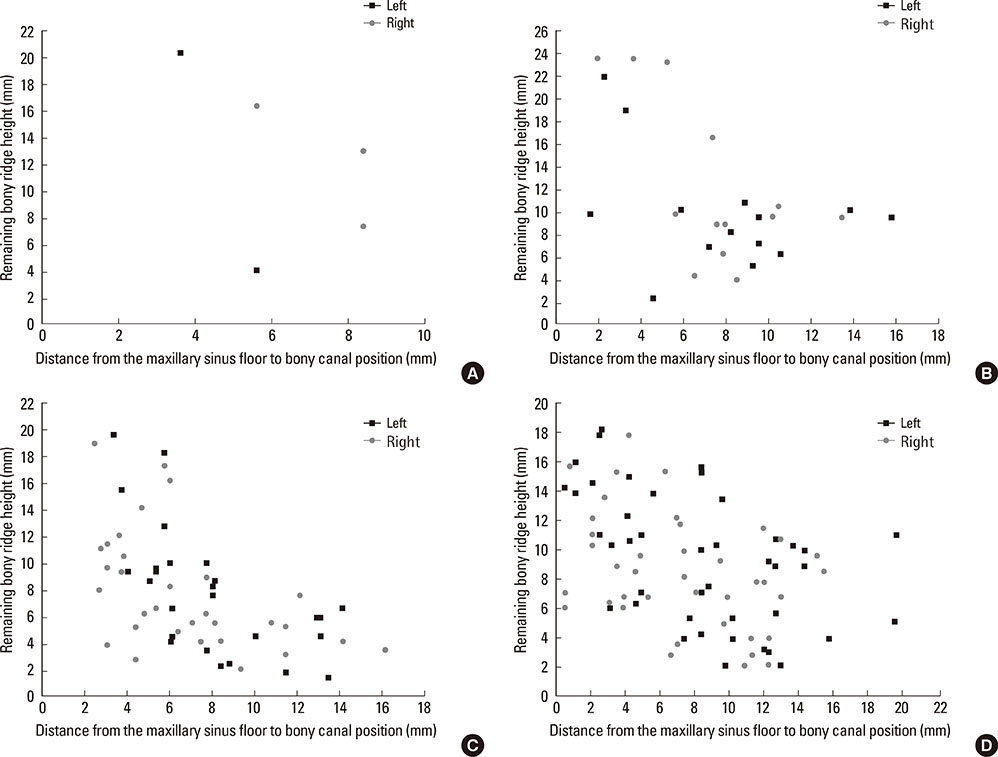
RESULTS
The residual bone height values of different tooth positions were significantly different (P=0.0002). The distance from the maxillary sinus floor to the intraosseous vascular anastomosis was significantly different between groups 1 and 3 (P=0.0039). At the molar sites, a moderate negative correlation was found between the residual bone height and the distance from the maxillary sinus floor to the intraosseous anastomosis. The distances of the alveolar ridge crest and the maxillary sinus from the intraosseous vascular anastomosis were not significantly different between sexes.
CONCLUSIONS
Within the limitations of this study, sites with a higher residual bone height in the molar regions were at a relatively high risk of artery damage during window osteotomy preparation; therefore, we recommend taking more precautions when using a lateral approach for sinus elevation.
Keyword
MeSH Terms
Figure
Reference
-
1. Garg AK, Quinones CR. Augmentation of the maxillary sinus: a surgical technique. Pract Periodontics Aesthet Dent. 1997; 9:211–219.2. Wallace SS, Froum SJ. Effect of maxillary sinus augmentation on the survival of endosseous dental implants: a systematic review. Ann Periodontol. 2003; 8:328–343.
Article3. Hong SB, Kim JS, Shin SI, Han JY, Herr Y, Chung JH. Clinical treatment of postoperative infection following sinus augmentation. J Periodontal Implant Sci. 2010; 40:144–149.
Article4. Flanagan D. Arterial supply of maxillary sinus and potential for bleeding complication during lateral approach sinus elevation. Implant Dent. 2005; 14:336–338.
Article5. Rosano G, Taschieri S, Gaudy JF, Del Fabbro M. Maxillary sinus vascularization: a cadaveric study. J Craniofac Surg. 2009; 20:940–943.6. Rosano G, Taschieri S, Gaudy JF, Weinstein T, Del Fabbro M. Maxillary sinus vascular anatomy and its relation to sinus lift surgery. Clin Oral Implants Res. 2011; 22:711–715.
Article7. Gaudy JF. Anatomie clinique. Rueil-Malmaison Cedex: Editions CdP;2003.8. Solar P, Geyerhofer U, Traxler H, Windisch A, Ulm C, Watzek G. Blood supply to the maxillary sinus relevant to sinus floor elevation procedures. Clin Oral Implants Res. 1999; 10:34–44.
Article9. Traxler H, Windisch A, Geyerhofer U, Surd R, Solar P, Firbas W. Arterial blood supply of the maxillary sinus. Clin Anat. 1999; 12:417–421.
Article10. Elian N, Wallace S, Cho SC, Jalbout ZN, Froum S. Distribution of the maxillary artery as it relates to sinus floor augmentation. Int J Oral Maxillofac Implants. 2005; 20:784–787.11. Guncu GN, Yildirim YD, Wang HL, Tozum TF. Location of posterior superior alveolar artery and evaluation of maxillary sinus anatomy with computerized tomography: a clinical study. Clin Oral Implants Res. 2011; 22:1164–1167.
Article12. Mardinger O, Abba M, Hirshberg A, Schwartz-Arad D. Prevalence, diameter and course of the maxillary intraosseous vascular canal with relation to sinus augmentation procedure: a radiographic study. Int J Oral Maxillofac Surg. 2007; 36:735–738.
Article13. Mardinger O, Namani-Sadan N, Chaushu G, Schwartz-Arad D. Morphologic changes of the nasopalatine canal related to dental implantation: a radiologic study in different degrees of absorbed maxillae. J Periodontol. 2008; 79:1659–1662.
Article14. Hur MS, Kim JK, Hu KS, Bae HE, Park HS, Kim HJ. Clinical implications of the topography and distribution of the posterior superior alveolar artery. J Craniofac Surg. 2009; 20:551–554.
Article15. Jung J, Yim JH, Kwon YD, Al-Nawas B, Kim GT, Choi BJ, et al. A radiographic study of the position and prevalence of the maxillary arterial endosseous anastomosis using cone beam computed tomography. Int J Oral Maxillofac Implants. 2011; 26:1273–1278.16. Lofthag-Hansen S, Grondahl K, Ekestubbe A. Cone-beam CT for preoperative implant planning in the posterior mandible: visibility of anatomic landmarks. Clin Implant Dent Relat Res. 2009; 11:246–255.
Article17. Park YB, Jeon HS, Shim JS, Lee KW, Moon HS. Analysis of the anatomy of the maxillary sinus septum using 3-dimensional computed tomography. J Oral Maxillofac Surg. 2011; 69:1070–1078.
Article18. Neugebauer J, Ritter L, Mischkowski RA, Dreiseidler T, Scherer P, Ketterle M, et al. Evaluation of maxillary sinus anatomy by cone-beam CT prior to sinus floor elevation. Int J Oral Maxillofac Implants. 2010; 25:258–265.19. Monsour PA, Dudhia R. Implant radiography and radiology. Aust Dent J. 2008; 53:Suppl 1. S11–S25.
Article20. Maestre-Ferrín L, Galan-Gil S, Carrillo-García C, Penarrocha-Diago M. Radiographic findings in the maxillary sinus: comparison of panoramic radiography with computed tomography. Int J Oral Maxillofac Implants. 2011; 26:341–346.21. Yang SM, Park SI, Kye SB, Shin SY. Computed tomographic assessment of maxillary sinus wall thickness in edentulous patients. J Oral Rehabil. 2012; 39:421–428.
Article22. Ella B, Sedarat C, Noble Rda C, Normand E, Lauverjat Y, Siberchicot F, et al. Vascular connections of the lateral wall of the sinus: surgical effect in sinus augmentation. Int J Oral Maxillofac Implants. 2008; 23:1047–1052.23. Lekholm U. Patient selection and preparation. In : Branemark PI, Zarb GA, Albrektsson T, editors. Tissue-integrated prostheses: osseointegration in clinical dentistry. Chicago: Quintessence;1985. p. 199–209.24. Kang SJ, Shin SI, Herr Y, Kwon YH, Kim GT, Chung JH. Anatomical structures in the maxillary sinus related to lateral sinus elevation: a cone beam computed tomographic analysis. Clin Oral Implants Res. 2013; 24:Suppl A100. 75–81.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Analysis of the root position and angulation of maxillary premolars in alveolar bone using cone-beam computed tomography
- Analysis of the root position of the maxillary incisors in the alveolar bone using cone-beam computed tomography
- Single-tooth implant restoration with alveolar bone augmentation in the maxillary anterior tooth region: a case report
- Healing pattern of the mucous membrane after tooth extraction in the maxillary sinus
- Cone-beam computed tomography characterization of the intraosseous vascular canal in the lateral wall of the maxillary antrum