Neurointervention.
2014 Sep;9(2):101-105. 10.5469/neuroint.2014.9.2.101.
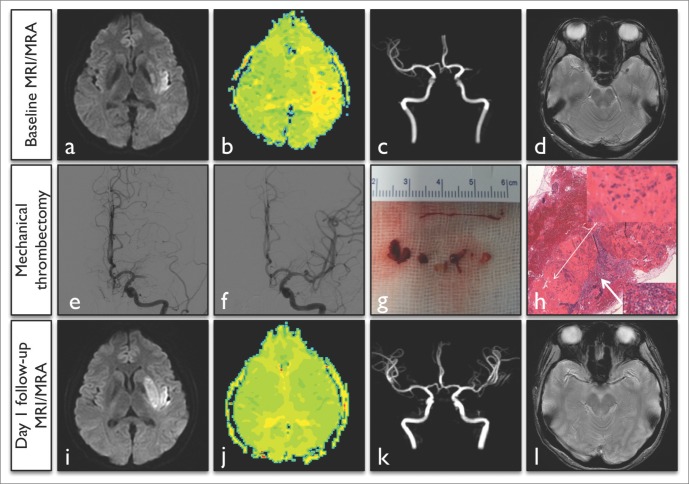
Forced Arterial Suction Thrombectomy of Septic Embolic Middle Cerebral Artery Occlusion Due to Infective Endocarditis: an Illustrative Case and Review of the Literature
- Affiliations
-
- 1Department of Neurology, Kyungpook National University Hospital, Daegu, Korea. yangha.hwang@gmail.com
- 2Department of Radiology, Kyungpook National University Hospital, Daegu, Korea.
- 3Department of Neurosurgery, Kyungpook National University Hospital, Daegu, Korea.
- 4Cerebrovascular Center, Kyungpook National University Hospital, Daegu, Korea.
- 5School of Medicine, Kyungpook National University, Daegu, Korea.
- KMID: 1910766
- DOI: http://doi.org/10.5469/neuroint.2014.9.2.101
Abstract
- In acute ischemic stroke patients with major intracranial vessel occlusion due to infective endocarditis, treatment modalities are not well established. A 40-year-old woman presented with acute stroke due to left middle cerebral artery occlusion. She was successfully treated with intra-arterial mechanical thrombectomy, and the subsequent clinical outcome was favorable. Pathological analysis of the retrieved clots showed septic thrombi containing gram-positive cocci. Based on literature review and the present case regarding treatment strategies for patients with septic embolic stroke, pharmacological thrombolysis might increase the risk of hemorrhagic complications, which might alter clinical outcome. Therefore, we can consider intra-arterial mechanical thrombectomy as a first-line treatment option in patients with acute stroke resulting from infective endocarditis.
MeSH Terms
Figure
Cited by 2 articles
-
Clinical challenges associated with the endovascular treatment of acute stroke in a patient with infective endocarditis
Emil Settarzade, Ahmet Peker, M. Akif Topcuoglu, E. Murat Arsava, Metin Demircin, Anıl Arat
J Cerebrovasc Endovasc Neurosurg. 2020;22(3):176-181. doi: 10.7461/jcen.2020.22.3.176.Clot Composition Analysis as a Diagnostic Tool to Gain Insight into Ischemic Stroke Etiology: A Systematic Review
Alicia Aliena-Valero, Júlia Baixauli-Martín, Germán Torregrosa, José I. Tembl, Juan B. Salom
J Stroke. 2021;23(3):327-342. doi: 10.5853/jos.2021.02306.
Reference
-
1. Ong E, Mechtouff L, Bernard E, Cho TH, Diallo LL, Nighoghossian N, et al. Thrombolysis for stroke caused by infective endocarditis: an illustrative case and review of the literature. J Neurol. 2013; 260:1339–1342. PMID: 23292203.
Article2. Bhuva P, Kuo SH, Claude Hemphill J, Lopez GA. Intracranial hemorrhage following thrombolytic use for stroke caused by infective endocarditis. Neurocrit Care. 2010; 12:79–82. PMID: 19688612.
Article3. Dababneh H, Hedna VS, Ford J, Taimeh Z, Peters K, Mocco J, et al. Endovascular intervention for acute stroke due to infective endocarditis: case report. Neurosurg Focus. 2012; 32:e1. PMID: 22296678.4. Sukumaran S, Jayadevan ER, Mandilya A, Sreedharan SE, Harikrishnan S, Radhakrishnan N, et al. Successful mechanical thrombectomy of acute middle cerebral artery occlusion due to vegetation from infective endocarditis. Neurol India. 2012; 60:239–240. PMID: 22626714.
Article5. Kan P, Webb S, Siddiqui AH, Levy EI. First reported use of retrievable stent technology for removal of a large septic embolus in the middle cerebral artery. World Neurosurg. 2012; 77:591.e1–591.e5. PMID: 22120371.
Article6. Kang DH, Hwang YH, Kim YS, Park J, Kwon O, Jung C. Direct thrombus retrieval using reperfusion catheter of the penumbra system: forced-suction thrombectomy in acute ischemic stroke. AJNR Am J Neuroradiol. 2011; 32:283–287. PMID: 21087940.7. Walker KA, Sampson JB, Skalabrin EJ, Majersik JJ. Clinical characteristics and thrombolytic outcomes of infective endocarditis-associated stroke. Neurohospitalist. 2012; 2:87–91. PMID: 23983869.
Article8. Hart RG, Foster JW, Luther MF, Kantar MC. Stroke in infective endocarditis. Stroke. 1990; 21:695–700. PMID: 2187287.
Article9. Ruttmann E, Willeit J, Ulmer H, Chevtchik O, Hofer D, Poewe W, et al. Neurological outcome of septic cardioembolic stroke after infective carditis. Stroke. 2006; 37:2094–2099. PMID: 16794213.10. Bain MD, Hussain MS, Gonugunta V, Katzan I, Gupta R. Successful recanalization of a septic embolus with a balloon mounted stent after failed mechanical thrombectomy. J Neuroimaging. 2011; 21:170–172. PMID: 20040014.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Mechanical Thrombectomy for Septic Embolism Secondary to Staphylococcus lugdunensis Bacteremia without Infective Endocarditis: A Case Report
- Motor Weakness of Contralateral Upper and Lower Limbs in a Patient with Septic Arthritis of the Knee Combined with Infective Endocarditis: Embolic Infarction Due to Infective Endocarditis
- A Case of Intracranial Infectious Aneurysm with Embolic Cerebral Infarction
- Delayed Development of Symptomatic Arterial Stenosis after a Mechanical Thrombectomy for an Acute Embolic Occlusion of the Middle Cerebral Artery
- Directly Retrieved Entire Clot from Forced Suction Thrombectomy Using the Penumbra System in Acute Middle Cerebral Artery Occlusion