Ann Surg Treat Res.
2014 Aug;87(2):108-111. 10.4174/astr.2014.87.2.108.
Salvage dual graft living donor liver transplantation after major hepatectomy
- Affiliations
-
- 1Division of Hepatobiliary Pancreas Surgery and Abdominal Organ Transplantation, Department of Surgery, Catholic University of Daegu School of Medicine, Daegu, Korea. dnchoi@cu.ac.kr
- KMID: 1882840
- DOI: http://doi.org/10.4174/astr.2014.87.2.108
Abstract
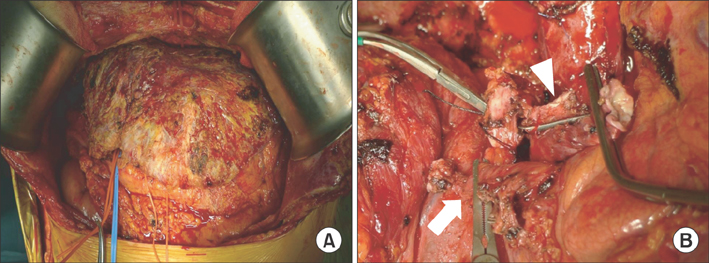
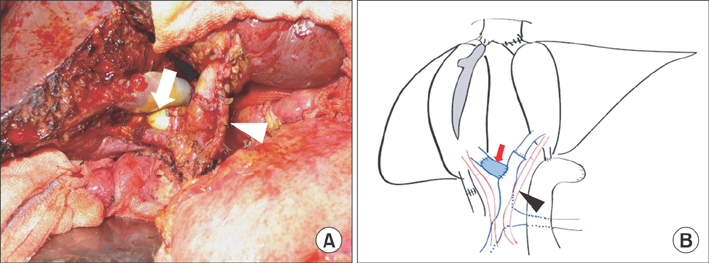
- Salvage living donor liver transplantation (LDLT) after major hepatectomy has been considered a challenging procedure due to operative complexity. We report a successful case of salvage dual graft LDLT after right hepatectomy. A 48-year-old male was transferred to Daegu Catholic University Medical Center because of duodenal variceal bleeding. He underwent right hepatectomy due to hepatocellular carcinoma four years prior. We performed LDLT with dual graft from his wife and sister. During operation, portal vein anastomosis of the right lobe graft was performed using an interposing cadaveric iliac vein graft and the right gastroepiploic artery was anastomosed to the hepatic artery of the left lobe graft. Adequate graft inflow was demonstrated by postoperative imaging studies. He has been doing well with normal graft function for 31 months. Salvage dual graft LDLT could be undertaken successfully in patients with prior major hepatectomy under accurate preoperative planning and proper surgical techniques.
Keyword
MeSH Terms
Figure
Reference
-
1. Hwang S, Lee SG, Moon DB, Ahn CS, Kim KH, Lee YJ, et al. Salvage living donor liver transplantation after prior liver resection for hepatocellular carcinoma. Liver Transpl. 2007; 13:741–746.2. Li HY, Wei YG, Yan LN, Li B. Salvage liver transplantation in the treatment of hepatocellular carcinoma: a meta-analysis. World J Gastroenterol. 2012; 18:2415–2422.3. Kim BW, Park YK, Kim YB, Wang HJ, Kim MW. Salvage liver transplantation for recurrent hepatocellular carcinoma after liver resection: feasibility of the Milan criteria and operative risk. Transplant Proc. 2008; 40:3558–3561.4. Moon D, Lee S, Hwang S, Park K, Kim K, Ahn C, et al. Umbilical portion of recipient's left portal vein: a useful vascular conduit in dual living donor liver transplantation for the thrombosed portal vein. Liver Transpl. 2004; 10:802–806.5. Wu L, Hu A, Tam N, Zhang J, Lin M, Guo Z, et al. Salvage liver transplantation for patients with recurrent hepatocellular carcinoma after curative resection. PLoS One. 2012; 7:e41820.6. Adam R, Azoulay D, Castaing D, Eshkenazy R, Pascal G, Hashizume K, et al. Liver resection as a bridge to transplantation for hepatocellular carcinoma on cirrhosis: a reasonable strategy? Ann Surg. 2003; 238:508–518.7. Belghiti J, Cortes A, Abdalla EK, Regimbeau JM, Prakash K, Durand F, et al. Resection prior to liver transplantation for hepatocellular carcinoma. Ann Surg. 2003; 238:885–892.8. Hu Z, Wang W, Li Z, Ye S, Zheng SS. Recipient outcomes of salvage liver transplantation versus primary liver transplantation: a systematic review and meta-analysis. Liver Transpl. 2012; 18:1316–1323.9. Lee JH, Oh DY, Seo JW, Moon SH, Rhie JW, Ahn ST. Versatility of right gastroepiploic and gastroduodenal arteries for arterial reconstruction in adult living donor liver transplantation. Transplant Proc. 2011; 43:1716–1719.10. Ahn CS, Hwang S, Moon DB, Song GW, Ha TY, Park GC, et al. Right gastroepiploic artery is the first alternative inflow source for hepatic arterial reconstruction in living donor liver transplantation. Transplant Proc. 2012; 44:451–453.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Assessment of Technical Feasibility of Living Donor Liver Transplantation after Prior Major Liver Resection for Hepatocellular Carcinoma
- Pure laparoscopic donor right hepatectomy for adult living donor liver transplantation: initial report from Southeast Asia liver transplant center
- Technical refinement of the anterior sectional drainage in right liver transplantation: a single center experience
- Left at right heterotopic implantation of left liver graft in adult-to-adult living donor liver transplantation: the technical concern for decision-making
- Laparoscopic living donor hepatectomy