Brain Tumor Res Treat.
2015 Apr;3(1):39-43. 10.14791/btrt.2015.3.1.39.
Thrombosed Large Middle Cerebral Artery Aneurysm Mimicking an Intra-Axial Brain Tumor: Case Report and Review of Literature
- Affiliations
-
- 1Department of Neurosurgery, Seoul St. Mary's Hospital, The Catholic University of Korea College of Medicine, Seoul, Korea. jhyun@catholic.ac.kr
- KMID: 1882009
- DOI: http://doi.org/10.14791/btrt.2015.3.1.39
Abstract
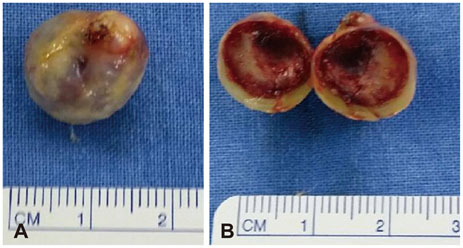
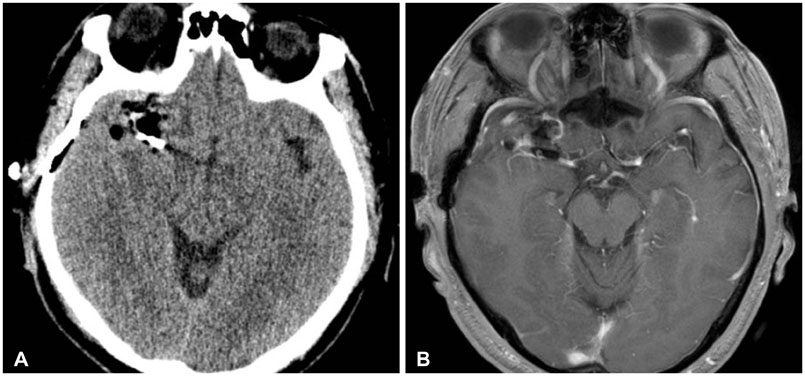
- This case report presents a fully thrombosed large aneurysm of middle cerebral artery mimicking an intra-axial brain tumor in a 54-year-old male patient. A small mass like lesion was found incidentally in right frontal area. Brain magnetic resonance image showed dark signal intensity on T2-weighted images and peripheral high signal intensity on T1-weighted images with peripheral rim enhancement. We considered intra-axial tumors such as glioma or metastatic tumor as a differential diagnosis. The lesion was approached transcortically, and intraoperatively, the lesion was found to be a large thrombosed aneurysm originating from the lateral lenticulostriate artery of right middle cerebral artery. One vascular clip was applied at the parent artery, and the thrombosed aneurysm was totally removed. There have been many reports of other intracranial lesions wrongly diagnosed as intracranial neoplasms. And thrombosed aneurysms mimicking intracranial neoplasm have been reported in 4 cases previously. According to those case reports, there were no efficient imaging tools to differentiate between these thrombosed aneurysms and intracranial neoplasms. We reviewed those reports and considered about the efficient method to diagnosed accurately before surgery. To sum up, when a patient presents with an intracranial lesion lying on the course of major or distal cerebral arteries, the surgeon should have thrombosed aneurysm in mind as one of the differential diagnosis and be prepared when surgically treating such lesions.
MeSH Terms
Figure
Reference
-
1. Heros RC, Fritsch MJ. Surgical management of middle cerebral artery aneurysms. Neurosurgery. 2001; 48:780–785.
Article2. Rinne J, Hernesniemi J, Niskanen M, Vapalahti M. Analysis of 561 patients with 690 middle cerebral artery aneurysms: anatomic and clinical features as correlated to management outcome. Neurosurgery. 1996; 38:2–11.
Article3. Brownlee RD, Tranmer BI, Sevick RJ, Karmy G, Curry BJ. Spontaneous thrombosis of an unruptured anterior communicating artery aneurysm. An unusual cause of ischemic stroke. Stroke. 1995; 26:1945–1949.
Article4. Jellinger K. Pathology of intracerebral hemorrhage. Zentralbl Neurochir. 1977; 38:29–42.5. Wiebers DO, Whisnant JP, Huston J 3rd, et al. Unruptured intracranial aneurysms: natural history, clinical outcome, and risks of surgical and endovascular treatment. Lancet. 2003; 362:103–110.
Article6. Hosoda K, Fujita S, Kawaguchi T, Shose Y, Hamano S. Saccular aneurysms of the proximal (M1) segment of the middle cerebral artery. Neurosurgery. 1995; 36:441–446.
Article7. Gandhi CD, Gilad R, Patel AB, Haridas A, Bederson JB. Treatment of ruptured lenticulostriate artery aneurysms. J Neurosurg. 2008; 109:28–37.
Article8. Morley TP, Barr HW. Giant intracranial aneurysms: diagnosis, course, and management. Clin Neurosurg. 1969; 16:73–94.
Article9. Whittle IR, Dorsch NW, Besser M. Spontaneous thrombosis in giant intracranial aneurysms. J Neurol Neurosurg Psychiatry. 1982; 45:1040–1047.
Article10. Black SP, German WJ. Observations on the relationship between the volume and the size of the orifice of experimental aneurysms. J Neurosurg. 1960; 17:984–990.
Article11. Jaimovich SG, Thea VC, Guevara M, Gardella JL. Cavernous sinus tuberculoma mimicking a neoplasm: case report, literature review, and diagnostic and treatment suggestions for tuberculomas in rare locations. Surg Neurol Int. 2013; 4:158.
Article12. Grayeli AB, Redondo A, Salama J, Rey A. Tuberculoma of the cavernous sinus: case report. Neurosurgery. 1998; 42:179–181.
Article13. Woo PY, Ko NM, Chan KY. Thrombosed large distal posterior inferior cerebellar artery aneurysm mimicking an infratentorial ependymoma. Case Rep Neurol Med. 2014; 2014:435953.
Article14. Päsler D, Baldauf J, Runge U, Schroeder HW. Intrameatal thrombosed anterior inferior cerebellar artery aneurysm mimicking a vestibular schwannoma. J Neurosurg. 2011; 114:1057–1060.
Article15. Fifi JT, Komotar R, Meyers P, Khandji A, Tanji K, Connolly ES. Restricted diffusion in a thrombosed anterior cerebral artery aneurysm mimicking a dermoid cyst. J Neuroimaging. 2012; 22:85–88.
Article16. Lan ZG, Ma L, Duan J, You C. A fully thrombosed giant posterior inferior cerebellar aneurysm mimicking an intracranial tumour in a child. Br J Neurosurg. 2012; 26:888–890.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Huge Intramural Hematoma in a Thrombosed Middle Cerebral Artery Aneurysm: A Case Report
- Dissecting Aneurysm of the Anterior Cerebral Artery: Report of Two Cases
- Duplication of the Middle Cerebral Artery: Case Report
- Endovascular Treatment of a Large Partially Thrombosed Basilar Tip Aneurysm
- Magnetization Transfer Contrast Angiography for Organized Thrombosed Intracranial Aneurysm in TOF MR Angiography: a Case Report