Korean Circ J.
2014 Jan;44(1):22-29. 10.4070/kcj.2014.44.1.22.
Prognostic Implication of QRS Variability during Hospitalization in Patients with Acute Decompensated Heart Failure
- Affiliations
-
- 1Department of Internal Medicine, Seoul National University Hospital, Seoul, Korea. choiek17@snu.ac.kr
- 2Cardiovascular Center, Seoul National University Bundang Hospital, Seongnam, Korea.
- KMID: 1859238
- DOI: http://doi.org/10.4070/kcj.2014.44.1.22
Abstract
- BACKGROUND AND OBJECTIVES
Heart failure (HF) patients display more varied QRS duration. We investigated whether QRS variability during hospitalization for acute decompensated HF is associated with poor clinical outcomes after discharge.
SUBJECTS AND METHODS
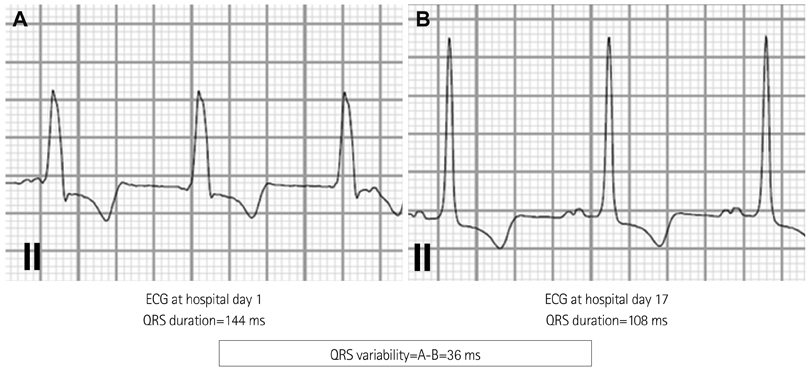
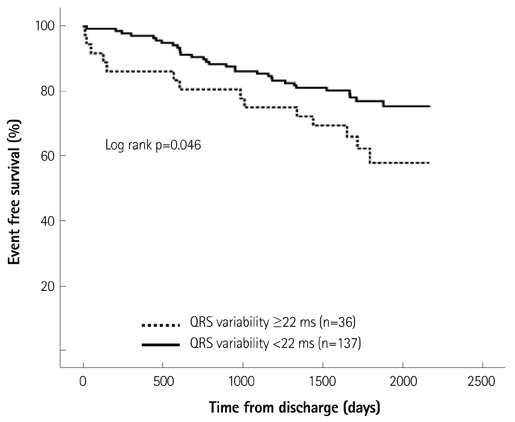
One hundred seventy three patients (64% males; age 60+/-13 years) admitted for acute decompensated HF with severe left ventricular (LV) dysfunction (LV ejection fraction < or =35%) were consecutively enrolled. QRS variability was calculated by the difference between maximum and minimum QRS duration acquired during hospitalization. The prognostic implications on composite endpoints of death or urgent heart transplantation were analyzed.
RESULTS
Forty-two patients (24.3%) died and three patients (1.7%) underwent urgent heart transplantation during the follow-up of 51+/-18 months. Patients who reached composite endpoints (n=45) showed greater QRS variability than those who did not (n=128) (20+/-23 ms vs. 14+/-14 ms, p=0.046). Patients who had high QRS variability (more than 22 ms; n=36) tended to have a higher event rate than those with QRS variability <22 ms {39% vs. 23%, hazard ratio (HR), 1.88; 95% confidence interval (CI) 1.001-3.539, p=0.05}. Adjusting with other variables, high QRS variability was an independent predictor for composite outcome (HR 1.94; 95% CI 1.023-3.683, p=0.042).
CONCLUSION
QRS variability measured during hospitalization for acute decompensated HF has a prognostic impact in HF patients with severe LV dysfunction.
MeSH Terms
Figure
Reference
-
1. Cleland JG, Gemmell I, Khand A, Boddy A. Is the prognosis of heart failure improving? Eur J Heart Fail. 1999; 1:229–241.2. Shenkman HJ, Pampati V, Khandelwal AK, et al. Congestive heart failure and QRS duration: establishing prognosis study. Chest. 2002; 122:528–534.3. Kashani A, Barold SS. Significance of QRS complex duration in patients with heart failure. J Am Coll Cardiol. 2005; 46:2183–2192.4. Murkofsky RL, Dangas G, Diamond JA, Mehta D, Schaffer A, Ambrose JA. A prolonged QRS duration on surface electrocardiogram is a specific indicator of left ventricular dysfunction. J Am Coll Cardiol. 1998; 32:476–482.5. Sandhu R, Bahler RC. Prevalence of QRS prolongation in a community hospital cohort of patients with heart failure and its relation to left ventricular systolic dysfunction. Am J Cardiol. 2004; 93:244–246.6. Brilakis ES, Mavrogiorgos NC, Kopecky SL, et al. Usefulness of QRS duration in the absence of bundle branch block as an early predictor of survival in non-ST elevation acute myocardial infarction. Am J Cardiol. 2002; 89:1013–1018.7. Kalra PR, Sharma R, Shamim W, et al. Clinical characteristics and survival of patients with chronic heart failure and prolonged QRS duration. Int J Cardiol. 2002; 86:225–231.8. Iuliano S, Fisher SG, Karasik PE, Fletcher RD, Singh SN. Department of Veterans Affairs Survival Trial of Antiarrhythmic Therapy in Congestive Heart Failure. QRS duration and mortality in patients with congestive heart failure. Am Heart J. 2002; 143:1085–1091.9. Bleeker GB, Schalij MJ, Molhoek SG, et al. Relationship between QRS duration and left ventricular dyssynchrony in patients with end-stage heart failure. J Cardiovasc Electrophysiol. 2004; 15:544–549.10. Cleland JG, Daubert JC, Erdmann E, et al. The effect of cardiac resynchronization on morbidity and mortality in heart failure. N Engl J Med. 2005; 352:1539–1549.11. Sipahi I, Carrigan TP, Rowland DY, Stambler BS, Fang JC. Impact of QRS duration on clinical event reduction with cardiac resynchronization therapy: meta-analysis of randomized controlled trials. Arch Intern Med. 2011; 171:1454–1462.12. Aranda JM, Carlson ER, Pauly DF, et al. QRS duration variability in patients with heart failure. Am J Cardiol. 2002; 90:335–337.13. Wang NC, Maggioni AP, Konstam MA, et al. Clinical implications of QRS duration in patients hospitalized with worsening heart failure and reduced left ventricular ejection fraction. JAMA. 2008; 299:2656–2666.14. Barsheshet A, Goldenberg I, Garty M, et al. Relation of bundle branch block to long-term (four-year) mortality in hospitalized patients with systolic heart failure. Am J Cardiol. 2011; 107:540–544.15. McCullough PA, Hassan SA, Pallekonda V, et al. Bundle branch block patterns, age, renal dysfunction, and heart failure mortality. Int J Cardiol. 2005; 102:303–308.16. Baldasseroni S, Gentile A, Gorini M, et al. Intraventricular conduction defects in patients with congestive heart failure: left but not right bundle branch block is an independent predictor of prognosis. A report from the Italian Network on Congestive Heart Failure (IN-CHF database). Ital Heart J. 2003; 4:607–613.17. Gheorghiade M, Pang PS. Acute heart failure syndromes. J Am Coll Cardiol. 2009; 53:557–573.18. Lee CW, Lee JH, Lim TH, et al. Prognostic significance of cerebral metabolic abnormalities in patients with congestive heart failure. Circulation. 2001; 103:2784–2787.19. Gulati A, Ismail TF, Jabbour A, et al. The prevalence and prognostic significance of right ventricular systolic dysfunction in nonischemic dilated cardiomyopathy. Circulation. 2013; 128:1623–1633.20. Parameshwar J, Keegan J, Sparrow J, Sutton GC, Poole-Wilson PA. Predictors of prognosis in severe chronic heart failure. Am Heart J. 1992; 123:421–426.21. Hunt SA, Abraham WT, Chin MH, et al. ACC/AHA 2005 Guideline Update for the Diagnosis and Management of Chronic Heart Failure in the Adult: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Update the 2001 Guidelines for the Evaluation and Management of Heart Failure): developed in collaboration with the American College of Chest Physicians and the International Society for Heart and Lung Transplantation: endorsed by the Heart Rhythm Society. Circulation. 2005; 112:e154–e235.22. Shamim W, Yousufuddin M, Cicoria M, Gibson DG, Coats AJ, Henein MY. Incremental changes in QRS duration in serial ECGs over time identify high risk elderly patients with heart failure. Heart. 2002; 88:47–51.23. Xiao HB, Roy C, Fujimoto S, Gibson DG. Natural history of abnormal conduction and its relation to prognosis in patients with dilated cardiomyopathy. Int J Cardiol. 1996; 53:163–170.24. Leclercq C, Cazeau S, Le Breton H, et al. Acute hemodynamic effects of biventricular DDD pacing in patients with end-stage heart failure. J Am Coll Cardiol. 1998; 32:1825–1831.25. Horwich T, Lee SJ, Saxon L. Usefulness of QRS prolongation in predicting risk of inducible monomorphic ventricular tachycardia in patients referred for electrophysiologic studies. Am J Cardiol. 2003; 92:804–809.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Medical Treatment of Acute Decompensated Heart Failure Syndrome
- QRS complex
- Worsening Renal Function during Acute Decompensated Heart Failure: A Bad Signal Never to Ignore
- Prognostic Value of Short-Term Followup of Multiple Biomarkers After Discharge in Hospitalized Patients With Acute Heart Failure (POSTBIO-HF): Rationale and Study Design
- Pharmacological Treatment of Heart Failure