Korean Circ J.
2014 Jan;44(1):10-15. 10.4070/kcj.2014.44.1.10.
Myeloperoxidase Is Not Useful for Detecting Stress Inducible Myocardial Ischemia but May Be Indicative of the Severity of Coronary Artery Disease
- Affiliations
-
- 1Department of Cardiology, Medizinische Klinik I, Munich, Germany. haeyoung.sohn@med.uni-muenchen.de
- 2Department of Nuclear Medicine, University Hospital of the Ludwig Maximilian University of Munich, Munich, Germany.
- KMID: 1859236
- DOI: http://doi.org/10.4070/kcj.2014.44.1.10
Abstract
- BACKGROUND AND OBJECTIVES
Elevated levels of myeloperoxidase (MPO) have been found in patients in different stages of coronary artery disease (CAD). The aim of this study was to assess whether the MPO liberation is increased by stress inducible myocardial ischemia and could be used to improve the diagnostic accuracy of non-invasive evaluation for myocardial ischemia.
SUBJECTS AND METHODS
Seventy-six patients with suspected myocardial ischemia who underwent stress myocardial perfusion scintigraphy (MPS) were enrolled. 59 patients with an acute coronary syndrome (ACS) who received a percutaneous coronary intervention along with 12 healthy volunteers were also included in the study. In every subject the MPO plasma levels were assessed by enzyme linked immunosorbent assay. In patients undergoing MPS, the MPO levels were measured serially before and after the stress testing.
RESULTS
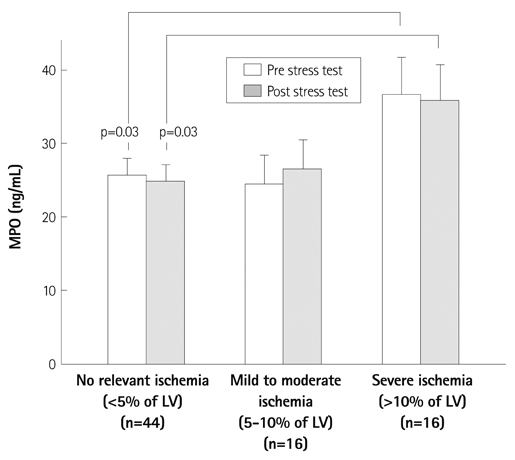
Of the 76 patients undergoing MPS, 38 were diagnosed with a stress inducible myocardial ischemia. The patients with a stress induced ischemia had significantly higher basal MPO levels than those without it (32+/-3 ng/mL vs. 24+/-4 ng/mL, p=0.03). However, there was no relevant change in the MPO levels after the stress test compared to the baseline. The patients with ACS showed significantly higher MPO levels than the patients undergoing MPS (131+/-14 ng/mL vs. 28+/-2 ng/mL, p<0.01) and the healthy subjects (131+/-14 ng/mL vs. 26+/-2 ng/mL, p<0.01).
CONCLUSION
Since the MPO plasma levels did not increase after the stress MPS, MPO appears not to be a useful biomarker for detecting a stress inducible myocardial ischemia. Yet, the MPO levels correlate with the different stages of CAD and may hold significance as an indicator for its clinical severity.
Keyword
MeSH Terms
Figure
Reference
-
1. Klebanoff SJ. Myeloperoxidase: friend and foe. J Leukoc Biol. 2005; 77:598–625.2. Brennan ML, Hazen SL. Emerging role of myeloperoxidase and oxidant stress markers in cardiovascular risk assessment. Curr Opin Lipidol. 2003; 14:353–359.3. Ndrepepa G, Braun S, Mehilli J, von Beckerath N, Schömig A, Kastrati A. Myeloperoxidase level in patients with stable coronary artery disease and acute coronary syndromes. Eur J Clin Invest. 2008; 38:90–96.4. Zhang R, Brennan ML, Fu X, et al. Association between myeloperoxidase levels and risk of coronary artery disease. JAMA. 2001; 286:2136–2142.5. Eggers KM, Dellborg M, Johnston N, et al. Myeloperoxidase is not useful for the early assessment of patients with chest pain. Clin Biochem. 2010; 43:240–245.6. Sawicki M, Sypniewska G, Kozinski M, et al. Diagnostic efficacy of myeloperoxidase for the detection of acute coronary syndromes. Eur J Clin Invest. 2011; 41:667–671.7. Rebeiz AG, Tamim HM, Sleiman RM, et al. Plasma myeloperoxidase concentration predicts the presence and severity of coronary disease in patients with chest pain and negative troponin-T. Coron Artery Dis. 2011; 22:553–558.8. Brennan ML, Penn MS, Van Lente F, et al. Prognostic value of myeloperoxidase in patients with chest pain. N Engl J Med. 2003; 349:1595–1604.9. Baldus S, Heeschen C, Meinertz T, et al. Myeloperoxidase serum levels predict risk in patients with acute coronary syndromes. Circulation. 2003; 108:1440–1445.10. Meuwese MC, Stroes ES, Hazen SL, et al. Serum myeloperoxidase levels are associated with the future risk of coronary artery disease in apparently healthy individuals: the EPIC-Norfolk Prospective Population Study. J Am Coll Cardiol. 2007; 50:159–165.11. Mocatta TJ, Pilbrow AP, Cameron VA, et al. Plasma concentrations of myeloperoxidase predict mortality after myocardial infarction. J Am Coll Cardiol. 2007; 49:1993–2000.12. Sugiyama S, Kugiyama K, Aikawa M, Nakamura S, Ogawa H, Libby P. Hypochlorous acid, a macrophage product, induces endothelial apoptosis and tissue factor expression: involvement of myeloperoxidasemediated oxidant in plaque erosion and thrombogenesis. Arterioscler Thromb Vasc Biol. 2004; 24:1309–1314.13. Daugherty A, Dunn JL, Rateri DL, Heinecke JW. Myeloperoxidase, a catalyst for lipoprotein oxidation, is expressed in human atherosclerotic lesions. J Clin Invest. 1994; 94:437–444.14. Buffon A, Biasucci LM, Liuzzo G, D'Onofrio G, Crea F, Maseri A. Widespread coronary inflammation in unstable angina. N Engl J Med. 2002; 347:5–12.15. Naruko T, Ueda M, Haze K, et al. Neutrophil infiltration of culprit lesions in acute coronary syndromes. Circulation. 2002; 106:2894–2900.16. Jordan JE, Zhao ZQ, Vinten-Johansen J. The role of neutrophils in myocardial ischemia-reperfusion injury. Cardiovasc Res. 1999; 43:860–878.17. Hansen PR. Role of neutrophils in myocardial ischemia and reperfusion. Circulation. 1995; 91:1872–1885.18. Klocke FJ, Baird MG, Lorell BH, et al. ACC/AHA/ASNC guidelines for the clinical use of cardiac radionuclide imaging--executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/ASNC Committee to Revise the 1995 Guidelines for the Clinical Use of Cardiac Radionuclide Imaging). J Am Coll Cardiol. 2003; 42:1318–1333.19. Slomka PJ, Hurwitz GA, Stephenson J, Cradduck T. Automated alignment and sizing of myocardial stress and rest scans to three-dimensional normal templates using an image registration algorithm. J Nucl Med. 1995; 36:1115–1122.20. Wiersma JJ, Verberne HJ, Meuwese MC, et al. Myeloperoxidase is not associated with scintigraphic myocardial perfusion abnormalities in type 2 diabetic patients with mild stable anginal complaints. Clin Chim Acta. 2011; 412:86–90.21. Biasucci LM, D'Onofrio G, Liuzzo G, et al. Intracellular neutrophil myeloperoxidase is reduced in unstable angina and acute myocardial infarction, but its reduction is not related to ischemia. J Am Coll Cardiol. 1996; 27:611–616.22. Yunoki K, Naruko T, Komatsu R, et al. Relation of elevated levels of plasma myeloperoxidase to impaired myocardial microcirculation after reperfusion in patients with acute myocardial infarction. Am J Cardiol. 2010; 105:922–929.23. Sugiyama S, Okada Y, Sukhova GK, Virmani R, Heinecke JW, Libby P. Macrophage myeloperoxidase regulation by granulocyte macrophage colony-stimulating factor in human atherosclerosis and implications in acute coronary syndromes. Am J Pathol. 2001; 158:879–891.24. Aminian A, Boudjeltia KZ, Babar S, et al. Coronary stenting is associated with an acute increase in plasma myeloperoxidase in stable angina patients but not in patients with acute myocardial infarction. Eur J Intern Med. 2009; 20:527–532.25. Marshall CJ, Nallaratnam M, Mocatta T, et al. Factors influencing local and systemic levels of plasma myeloperoxidase in ST-segment elevation acute myocardial infarction. Am J Cardiol. 2010; 106:316–322.26. Rudolph V, Steven D, Gehling UM, et al. Coronary plaque injury triggers neutrophil activation in patients with coronary artery disease. Free Radic Biol Med. 2007; 42:460–465.27. Naruko T, Furukawa A, Yunoki K, et al. Increased expression and plasma levels of myeloperoxidase are closely related to the presence of angiographically-detected complex lesion morphology in unstable angina. Heart. 2010; 96:1716–1722.28. Ferrante G, Nakano M, Prati F, et al. High levels of systemic myeloperoxidase are associated with coronary plaque erosion in patients with acute coronary syndromes: a clinicopathological study. Circulation. 2010; 122:2505–2513.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Functional Angioplasty: Definitions, Historical Overview, and Future Perspectives
- Comparison of Stress-rest and Rest-stress One Day Myocardial Perfusion Scintigraphies in Detecting Coronary Artery Diseases
- 2 Case of Coronary Artery-to-Left Ventricular Fistulae
- Evaluation of Myocardial Ischemia Using Coronary Computed Tomography Angiography in Patients with Stable Angina
- Assessment of Myocardial Ischemia Using Stress Perfusion Cardiovascular Magnetic Resonance