Korean Circ J.
2007 Feb;37(2):51-57. 10.4070/kcj.2007.37.2.51.
The Effects of Trimetazidine on the Enhancement Pattern of Multi-detector Computed Tomography in a Porcine Myocardial Infarction Model
- Affiliations
-
- 1The Heart Center of Diagnostic Radiology, Chonnam National University Hospital, Gwangju, Korea. myungho@chollian.net
- 2Department of Diagnostic Radiology, Chonnam National University Hospital, Gwangju, Korea.
- 3Chonnam National University Research Institute of Medical Sciences, Gwangju, Korea.
- KMID: 1859081
- DOI: http://doi.org/10.4070/kcj.2007.37.2.51
Abstract
-
BACKGROUND AND OBJECTIVES: There is increasing evidence to suggest that trimetazidine (TMZ) has the ability to improve ischemic heart failure by way of optimizing the heart's energy metabolism. The aim of this study was to examine the changes of the myocardial enhancement pattern by using two-phase, contrast enhanced, ECG-gated, multi-detector computed tomography (MDCT) after the administration of TMZ in a porcine myocardial infarction model.
SUBJECTS AND METHODS
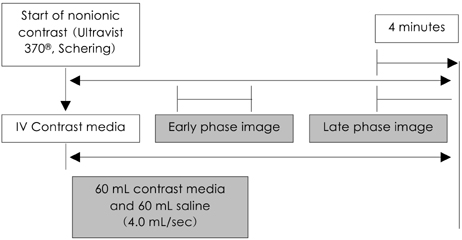
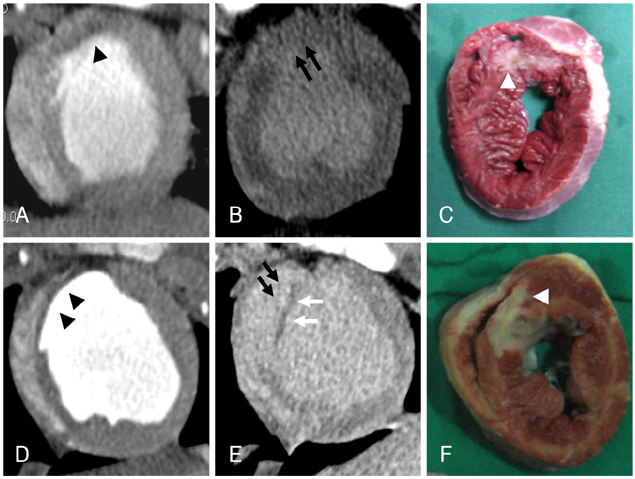
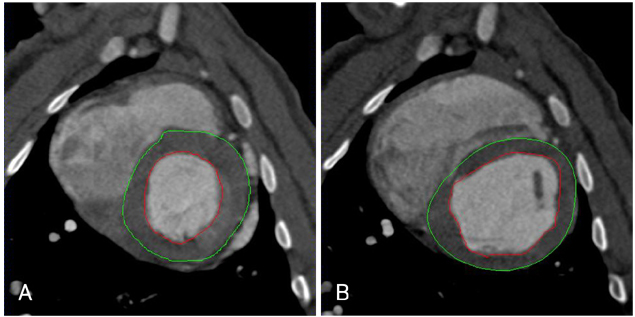
The porcine myocardial infarction model was created by balloon occlusion of the left anterior descending coronary artery. We randomized the swine into two groups: group I (n=7: aspirin only) and group II (n=7: aspirin plus 1 mg/kg TMZ for 4 weeks). Echocardiography and MDCT were performed and the ejection fraction (EF, %), end-systolic volume (ESV, mL) and end-diastolic volume (EDV, mL) were measured at 28 days after induction of myocardial infarction. Three enhancement patterns, including the early arterial phase defect (ED), the 4-min late enhancement (LE) and the residual defect (RD), were also investigated and those were described as class I [ED (-), RD (-), LE (+/-)], class II [ED (+), RD (-), LE (+)], and class III [ED (+), RD (+), LE (+)]. We performed histopathologic examination after sacrificing the animals.
RESULTS
The baseline and follow-up echocardiography at 4 weeks after the induction of MI demonstrated no significant differences between the two groups. The LV indices by MDCT were also similar between the two groups (group I: EF, ESV and EDV=46.0+/-12.5%, 35.9+/-23.0 mL and 69.0+/-40.2 mL, respectively, group II: EF, ESV and EDV=49.8+/-13.2%, 43.8+/-23.1 mL and 82.8+/-24.6 mL, respectively, p=NS). The percent wall thickness was similar (69.1+/-19.6% vs. 64.9+/-10.5%, respectively, p=NS), but the enhancement pattern was different between the two groups (group I: class I, II and III=0 (0%), 0 (0%): and 7 (100%) respectively, group II: class I, II and III=0 (0%), 2 (28.6%) and 5 (71.4%), respectively, p<0.001). The volume of tissue that lacked triphenyl tetrazolium chloride was similar between two groups (8.4+/-1.9% vs. 7.3+/-2.6%, respectively, p=NS).
CONCLUSION
TMZ administration produced different enhancement patterns on MDCT. This result suggests that TMZ administration can reduce the residual defect in a porcine myocardial infarction model. Although further experiments are needed for determining the effect of TMZ on reducing the irreversible area of infarcted myocardium, this is the first report that proved the beneficial effect of TMZ by performing MDCT.
MeSH Terms
Figure
Reference
-
1. Lee L, Horowitz J, Frenneaux M. Metabolic manipulation in ischemic heart disease, a novel approach to treatment. Eur Heart J. 2004. 25:634–641.2. De Luca G, Suryapranata H, Stone GW, et al. Abciximab as adjunctive therapy to reperfusion in acute ST-segment elevation myocardial Infarction: a meta-analysis of randomized trials. JAMA. 2005. 293:1759–1765.3. O'Meara E, McMurray JJ. Myocardial metabolic manipulation: a new therapeutic approach in heart failure? Heart. 2005. 91:131–132.4. Di Napoli P, Taccardi AA, Barsotti A. Long term cardioprotective action of trimetazidine and potential effect on the inflammatory process in patients with ischaemic dilated cardiomyopathy. Heart. 2005. 91:161–165.5. Kantor PF, Lucien A, Kozak R, Lopaschuk GD. The antianginal drug trimetazidine shifts cardiac energy metabolism from fatty acid oxidation to glucose oxidation by inhibiting mitochondrial long-chain 3-ketoacyl coenzyme A thiolase. Circ Res. 2000. 86:580–588.6. Liu Q, Docherty JC, Rendell JC, Clanachan AS, Lopaschuk GD. High levels of fatty acids delay the recovery of intracellular pH and cardiac efficiency in post-ischemic hearts by inhibiting glucose oxidation. J Am Coll Cardiol. 2002. 39:718–725.7. Orchard CH, Kentish JC. Effects of changes of pH on the contractile function of cardiac muscle. Am J Physiol. 1990. 258:C967–C981.8. Belardinelli R, Purcaro A. Effects of trimetazidine on the contractile response of chronically dysfunctional myocardium to low-dose dobutamine in ischaemic cardiomyopathy. Eur Heart J. 2001. 22:2164–2170.9. Manchanda SC, Krishnaswani S. Combination treatment with trimetazidine and diltiazem in stable angina pectoris. Heart. 1997. 78:353–357.10. Rhew JY, Jeong MH, Lee SR, et al. The effects of radiation using Ho-166 on endothelial function in a porcine coronary model. Korean Circ J. 2002. 32:118–124.11. Kim W, Jeong MH, Hong YJ, et al. A new porcine model of ischemic heart failure and pathologic findings by intra-coronary injection of ethanol. Korean Circ J. 2004. 34:900–908.12. Lim SY, Jeong MH, Ahn YG, et al. The effect of mesenchymal stem cells transduced with Akt in a porcine myocardial infarction model. Korean Circ J. 2005. 35:734–741.13. Sahn DJ, DeMaria A, Kisslo J, Weyman A. Recommendation regarding quantitation in M-mode echocardiography: results of a survey of echocardiographic measurements. Circulation. 1978. 58:1072–1083.14. Hoffmann U, Millea R, Enzweiler C, et al. Acute myocardial infarction: contrast-enhanced multi-detector row CT in a porcine model. Radiology. 2004. 231:697–701.15. Mahnken AH, Bruners P, Katoh M, Wildberger JE, Gunther RW, Buecker A. Dynamic multi-section CT imaging in acute myocardial infarction: preliminary animal experience. Eur Radiol. 2006. 16:746–752.16. Koyama Y, Mochizuki T, Higaki J. Computed tomography assessment of myocardial perfusion, viability, and function. J Magn Reson Imaging. 2004. 19:800–815.17. Koyama Y, Matsuoka H, Mochizuki T, et al. Assessment of reperfused acute myocardial infarction with two-phase contrast-enhanced helical CT: prediction of left ventricular function and wall thickness. Radiology. 2005. 235:804–811.18. Lardo AC, Cordeiro MA, Silva C, et al. Contrast-enhanced multidetector computed tomography viability imaging after myocardial infarction: characterization of myocyte death, microvascular obstruction, and chronic scar. Circulation. 2006. 113:394–404.19. Mahnken AH, Koos R, Katoh M, et al. Assessment of myocardial viability in reperfused acute myocardial infarction using 16-slice computed tomography in comparison to magnetic resonance imaging. J Am Coll Cardiol. 2005. 45:2042–2047.20. Gerber BL, Belge B, Legros GJ, et al. Characterization of acute and chronic myocardial infarcts by multidetector computed tomography: comparison with contrast-enhanced magnetic resonance. Circulation. 2006. 113:823–833.21. Ko SM, Seo JB, Hong MK, et al. Myocardial enhancement pattern in patients with acute myocardial infarction on two-phase contrast-enhanced ECG-gated multidetector-row computed tomography. Clin Radiol. 2006. 61:417–422.22. Heuschmid M, Rothfuss JK, Schroeder S, et al. Assessment of left ventricular myocardial function using 16-slice multidetector-row computed tomography: comparison with magnetic resonance imaging and echocardiography. Eur Radiol. 2006. 16:551–559.23. Raman SV, Shah M, McCarthy B, Garcia A, Ferketich AK. Multi-detector row cardiac computed tomography accurately quantifies right and left ventricular size and function compared with cardiac magnetic resonance. Am Heart J. 2006. 151:736–744.24. Nieman K, Cury RC, Ferencik M, et al. Differentiation of recent and chronic myocardial infarction by cardiac computed tomography. Am J Cardiol. 2006. 98:303–308.25. Achenbach S. Computed tomography coronary angiography. J Am Coll Cardiol. 2006. 48:1919–1928.26. Bertomeu-Gonzalez V, Bouzas-Mosquera A, Kaski JC. Role of trimetazidine in management of ischemic cardiomyopathy. Am J Cardiol. 2006. 98:Suppl. 19J–24J.27. Danchin N. Clinical benefits of a metabolic approach with trimetazidine in revascularized patients with angina. Am J Cardiol. 2006. 98:8J–13J.28. Dib N, Diethrich EB, Campbell A, Gahremanpour A, McGarry M, Opie SR. A percutaneous swine model of myocardial infarction. J Pharmacol Toxicol Methods. 2006. 53:256–263.29. El-Kady T, El-Sabban K, Gabaly M, Sabry A, Abdel-Hady S. Effects of trimetazidine on myocardial perfusion and the contractile response of chronically dysfunctional myocardium in ischemic cardiomyopathy: a 24-month study. Am J Cardiovasc Drugs. 2005. 5:271–278.30. Volpi A, Cavalli A, Santoro L, Negri E. Incidence and prognosis of early primary ventricular fibrillation in acute myocardial infarction: results of the Gruppo Italiano per lo Studio della Sopravvivenza nell' Infarto Miocardico (GISSI-2) database. Am J Cardiol. 1998. 82:265–271.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effects of Trimetazidine on the Enhancement Patterns of Multi-Detector Computed Tomography in a Porcine Myocardial Infarction Model: What is the Meaning of the MDCT Enhancement Pattern in this Myocardial Infarction Model?
- Three cases of right coronary anomaly confirmed by multi-detector computed tomography
- A Case of Spontaneous Coronary Artery Dissection Healed by Medical Treatment: Serial Findings of Coronary Angiography, Intravascular Ultrasound and Multi-Detector Computed Tomography
- Overlooked or unrecognized pitfalls in noninvasive multi-detector computed tomography coronary angiography
- Assessment of Left Ventricular Myocardial Diseases with Cardiac Computed Tomography