J Clin Neurol.
2007 Jun;3(2):71-78. 10.3988/jcn.2007.3.2.71.
Are in-Hospital Delays Important Obstacles in Thrombolytic Therapy Following Acute Ischemic Stroke?
- Affiliations
-
- 1Department of Neurology, Cheju National University School of Medicine, Jeju, Korea. iguazzu@hanmail.net
- 2Department of Preventive Medicine, Cheju National University School of Medicine, Jeju, Korea.
- KMID: 1851015
- DOI: http://doi.org/10.3988/jcn.2007.3.2.71
Abstract
- BACKGROUND AND PURPOSE
The advances in the diagnosis and treatment of acute stroke increase the importance of providing these patients with timely medical attention. This study was designed to assess time delays in neurological evaluation and neuroimaging and to determine whether they are important obstacles to performing thrombolytic therapy.
METHODS
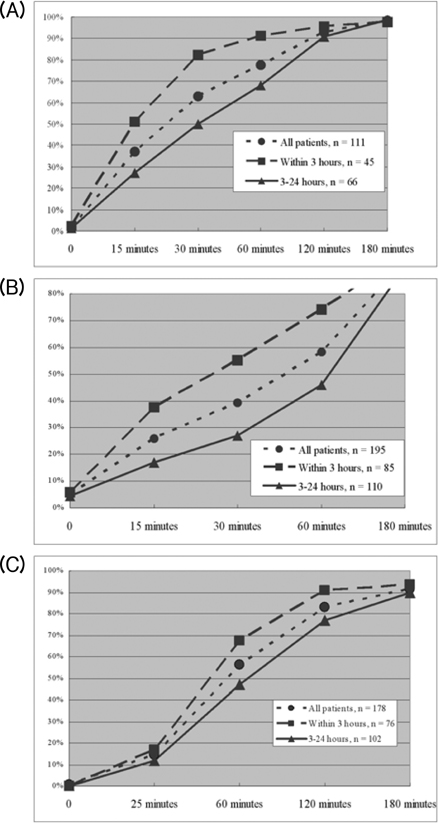
Data were obtained between May 2004 and September 2006 from 195 consecutive patients who were admitted to Cheju National University Hospital for acute ischemic stroke within 24 hours of the onset of symptoms. We determined the time of the onset of symptoms, arrival time at the emergency department (ED), and times of neurology notification, neurology evaluation, and neuroimaging using interviews and by reviewing the medical record.
RESULTS
Short onset-to-door time, performing computed tomography rather than magnetic resonance imaging, presence of aphasia or motor weakness, and severe initial neurological deficit were significantly associated with reduced in-hospital delays. Seventeen (20%) of the 85 patients who arrived within 3 hours of the onset of symptoms received intravenous thrombolysis. Mild neurological deficit, rapidly improving symptoms, and insufficient time to workup were the main causes of the nonreceipt of thrombolytic therapy in these patients. Only one patient did not receive thrombolytic therapy due to delay in neurology consultation.
CONCLUSIONS
Whilst in-hospital delays were not major obstacles to performing thrombolytic therapy in this study, there is still a high probability of missing patients with mild-to-moderate stroke symptoms. More effective in-hospital organization is required for the prompt evaluation and treatment of patients with acute ischemic stroke.
MeSH Terms
Figure
Cited by 2 articles
-
Cost-Effectiveness of Recombinant Tissue Plasminogen Activator in the Management of Acute Ischemic Stroke: A Systematic Review
Kee-Taig Jung, Dong Wook Shin, Kyung-Jin Lee, Myungju Oh
J Clin Neurol. 2010;6(3):117-126. doi: 10.3988/jcn.2010.6.3.117.Emergency Microsurgical Embolectomy for the Treatment of Acute Intracranial Artery Occlusion: Report of Two Cases
Dae-Won Kim, Sung-Jo Jang, Sung-Don Kang
J Clin Neurol. 2011;7(3):159-163. doi: 10.3988/jcn.2011.7.3.159.
Reference
-
1. The National Institute of Neurological Disorders and Stroke rt-PA Stroke study group. Tissue plasminogen activator for acute ischemic stroke. N Engl J Med. 1995. 333:1581–1587.2. Hacke W, Donnan G, Fieschi C, Kaste M, von Kummer R, Broderick JP, et al. Association of outcome with early stroke treatment: pooled analysis of ATLANTIS, ECASS, and NINDS rt-PA stroke trials. Lancet. 2004. 363:768–774.
Article3. Reeves MJ, Arora S, Broderick JP, Frankel M, Heinrich JP, Hickenbottom S, et al. Acute stroke care in the US: results from 4 pilot prototypes of the Paul Coverdell National Acute Stroke Registry. Stroke. 2005. 36:1232–1240.4. Schenkel J, Weimar C, Knoll T, Haberl RL, Busse O, Hamann GF, et al. R1 - systemic thrombolysis in German stroke units - the experience from the German Stroke data bank. J Neurol. 2003. 250:320–324.5. Kleindorfer D, Kissela B, Schneider A, Woo D, Khoury J, Miller R, et al. Eligibility for recombinant tissue plasminogen activator in acute ischemic stroke: a population-based study. Stroke. 2004. 35:e27–e29.6. Barber PA, Zhang J, Demchuk AM, Hill MD, Buchan AM. Why are stroke patients excluded from TPA therapy? An analysis of patient eligibility. Neurology. 2001. 56:1015–1020.
Article7. Cocho D, Belvis R, Marti-Fabregas J, Molina-Porcel L, Diaz-Manera J, Aleu A, et al. Reasons for exclusion from thrombolytic therapy following acute ischemic stroke. Neurology. 2005. 64:719–720.
Article8. Katzan IL, Hammer MD, Hixson ED, Furlan AJ, Abou-Chebl A, Nadzam DM. Utilization of intravenous tissue plasminogen activator for acute ischemic stroke. Arch Neurol. 2004. 61:346–350.
Article9. Huang P, Chen CH, Yang YH, Lin RT, Lin FC, Liu CK. Eligibility for recombinant tissue plasminogen activator in acute ischemic stroke: way to endeavor. Cerebrovasc Dis. 2006. 22:423–428.
Article10. National Institute of Neurological Disorders and Stroke. Proceedings of a national symposium on rapid identification and treatment of acute stroke. 1997. Washington:11. Kothari R, Jauch E, Broderick J, Brott T, Sauerbeck L, Khoury J, et al. Acute stroke: delays to presentation and emergency department evaluation. Ann Emerg Med. 1999. 33:3–8.
Article12. Bratina P, Greenberg L, Pasteur W, Grotta JC. Current emergency department management of stroke in Houston, Texas. Stroke. 1995. 26:409–414.
Article13. Wester P, Radberg J, Lundgren B, Peltonen M; Seek-Medical-Attention-in-Time Study Group. Factors associated with delayed admission to hospital and in-hospital delays in acute stroke and TIA: a prospective, multicenter study. Stroke. 1999. 30:40–48.
Article14. Morris DL, Rosamond WD, Hinn AR, Gorton RA. Time delays in accessing stroke care in the emergency department. Acad Emerg Med. 1999. 6:218–223.
Article15. Morris DL, Rosamond W, Madden K, Schultz C, Hamilton S. Prehospital and emergency department delays after acute stroke: The Genentech Stroke Presentation Survey. Stroke. 2000. 31:2585–2590.
Article16. Adams HP, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993. 24:35–41.
Article17. Jungehulsing GJ, Rossnagel K, Nolte CH, Muller-Nordhorn J, Roll S, Klein M, et al. Emergency department delays in acute stroke - analysis of time between ED arrival and imaging. Eur J Neurol. 2006. 13:225–232.
Article18. Chalela JA, Kidwell CS, Nentwich LM, Luby M, Butman JA, Demchuk AM, et al. Magnetic resonance imaging and computed tomography in emergency assessment of patients with suspected acute stroke: a prospective comparison. Lancet. 2007. 369:293–298.
Article19. Sims J, Schwamm LH. The evolving role of acute stroke imaging in intravenous thrombolytic therapy: patient selection and outcomes assessment. Neuroimaging Clin N Am. 2005. 15:421–440. xii
Article20. Thomalla G, Schwark C, Sobesky J, Bluhmki E, Fiebach JB, Fiehler J, et al. Outcome and symptomatic bleeding complications of intravenous thrombolysis within 6 hours in MRI-selected stroke patients: comparison of a German multicenter study with the pooled data of ATLANTIS, ECASS, and NINDS tPA trials. Stroke. 2006. 37:852–858.
Article21. Kang DW, Chalela JA, Dunn W, Warach S; NIH-Suburban Stroke Center Investigators. MRI screening before standard tissue plasminogen activator therapy is feasible and safe. Stroke. 2005. 36:1939–1943.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pneumococcal meningitis complicated by otomastoiditis and pneumocephalus confounding an acute ischemic stroke diagnosis
- A Case of Hemoperitoneum after Intraarterial Urokinase Infusion for Acute Ischemic Stroke
- Performance Rate of Thrombolytic Therapy and Acute Prognosis of Hyperacute Ischemic Stroke
- Guideline for intra-arterial thrombolysis of hyperacute ischemic stroke patients: Preliminary Report
- Repeated Thrombolytic Therapy in Patients with Recurrent Acute Ischemic Stroke