J Periodontal Implant Sci.
2014 Feb;44(1):2-7. 10.5051/jpis.2014.44.1.2.
How to improve the survival rate of implants after radiotherapy for head and neck cancer?
- Affiliations
-
- 1Department of Stomatology, Zhou Shan Hospital, Zhoushan Zhejiang, China. tangyaling@scu.edu.cn, lxh88866@scu.edu.cn
- 2State Key Laboratory of Oral Diseases, West China Hospital of Stomatology, Sichuan University, Chengdu Sichuan, China.
- 3Department of Oral Pathology, West China Hospital of Stomatology, Sichuan University, Chengdu Sichuan, China.
- 4Department of Oral and Maxillofacial Surgery, West China College of Stomatology, Sichuan University, Chengdu Sichuan, China.
- KMID: 1845871
- DOI: http://doi.org/10.5051/jpis.2014.44.1.2
Abstract
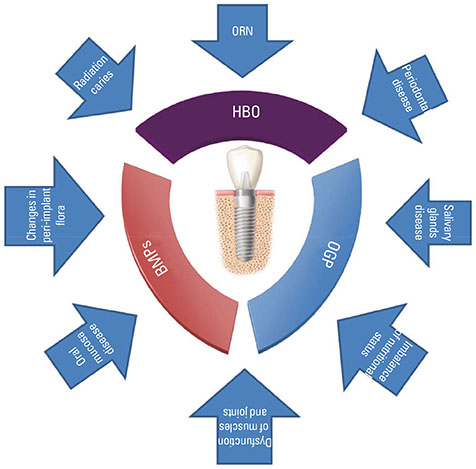
- Implants have been widely used in restorative treatment for patients who have undergone head and neck cancer surgery. With the development of combination treatment of head and neck cancer, radiotherapy has been a common means of therapy. However, it could induce various changes in hard and soft tissues and reduce the success and survival rate of the implants. Some research, using either animal models or clinical studies, have shown that certain strategies could be used for improving the survival rate of implants. In this review, we discussed the changes in both hard and soft tissues, which may reduce the survival rate of the implants, and the proposed methods for improving the survival rate of patients after radiotherapy.
Keyword
MeSH Terms
Figure
Reference
-
1. Harding SA, Hodder SC, Courtney DJ, Bryson PJ. Impact of perioperative hyperbaric oxygen therapy on the quality of life of maxillofacial patients who undergo surgery in irradiated fields. Int J Oral Maxillofac Surg. 2008; 37:617–624.
Article2. Tanaka TI, Chan HL, Tindle DI, Maceachern M, Oh TJ. Updated clinical considerations for dental implant therapy in irradiated head and neck cancer patients. J Prosthodont. 2013; 22:432–438.
Article3. Krause S, Debus J, Neuhof D. Radiotherapy. Recent Results Cancer Res. 2011; 183:285–291.
Article4. Thavarajah N, Wong K, Zhang L, Bedard G, Wong E, Tsao M, et al. Continued success in providing timely palliative radiation therapy at the Rapid Response Radiotherapy Program: a review of 2008-2012. Curr Oncol. 2013; 20:e206–e211.
Article5. Ohri N, Shen X, Dicker AP, Doyle LA, Harrison AS, Showalter TN. Radiotherapy protocol deviations and clinical outcomes: a meta-analysis of cooperative group clinical trials. J Natl Cancer Inst. 2013; 105:387–393.
Article6. Koga DH, Salvajoli JV, Alves FA. Dental extractions and radiotherapy in head and neck oncology: review of the literature. Oral Dis. 2008; 14:40–44.
Article7. O'Dell K, Sinha U. Osteoradionecrosis. Oral Maxillofac Surg Clin North Am. 2011; 23:455–464.8. Nagy K, Urban E, Fazekas O, Thurzo L, Nagy E. Controlled study of lactoperoxidase gel on oral flora and saliva in irradiated patients with oral cancer. J Craniofac Surg. 2007; 18:1157–1164.
Article9. Ihde S, Kopp S, Gundlach K, Konstantinovic VS. Effects of radiation therapy on craniofacial and dental implants: a review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009; 107:56–65.
Article10. Yerit KC, Posch M, Seemann M, Hainich S, Dortbudak O, Turhani D, et al. Implant survival in mandibles of irradiated oral cancer patients. Clin Oral Implants Res. 2006; 17:337–344.
Article11. Keller EE, Tolman DE, Zuck SL, Eckert SE. Mandibular endosseous implants and autogenous bone grafting in irradiated tissue: a 10-year retrospective study. Int J Oral Maxillofac Implants. 1997; 12:800–813.12. Babin RW, Ryu JH, Gantz BJ, Maynard JA. Survival of implanted irradiated cartilage. Otolaryngol Head Neck Surg. 1982; 90:75–80.
Article13. Buddula A, Assad DA, Salinas TJ, Garces YI. Survival of dental implants in native and grafted bone in irradiated head and neck cancer patients: a retrospective analysis. Indian J Dent Res. 2011; 22:644–648.
Article14. Mancha de la Plata M, Gias LN, Diez PM, Munoz-Guerra M, Gonzalez-Garcia R, Lee GY, et al. Osseointegrated implant rehabilitation of irradiated oral cancer patients. J Oral Maxillofac Surg. 2012; 70:1052–1063.
Article15. Linsen SS, Martini M, Stark H. Long-term results of endosteal implants following radical oral cancer surgery with and without adjuvant radiation therapy. Clin Implant Dent Relat Res. 2012; 14:250–258.
Article16. Colley HE, Eves PC, Pinnock A, Thornhill MH, Murdoch C. Tissue-engineered oral mucosa to study radiotherapy-induced oral mucositis. Int J Radiat Biol. 2013; 89:907–914.
Article17. Cheng SC, Wu VW, Kwong DL, Ying MT. Assessment of post-radiotherapy salivary glands. Br J Radiol. 2011; 84:393–402.
Article18. Khojastepour L, Bronoosh P, Zeinalzade M. Mandibular bone changes induced by head and neck radiotherapy. Indian J Dent Res. 2012; 23:774–777.
Article19. Silverman S Jr, Chierici G. Radiation therapy of oral carcinoma. I. Effects on oral tissues and management of the periodontium. J Periodontol. 1965; 36:478–484.
Article20. Mariano FV, Gondak RO, Santos-Silva AR, Correa MB, Almeida OP, Lopes MA. Reactive post-radiotherapy bone formation in the maxilla. J Craniofac Surg. 2013; 24:e43–e45.
Article21. Georgiou KR, Hui SK, Xian CJ. Regulatory pathways associated with bone loss and bone marrow adiposity caused by aging, chemotherapy, glucocorticoid therapy and radiotherapy. Am J Stem Cells. 2012; 1:205–224.22. Lambade PN, Lambade D, Goel M. Osteoradionecrosis of the mandible: a review. Oral Maxillofac Surg. 2013; 17:243–249.
Article23. Wu G, Chen L, Zhu G, Wang Y. Low-intensity ultrasound accelerates mandibular implant bone integration in dogs with mandibular osteoradionecrosis. J Surg Res. 2013; 182:55–61.
Article24. Sugerman PB, Barber MT. Patient selection for endosseous dental implants: oral and systemic considerations. Int J Oral Maxillofac Implants. 2002; 17:191–201.25. Marques MA, Dib LL. Periodontal changes in patients undergoing radiotherapy. J Periodontol. 2004; 75:1178–1187.
Article26. Colella G, Vuolo G, Siniscalchi G, Moscariello A, Itro A. Radiotherapy for maxillo-facial hemangiomas in children: dental and periodontal long term effects. Minerva Stomatol. 2005; 54:509–516.27. Leung WK, Jin LJ, Samaranayake LP, Chiu GK. Subgingival microbiota of shallow periodontal pockets in individuals after head and neck irradiation. Oral Microbiol Immunol. 1998; 13:1–10.
Article28. Vissink A, Jansma J, Spijkervet FK, Burlage FR, Coppes RP. Oral sequelae of head and neck radiotherapy. Crit Rev Oral Biol Med. 2003; 14:199–212.29. Blaha PJ, Reeve CM. Periodontal treatment for patients with cancer. Curr Opin Periodontol. 1994; 64–70.30. Fiorentino A, Caivano R, Metallo V, Chiumento C, Cozzolino M, Califano G, et al. Parotid gland volumetric changes during intensity-modulated radiotherapy in head and neck cancer. Br J Radiol. 2012; 85:1415–1419.
Article31. Chen WC, Lai CH, Lee TF, Hung CH, Liu KC, Tsai MF, et al. Scintigraphic assessment of salivary function after intensity-modulated radiotherapy for head and neck cancer: correlations with parotid dose and quality of life. Oral Oncol. 2013; 49:42–48.
Article32. Şimşek G, Gurocak S, Karadag N, Karabulut AB, Demirtas E, Karatas E, et al. Protective effects of resveratrol on salivary gland damage induced by total body irradiation in rats. Laryngoscope. 2012; 122:2743–2748.
Article33. Santos-Silva AR, Rosa GB, Eduardo CP, Dias RB, Brandao TB. Increased risk for radiation-related caries in cancer patients using topical honey for the prevention of oral mucositis. Int J Oral Maxillofac Surg. 2011; 40:1335–1336.
Article34. Hong CH, Napenas JJ, Hodgson BD, Stokman MA, Mathers-Stauffer V, Elting LS, et al. A systematic review of dental disease in patients undergoing cancer therapy. Support Care Cancer. 2010; 18:1007–1021.
Article35. Sammartino G, Marenzi G, Cioffi I, Tete S, Mortellaro C. Implant therapy in irradiated patients. J Craniofac Surg. 2011; 22:443–445.
Article36. Carney AY. Hyperbaric oxygen therapy: an introduction. Crit Care Nurs Q. 2013; 36:274–279.37. Wang X, Ding I, Xie H, Wu T, Wersto N, Huang K, et al. Hyperbaric oxygen and basic fibroblast growth factor promote growth of irradiated bone. Int J Radiat Oncol Biol Phys. 1998; 40:189–196.
Article38. Anderson L, Meraw S, Al-Hezaimi K, Wang HL. The influence of radiation therapy on dental implantology. Implant Dent. 2013; 22:31–38.
Article39. Granström G, Jacobsson M, Tjellstrom A. Titanium implants in irradiated tissue: benefits from hyperbaric oxygen. Int J Oral Maxillofac Implants. 1992; 7:15–25.40. Chen X, Matsui Y, Ohno K, Michi K. Histomorphometric evaluation of the effect of hyperbaric oxygen treatment on healing around hydroxyapatite implants in irradiated rat bone. Int J Oral Maxillofac Implants. 1999; 14:61–68.41. Marx RE, Ehler WJ, Tayapongsak P, Pierce LW. Relationship of oxygen dose to angiogenesis induction in irradiated tissue. Am J Surg. 1990; 160:519–524.42. Johnsson AA, Sawaii T, Jacobsson M, Granstrom G, Turesson I. A histomorphometric and biomechanical study of the effect of delayed titanium implant placement in irradiated rabbit bone. Clin Implant Dent Relat Res. 2000; 2:42–49.
Article43. Donoff RB. Treatment of the irradiated patient with dental implants: the case against hyperbaric oxygen treatment. J Oral Maxillofac Surg. 2006; 64:819–822.44. Wagner W, Esser E, Ostkamp K. Osseointegration of dental implants in patients with and without radiotherapy. Acta Oncol. 1998; 37:693–696.45. Granström G. Placement of dental implants in irradiated bone: the case for using hyperbaric oxygen. J Oral Maxillofac Surg. 2006; 64:812–818.
Article46. Granström G. Osseointegration in irradiated cancer patients: an analysis with respect to implant failures. J Oral Maxillofac Surg. 2005; 63:579–585.47. McGovern SC, Fong W, Wang JC. Can bone morphogenetic protein binding peptide increase efficiency of bone formation? Spine (Phila Pa 1976). 2010; 35:1655–1659.48. Würzler KK, DeWeese TL, Sebald W, Reddi AH. Radiation-induced impairment of bone healing can be overcome by recombinant human bone morphogenetic protein-2. J Craniofac Surg. 1998; 9:131–137.
Article49. Springer IN, Niehoff P, Acil Y, Marget M, Lange A, Warnke PH, et al. BMP-2 and bFGF in an irradiated bone model. J Craniomaxillofac Surg. 2008; 36:210–217.
Article50. Zhang WB, Zheng LW, Chua DT, Cheung LK. Expression of bone morphogenetic protein, vascular endothelial growth factor, and basic fibroblast growth factor in irradiated mandibles during distraction osteogenesis. J Oral Maxillofac Surg. 2011; 69:2860–2871.
Article51. Iyomasa MM, Issa JP, de Queiroz Tavares ML, Pereira YC, Stuani MB, Mishima F, et al. Influence of low-level laser associated with osteogenic proteins recombinant human BMP-2 and Hevea brasiliensis on bone repair in Wistar rats. Microsc Res Tech. 2012; 75:117–125.
Article52. Ong KL, Villarraga ML, Lau E, Carreon LY, Kurtz SM, Glassman SD. Off-label use of bone morphogenetic proteins in the United States using administrative data. Spine (Phila Pa 1976). 2010; 35:1794–1800.
Article53. Razzouk S, Sarkis R. BMP-2: biological challenges to its clinical use. N Y State Dent J. 2012; 78:37–39.54. Lauzon MA, Bergeron E, Marcos B, Faucheux N. Bone repair: new developments in growth factor delivery systems and their mathematical modeling. J Control Release. 2012; 162:502–520.
Article55. Johnson EE, Urist MR, Schmalzried TP, Chotivichit A, Huang HK, Finerman GA. Autogeneic cancellous bone grafts in extensive segmental ulnar defects in dogs. Effects of xenogeneic bovine bone morphogenetic protein without and with interposition of soft tissues and interruption of blood supply. Clin Orthop Relat Res. 1989; (243):254–265.56. Yan MN, Dai KR, Tang TT, Zhu ZA, Lou JR. Reconstruction of peri-implant bone defects using impacted bone allograft and BMP-2 gene-modified bone marrow stromal cells. J Biomed Mater Res A. 2010; 93:304–313.
Article57. Bab IA. Regulatory role of osteogenic growth peptide in proliferation, osteogenesis, and hemopoiesis. Clin Orthop Relat Res. 1995; (313):64–68.58. Chen Z, Chang M, Peng Y, Zhao L, Zhan Y, Wang L, et al. Regulation of endochondral ossification by osteogenic growth peptide C-terminal pentapeptide [OGP(10-14)]. Protein Pept Lett. 2009; 16:1074–1080.
Article59. Gabarin N, Gavish H, Muhlrad A, Chen YC, Namdar-Attar M, Nissenson RA, et al. Mitogenic G(i) protein-MAP kinase signaling cascade in MC3T3-E1 osteogenic cells: activation by C-terminal pentapeptide of osteogenic growth peptide [OGP(10-14)] and attenuation of activation by cAMP. J Cell Biochem. 2001; 81:594–603.
Article60. Gurevitch O, Slavin S, Muhlrad A, Shteyer A, Gazit D, Chorev M, et al. Osteogenic growth peptide increases blood and bone marrow cellularity and enhances engraftment of bone marrow transplants in mice. Blood. 1996; 88:4719–4724.
Article61. Sun YQ, Ashhurst DE. Osteogenic growth peptide enhances the rate of fracture healing in rabbits. Cell Biol Int. 1998; 22:313–319.
Article62. Gabet Y, Muller R, Regev E, Sela J, Shteyer A, Salisbury K, et al. Osteogenic growth peptide modulates fracture callus structural and mechanical properties. Bone. 2004; 35:65–73.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of survival rates between patients treated with conventional radiotherapy and helical tomotherapy for head and neck cancer
- Radiation Therapy of Head and Neck Cancer with CO-6O HDR Transcatheteric Irradiation
- The value of salvage operation for recurrent head and neck cancer after surgery alone or surgery with radiotherapy
- Radiotherapy of Stage I and II localized Head and Neck Non-odgkin' Ly,phoma
- Treatment Results and Patterns of Failure after Surgery for the Squamous Cell Carcinoma of Hypopharynx