J Korean Soc Spine Surg.
2014 Mar;21(1):24-29. 10.4184/jkss.2014.21.1.24.
The Relationship Between Preoperative MRI Findings and Clinical Outcomes in Surgical Treatment of Lumbar Disc Herniation
- Affiliations
-
- 1Department of Orthopaedic Surgery, Yonsei University College of Medicine, Seoul, Korea. hwanlee@yuhs.ac
- 2Department of Orthopaedic Surgery, Kwangmyeong Sung-Ae Hospital, Kwangmyeong, Korea.
- KMID: 1840413
- DOI: http://doi.org/10.4184/jkss.2014.21.1.24
Abstract
- STUDY DESIGN: A retrospective study.
OBJECTIVES
To assess the relationship between surgical outcomes and preoperative MRI findings, a retrospective review was conducted on the surgical outcomes depending on the preoperative MRI findings including type of herniation and Modic changes. SUMMARY OF LITERATURE REVIEW: In most reports, the patients that have large disc herniation were expected to have improved surgical outcomes. However, there have been controversies regarding the outcomes and Modic changes.
MATERIALS AND METHODS
The retrospective review was conducted in 82 patients who underwent a discectomy for single level lumbar disc herniation. The average follow-up period was 34.2 months. Among their preoperative baseline MRI measurements, the stage of disc herniation, degree of nerve root compression, degree of dural sac compression, and Modic change of vertebral endplate were evaluated for the subsequent comparison between the preoperative and postoperative changes and ODI score.
RESULTS
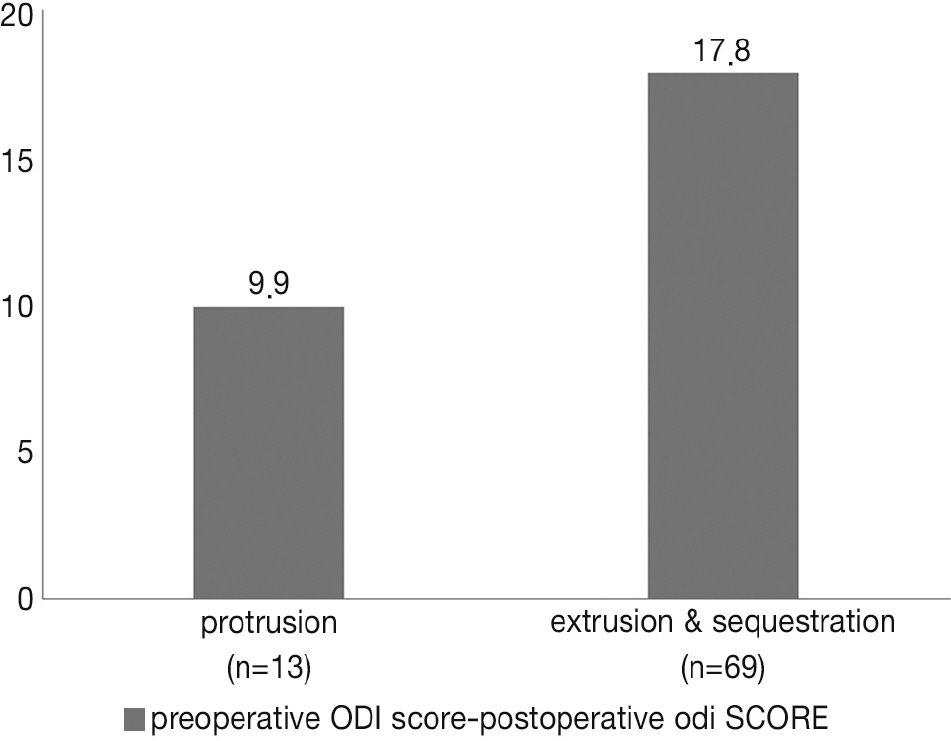
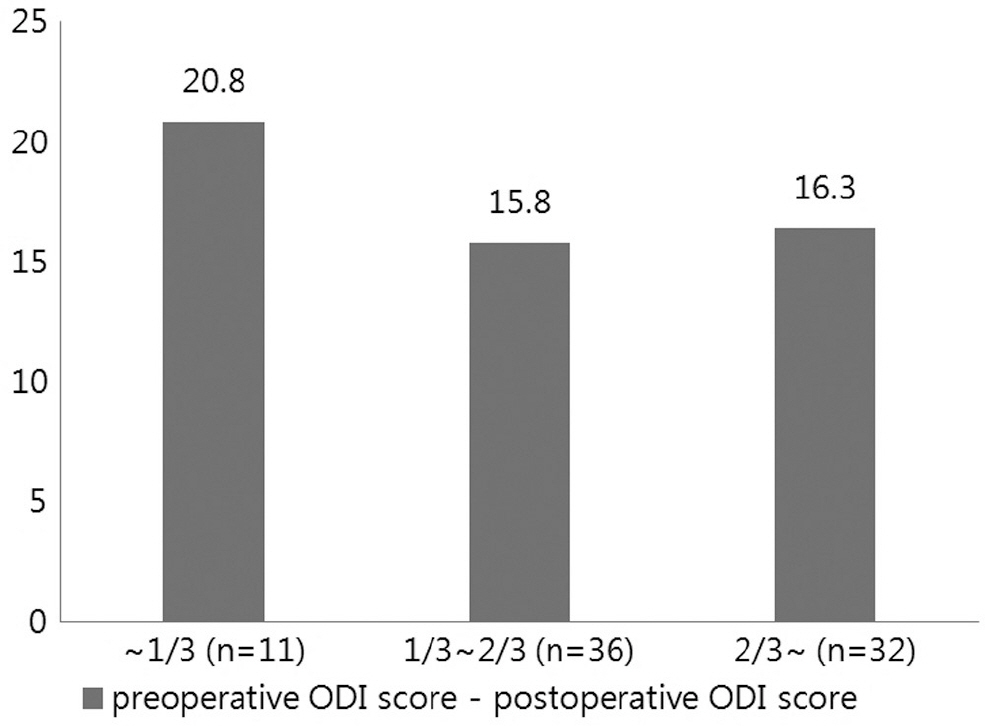
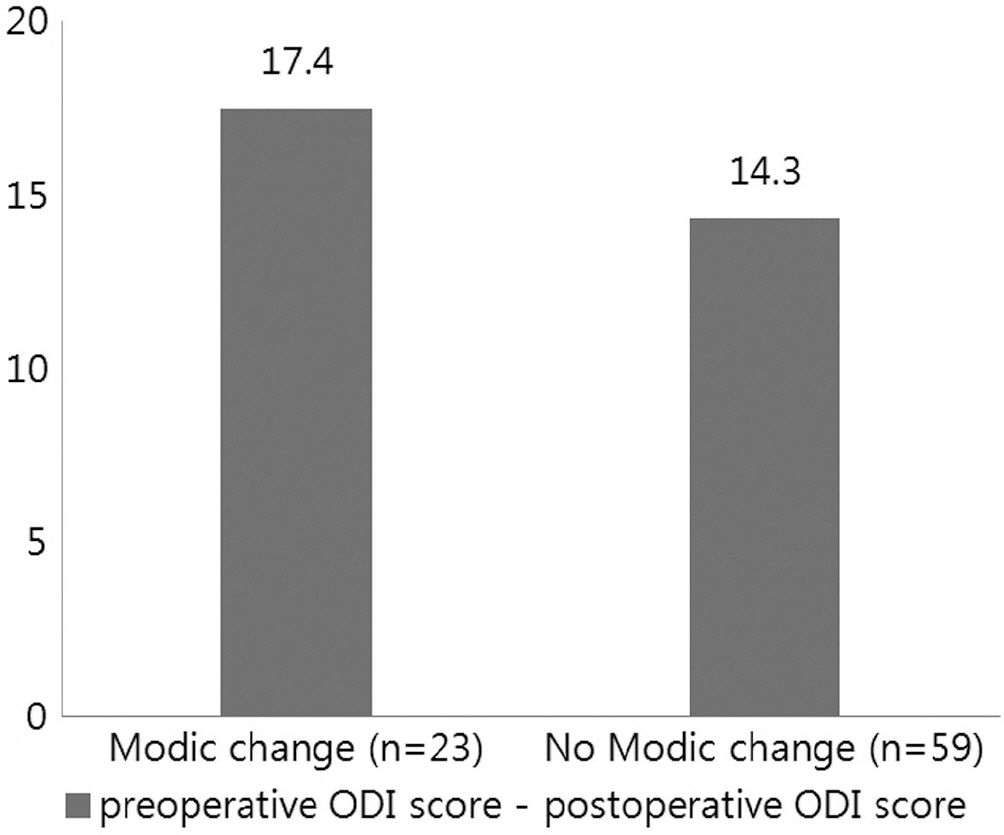
Patients with extrusion or sequestration type showed significant improvements compared to the patients with protrusion type disc herniation. By degree of nerve root compression, patients with root compression showed significant improvements compared to the patients who had contact type. The degree of dural sac compression revealed no correlation with changes in the ODI score. 23 of the 82 patients, the preoperative MRI showed a Modic change. Compared to the group who did not show such a Modic change, they turned out to be unrelated to the preoperative and postoperative changes in the ODI score.
CONCLUSIONS
Patients who had extrusion or sequestration type disc herniation showed a better clinical improvement than protrusion type. Patients with compression type root lesion showed better clinical improvement than contact type root lesion. No correlation was noted regarding the outcomes of the surgical treatment and degree of dural sac compression or Modic changes.
Keyword
MeSH Terms
Figure
Reference
-
1. Spangfort EV. The lumbar disc herniation. A computer-aided analysis of 2,504 operations. Acta Orthop Scand Suppl. 1972; 142:1–95.
Article2. Carlisle E, Luna M, Tsou PM, Wang JC. Percent spinal canal compromise on MRI utilized for predicting the need for surgical treatment in single-level lumbar intervertebral disc herniation. Spine J. 2005; 5:608–14.
Article3. Carragee EJ, Han MY, Suen PW, Kim D. Clinical outcomes after lumbar discectomy for sciatica: the effects of fragment type and anular competence. J Bone Joint Surg Am. 2003; 85:102–8.4. Jensen RK, Leboeuf-Yde C, Wedderkopp N, Sorensen JS, Jensen TS, Manniche C. Is the development of Modic changes associated with clinical symptoms? A 14-month cohort study with MRI. Eur Spine J. 2012; 21:2271–9.
Article5. Sorlie A, Moholdt V, Kvistad KA, et al. Modic type I changes and recovery of back pain after lumbar microdiscectomy. Eur Spine J. 2012; 21:2252–8.
Article6. Eismont FJ, Currier B. Surgical management of lumbar intervertebral-disc disease. J Bone Joint Surg Am. 1989; 71:1266–71.
Article7. Fardon DF, Milette PC. Combined Task Forces of the North American Spine Society ASoSR, American Society of N. Nomenclature and classification of lumbar disc pathology. Recommendations of the Combined task Forces of the North American Spine Society, American Society of Spine Radiology, and American Society of Neuroradiology. Spine (Phila Pa 1976). 2001; 26:E93–E113.8. Pfirrmann CW, Dora C, Schmid MR, Zanetti M, Hodler J, Boos N. MR image-based grading of lumbar nerve root compromise due to disk herniation: reliability study with surgical correlation. Radiology. 2004; 230:583–8.
Article9. Modic MT, Steinberg PM, Ross JS, Masaryk TJ, Carter JR. Degenerative disk disease: assessment of changes in vertebral body marrow with MR imaging. Radiology. 1988; 166:193–9.
Article10. Jeon CH, Kim DJ, Kim SK, Kim DJ, Lee HM, Park HJ. Validation in the cross-cultural adaptation of the Korean version of the Oswestry Disability Index. J Kor Med Sci. 2006; 21:1092–7.
Article11. Fairbank JC, Couper J, Davies JB, O'Brien JP. The Oswestry low back pain disability questionnaire. Physiotherapy. 1980; 66:271–3.12. Lee HM, Park MS. Classification and Imaging Study of the Lumbar Disc Herniation. J Korean Soc Spine Surg. 2001; 8:314–20.
Article13. Bush K, Cowan N, Katz DE, Gishen P. The natural history of sciatica associated with disc pathology: a prospective study with clinical and independent radiologic followup. Spine (Phila Pa 1976). 1992; 17:1205–12.
Article14. Hagen KB, Hilde G, Jamtvedt G, Winnem MF. The Co-chrane review of bed rest for acute low back pain and sciatica. Spine (Phila Pa 1976). 2000; 25:2932–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Spinal Nerve Root Swelling Mimicking Intervertebral Disc Herniation in Magnetic Resonance Imaging: A Case Report
- Clinical Analysis of Recurrent Lumbar Disc Herniation
- Analysis of MRI Findings of Adolescent Lumbar Disc Herniation (Comparision with Adult Lumbar Disc Herniation Findings)
- A Clinical Observation on High Lumbar Disc Herniation
- The Relationship between Lumbar Shape and Lumbar Disc Herniation