Trends in Oral Anticoagulation Therapy Among Korean Patients With Atrial Fibrillation: The KORean Atrial Fibrillation Investigation
- Affiliations
-
- 1Department of Cardiology, Keimyung University Dongsan Medical Center, Daegu, Korea. ynkim@dsmc.or.kr
- 2Department of Cardiology, Daegu Catholic University Medical Center, Daegu, Korea.
- KMID: 1826383
- DOI: http://doi.org/10.4070/kcj.2012.42.2.113
Abstract
- BACKGROUND AND OBJECTIVES
Anticoagulation with vitamin K antagonists (VKAs) such as warfarin provides effective stroke prophylaxis in patients with atrial fibrillation (AF). We conducted a large multicenter survey of Korean patients with AF to determine trends in VKA use.
SUBJECTS AND METHODS
Eligible patients were adults with AF that had been prescribed VKAs. Medical records from a total of 5616 patients {mean age 63.6+/-12.2 years, male 3150 (56.1%)} in 27 hospitals from Jan. 2001 to Oct. 2007 were reviewed.
RESULTS
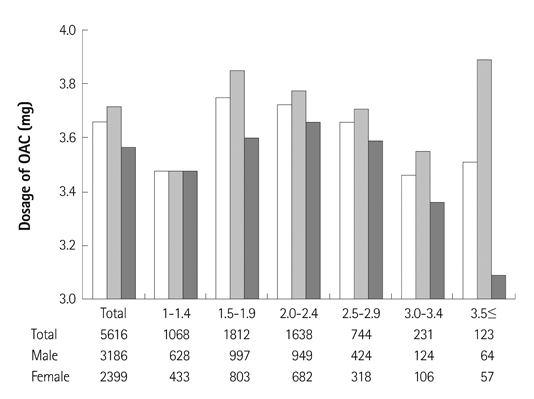
The mean international normalized ratio (INR) was 2.04+/-0.64, and mean dosage of VKA was 3.66+/-1.50 mg. Individuals in their sixties (1852 patients) accounted for about one third of patients studied. As patients grew older, INR increased and VKA dosage decreased. The dosage of VKA in male patients was larger than that in females for all ages. A total of 2146 (42.4%) patients had an INR of 2-3, and less than 40% patients in their sixties had an INR within optimal range. The dosage of oral anticoagulant for optimal INR level was 3.71 mg.
CONCLUSION
In this study, less than half of the Korean patients with AF on VKA reached the therapeutic range of INR. Mean dosage of VKA was 3.66+/-1.50 mg, and the dosage of oral anticoagulant for optimal INR level was 3.71 mg, which decreased with age.
MeSH Terms
Figure
Cited by 2 articles
-
Quality of Anticoagulation and Treatment Satisfaction in Patients with Non-Valvular Atrial Fibrillation Treated with Vitamin K Antagonist: Result from the KORean Atrial Fibrillation Investigation II
Seil Oh, June-Soo Kim, Yong-Seog Oh, Dong-Gu Shin, Hui-Nam Pak, Gyo-Seung Hwang, Kee-Joon Choi, Jin-Bae Kim, Man-Young Lee, Hyung-Wook Park, Dae-Kyeong Kim, Eun-Sun Jin, Jaeseok Park, Il-Young Oh, Dae-Hee Shin, Hyoung-Seob Park, Jun Hyung Kim, Nam-Ho Kim, Min-Soo Ahn, Bo-Jeong Seo, Young-Joo Kim, Seongsik Kang, Juneyoung Lee, Young-Hoon Kim
J Korean Med Sci. 2018;33(49):. doi: 10.3346/jkms.2018.33.e323.Quality of Anticoagulation with Warfarin in Korean Patients with Atrial Fibrillation and Prior Stroke: A Multicenter Retrospective Observational Study
Keun-Sik Hong, Yang-Ki Kim, Hee-Joon Bae, Hyo Suk Nam, Sun U. Kwon, Oh Young Bang, Jae-Kwan Cha, Byung-Woo Yoon, Joung-Ho Rha, Byung-Chul Lee, Jong-Moo Park, Man-Seok Park, Jun Lee, Jay Chol Choi, Dong Eog Kim, Kyung Bok Lee, Tai Hwan Park, Ji Sung Lee, Seong-Eun Kim, Juneyoung Lee
J Clin Neurol. 2017;13(3):273-280. doi: 10.3988/jcn.2017.13.3.273.
Reference
-
1. Singer DE, Albers GW, Dalen JE, et al. Antithrombotic therapy in atrial fibrillation: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest. 2008. 133:6 Suppl. 546S–592S.2. Fuster V, Rydén LE, Cannom DS, et al. 2011 ACCF/AHA/HRS focused updates incorporated into the ACC/AHA/ESC 2006 Guidelines for the management of patients with atrial fibrillation: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines developed in partnership with the European Society of Cardiology and in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society. J Am Coll Cardiol. 2011. 57:e101–e198.3. Lip GY, Agnelli G, Thach AA, Knight E, Rost D, Tangelder MJ. Oral anticoagulation in atrial fibrillation: a pan-European patient survey. Eur J Intern Med. 2007. 18:202–208.4. Ansell J, Hirsh J, Poller L, Bussey H, Jacobson A, Hylek E. The pharmacology and management of the vitamin K antagonists: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004. 126:3 Suppl. 204S–233S.5. Lee KS, Choi SJ, Park SH, Kim HL, Min H, Park HY. Prevalence of atrial fibrillation in middle-aged people in Korea: the Korean Genome and Epidemiology Study. Korean Circ J. 2008. 38:601–605.6. Shen AY, Chen W, Yao JF, Brar SS, Wang X, Go AS. Effect of race/ethnicity on the efficacy of warfarin: potential implications for prevention of stroke in patients with atrial fibrillation. CNS Drugs. 2008. 22:815–825.7. Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation: a major contributor to stroke in the elderly: the Framingham Study. Arch Intern Med. 1987. 147:1561–1564.8. Laupacis A, Boysen G, Connolly S, et al. Risk factors for stroke and efficacy of antithrombotic therapy in atrial fibrillation: analysis of pooled data from five randomized controlled trials. Arch Intern Med. 1994. 154:1449–1457.9. Kim YH. Rhythm control versus rate control of atrial fibrillation: pharmacologic and non-pharmacologic therapy. Korean Circ J. 2003. 33:553–558.10. van Walraven C, Hart RG, Singer DE, et al. Oral anticoagulants vs aspirin in nonvalvular atrial fibrillation: an individual patient meta-analysis. JAMA. 2002. 288:2441–2448.11. Hylek EM, Go AS, Chang Y, et al. Effect of intensity of oral anticoagulation on stroke severity and mortality in atrial fibrillation. N Engl J Med. 2003. 349:1019–1026.12. Waldo AL, Becker RC, Tapson VF, Colgan KJ. NABOR Steering Committee. Hospitalized patients with atrial fibrillation and a high risk of stroke are not being provided with adequate anticoagulation. J Am Coll Cardiol. 2005. 46:1729–1736.13. Stansbury JP, Jia H, Williams LS, Vogel WB, Duncan PW. Ethnic disparities in stroke: epidemiology, acute care, and postacute outcomes. Stroke. 2005. 36:374–386.14. van Walraven C, Jennings A, Oake N, Fergusson D, Forster AJ. Effect of study setting on anticoagulation control: a systematic review and me-taregression. Chest. 2006. 129:1155–1166.15. Yasaka M, Minematsu K, Yamaquchi T. Optimal intensity of international normalized ratio in warfarin therapy for secondary prevention of stroke in patients with non-valvular atrial fibrillation. Intern Med. 2001. 40:1183–1188.16. Miura T, Nishinaka T, Terada T, Yonezawa K. Relationship between aging and dosage of warfarin: the current status of warfarin anticoagulant therapy for Japanese outpatients in a department of cardiovascular medicine. J Cardiol. 2009. 53:355–360.17. Atarashi H, Inoue H, Okumura K, Yamashita T, Kumagai N, Origasa H. J-RHYTHM Registry Investigators. Present status of anticoagulation treatment in Japanese patients with atrial fibrillation: a report from the J-RHYTHM Resistry. Circ J. 2011. 75:1328–1333.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Mechanism of and Preventive Therapy for Stroke in Patients with Atrial Fibrillation
- Stroke Prevention in Atrial Fibrillation
- How and When to Screen for Atrial Fibrillation after Stroke: Insights from Insertable Cardiac Monitoring Devices
- Cardioembolic Stroke in Atrial Fibrillation-Rationale for Preventive Closure of the Left Atrial Appendage
- Pathophysiology and Diagnosis in Atrial Fibrillation