Korean Circ J.
2012 Feb;42(2):95-99. 10.4070/kcj.2012.42.2.95.
Impact of Multivessel Coronary Disease With Chronic Total Occlusion on One-Year Mortality in Patients With Acute Myocardial Infarction
- Affiliations
-
- 1Department of Internal Medicine, Kyungpook National University School of Medicine, Daegu, Korea. hspark@knu.ac.kr
- 2Department of Internal Medicine, Gumi CHA Hospital, Gumi, Korea.
- KMID: 1826380
- DOI: http://doi.org/10.4070/kcj.2012.42.2.95
Abstract
- BACKGROUND AND OBJECTIVES
The impact of multivessel coronary disease (MVD) with chronic total occlusion (CTO) on one-year mortality in patients with acute myocardial infarction (AMI) is not clearly known. We investigated the impact of MVD with concurrent CTO lesion on one-year mortality in patients with AMI.
SUBJECTS AND METHODS
We studied 1008 consecutive patients who underwent coronary angiography between November 2005 and December 2008 with a diagnosis of AMI.
RESULTS
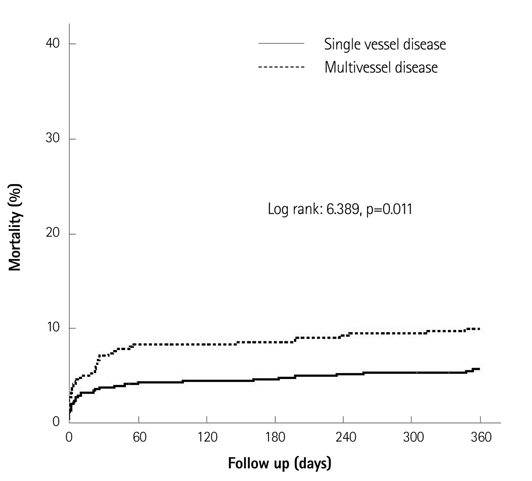
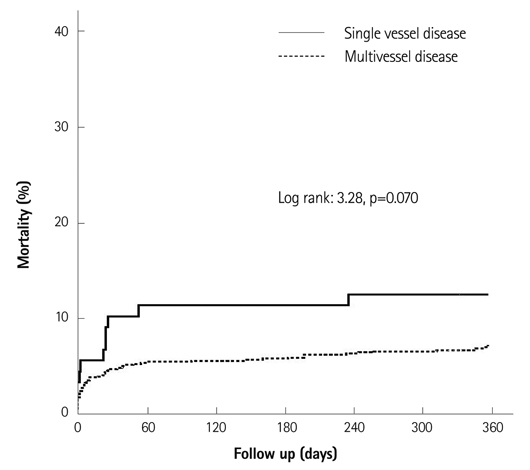
Among 1008 patients, 432 patients (43%) had MVD, and 88 patients (8.7%) had CTO lesion. The one-year overall mortality was higher in patients with MVD than in patients with single vessel disease (SVD) (10.2% vs. 5.9%, p=0.012). However, the one-year overall mortality was not significantly higher in patients with CTO lesion than in patients without that lesion (12.5% vs. 7.3%, p=0.080). In multivariate analysis, independent predictors of one-year overall mortality were age older than 65 years {hazard ratio (HR) 2.41, 95% confidence interval (CI): 1.43 to 4.08}, Killip class > or =III (HR 3.59, 95% CI: 2.24 to 5.77), ST-elevation myocardial infarction (HR 2.45, 95% CI: 1.49 to 4.05) and MVD (HR 1.76, 95% CI: 1.07 to 2.89).
CONCLUSION
Patients with MVD showed higher one-year mortality than patients with SVD. However, the presence of CTO was not an independent predictor of one-year mortality in this study that included patients with successfully revascularized CTO lesion.
MeSH Terms
Figure
Reference
-
1. O'Keefe JH Jr, Rutherford BD, McConahay DR, et al. Early and late results of coronary angioplasty without antecedent thrombolytic therapy for acute myocardial infarction. Am J Cardiol. 1989. 64:1221–1230.2. Moreno R, García E, Soriano J, et al. Early coronary angioplasty for acute myocardial infarction: predictors of poor outcome in a non-selected population. J Invasive Cardiol. 2001. 13:202–210.3. van der Schaaf RJ, Timmer YR, Ottervanger JP, et al. Long-term impact of multivessel disease on cause-specific mortality after ST elevation myocardial infarction treated with reperfusion therapy. Heart. 2006. 92:1760–1763.4. De Boer MJ, Suryapranata H, Hoorntje JC, et al. Limitation of infarct size and preservation of left ventricular function after primary coronary angioplasty compared with intravenous streptokinase in acute myocardial infarction. Circulation. 1994. 90:753–761.5. Shihara M, Tsutsui H, Tsuchihashi M, Tada H, Kono S, Takeshita A. Japanese Coronary Invention Study (JCIS) Group. In-hospital and oneyear outcomes for patients undergoing percutaneous coronary intervention for acute myocardial infarction. Am J Cardiol. 2002. 90:932–936.6. Parodi G, Memisha G, Valenti R, et al. Five year outcome after primary coronary intervention for acute ST elevation myocardial infarction: results from a single centre experience. Heart. 2005. 91:1541–1544.7. Waldecker B, Wass W, Haberbosch W, Voss R, Heizmann H, Tillmanns H. Long-term follow-up after direct percutaneous transluminal coronary angioplasty for acute myocardial infarction. J Am Coll Cardiol. 1998. 32:1320–1325.8. Christofferson RD, Lehmann KG, Martin GV, Every N, Caldwell JH, Kapadia SR. Effects of chronic total coronary occlusion on treatment strategy. Am J Cardiol. 2005. 95:1088–1091.9. van der Schaaf RJ, Vis MM, Sjauw KD, et al. Impact of multivessel coronary disease on long-term mortality in patients with ST-elevation myocardial infarction is due to the presence of a chronic total occlusion. Am J Cardiol. 2006. 98:1165–1169.10. Claessen BE, Hoebers LP, van der Schaaf RJ, et al. Prevalence and impact of a chronic total occlusion in a non-infarct-related artery on longterm mortality in diabetic patients with ST elevation myocardial infarction. Heart. 2010. 96:1968–1972.11. French JK, White HD. Clinical implications of the new definition of myocardial infarction. Heart. 2004. 90:99–106.12. Claessen BE, van der Schaaf RJ, Verouden NJ, et al. Evaluation of the effect of a concurrent chronic total occlusion on long-term mortality and left ventricular function in patients after primary percutaneous coronary intervention. JACC Cardiovasc Interv. 2009. 2:1128–1134.13. Schömig A, Mehilli J, Antoniucci D, et al. Mechanical reperfusion in patients with acute myocardial infarction presenting more than 12 hours from symptom onset: a randomized controlled trial. JAMA. 2005. 293:2865–2872.14. Piscione F, Galasso G, De Luca G, et al. Late reopening of an occluded infarct related artery improves left ventricular function and long term clinical outcome. Heart. 2005. 91:646–651.15. Suero JA, Marso SP, Jones PG, et al. Procedural outcomes and longterm survival among patients undergoing percutaneous coronary intervention of a chronic total occlusion in native coronary arteries: a 20-year experience. J Am Coll Cardiol. 2001. 38:409–414.16. Hoye A, van Domburg RT, Sonnenschein K, Serruys PW. Percutaneous coronary intervention for chronic total occlusions: the Thoraxcenter experience 1992-2002. Eur Heart J. 2005. 26:2630–2636.17. Joyal D, Afilalo J, Rinfret S. Effectiveness of recanalization of chronic total occlusions: a systematic review and meta-analysis. Am Heart J. 2010. 160:179–187.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Two Cases of Multivessel Coronary Artery Ectasias Resulting in Acute Inferior Myocardial Infarction
- Two Cases of Complications during Percutaneous Coronary Intervention for Myocardial Infarction in Patients with Concurrent Chronic Total Occlusion in an Emergency Setting
- The Concurrent Chronic Total Occlusion in a Non-Infarct Artery Strongly Associate With Poor Long-Term Prognosis in Patients With Acute Myocardial Infarction and Multivessel Coronary Disease
- Acute Myocardial Infarction with Simultaneous Thrombosis of Multiple Coronary Arteries
- Acute Myocardial Infarction Occurred in Multivessel Disease Including Chronic Total Occlusion