Korean Circ J.
2010 Nov;40(11):543-549. 10.4070/kcj.2010.40.11.543.
Current Concepts in Cardiac CT Angiography for Patients With Acute Chest Pain
- Affiliations
-
- 1Department of Diagnostic Radiology, CHA Medical University Hospital, Seongnam, Korea.
- 2Department of Diagnostic Radiology, Chung-Ang University College of Medicine, Seoul, Korea.
- 3Department of Cardiology, CHA Medical University Hospital, Seongnam, Korea.
- 4Department of Diagnostic Radiology, University of Maryland, Baltimore, Maryland, USA. cwhite@umm.edu
- KMID: 1826171
- DOI: http://doi.org/10.4070/kcj.2010.40.11.543
Abstract
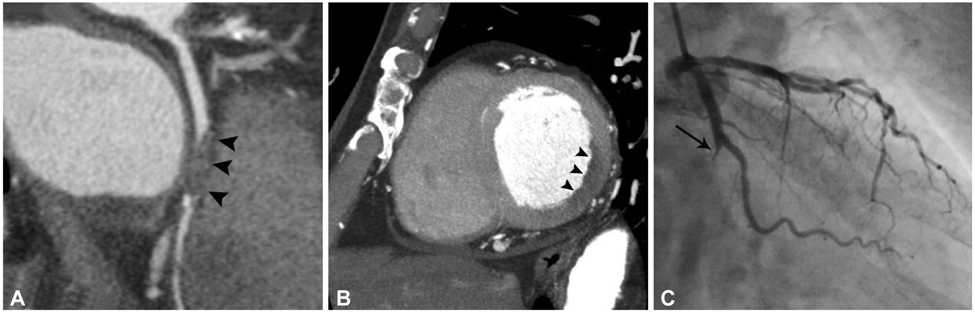
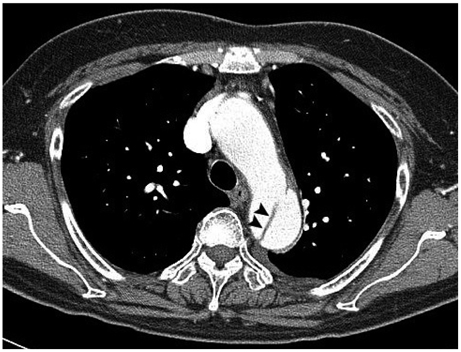
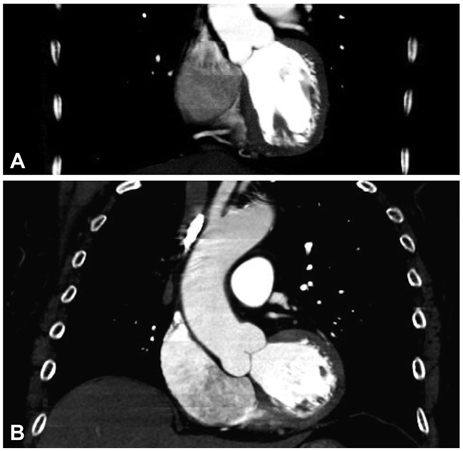
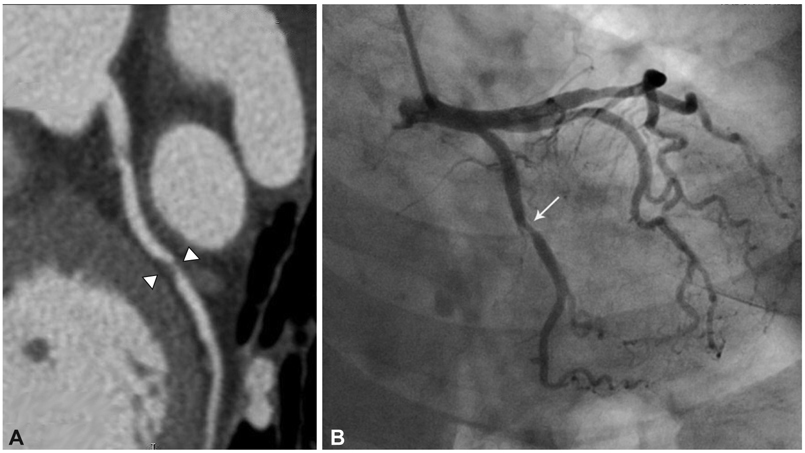
- This article presents specific examples of delayed diagnosis of acute coronary syndrome, acute aortic dissection, and pulmonary embolism resulting from evaluating patients with nonspecific acute chest pain who did not undergo immediate dedicated coronary CT angiography (CTA) or triple rule-out protocol (TRO). These concrete examples of delayed diagnosis may advance the concept of using cardiac CTA (i.e., dedicated coronary CTA versus TRO) to triage patients with nonspecific acute chest pain. This article also provides an overall understanding of how to choose the most appropriate examination based on the specific clinical situation in the emergency department (i.e., dedicated coronary CTA versus TRO versus dedicated pulmonary or aortic CTA), how to interpret the CTA results, and the pros and cons of biphasic versus triphasic administration of intravenous contrast material during TRO examination. A precise understanding of various cardiac CTA protocols will improve the diagnostic performance of radiologists while minimizing hazards related to radiation exposure and contrast use.
Keyword
MeSH Terms
Figure
Reference
-
1. Bastarrika G, Thilo C, Headden GF, Zwerner PL, Costello P, Schoepf UJ. Cardiac CT in the assessment of acute chest pain in the emergency department. AJR Am J Roentgenol. 2009. 193:397–409.2. Lee HY, Yoo SM, White CS. Coronary CT angiography in emergency department patients with acute chest pain: triple rule-out protocol versus dedicated coronary CT angiography. Int J Cardiovasc Imaging. 2009. 25:319–326.3. Halpern EJ. Triple rule-out CT angiography for evaluation of acute chest pain and possible acute coronary syndrome. Radiology. 2009. 252:332–345.4. Johnson TR, Nikolaou K, Wintersperger BJ, et al. Optimization of contrast material administration for electrocardiogram-gated computed tomographic angiography of the chest. J Comput Assist Tomogr. 2007. 31:265–271.5. Frauenfelder T, Appenzeller P, Karlo C, et al. Triple rule-out CT in the emergency department: protocols and spectrum of imaging findings. Eur Radiol. 2009. 19:789–799.6. Litmanovich D, Zamboni GA, Hauser TH, Lin PJ, Clouse ME, Raptopoulos V. ECG-gated chest CT angiography with 64-MDCT and triphasic IV contrast administration regimen in patients with acute nonspecific chest pain. Eur Radiol. 2008. 18:308–317.7. Shuman WP, Branch KR, May JM, et al. Whole-chest 64-MDCT of emergency department patients with nonspecific chest pain: radiation dose and coronary artery image quality with prospective ECG triggering versus retrospective ECG gating. AJR Am J Roentgenol. 2009. 192:1662–1667.8. Johnson TR, Nikolaou K, Becker A, et al. Dual-source CT for chest pain assessment. Eur Radiol. 2008. 18:773–780.9. Schertler T, Scheffel H, Frauenfelder T, et al. Dual-source computed tomography in patients with acute chest pain: feasibility and image quality. Eur Radiol. 2007. 17:3179–3188.10. Takakuwa KM, Halpern EJ. Evaluation of a "triple rule-out" coronary CT angiography protocol: use of 64-Section CT in low-to-moderate risk emergency department patients suspected of having acute coronary syndrome. Radiology. 2008. 248:438–446.11. Pozen MW, D'Agostino RB, Selker HP, Sytkowski PA, Hood WB Jr. A predictive instrument to improve coronary-care-unit admission practices in acute ischemic heart disease. A prospective multicenter clinical trial. N Engl J Med. 1984. 310:1273–1278.12. Hagan PG, Nienaber CA, Isselbacher EM, et al. The International Rregistry of Acute Aortic Dissection (IRAD): new insights into an old disease. JAMA. 2000. 283:897–903.13. Abcarian PW, Sweet JD, Watabe JT, Yoon HC. Role of a quantitative D-dimer assay in determining the need for CT angiography of acute pulmonary embolism. AJR Am J Roentgenol. 2004. 182:1377–1381.14. Klompas M. Does this patient have an acute thoracic aortic dissection? JAMA. 2002. 287:2262–2272.15. Viljanen T. Diagnostic difficulties in aortic dissection. Retrospective study of 89 surgically treated patients. Ann Chir Gynaecol. 1986. 75:328–332.16. Rogg JG, Neve JW, Huang C, et al. The triple work-up for emergency department patients with acute chest pain: how often does it occur? J Emerg Med. 2008. [Epub ahead of print].17. van Belle A, Büller HR, Huisman MV, et al. Effectiveness of managing suspected pulmonary embolism using an algorithm combining clinical probability, D-dimer testing, and computed tomography. JAMA. 2006. 295:172–179.18. von Kodolitsch Y, Schwartz AG, Nienaber CA. Clinical prediction of acute aortic dissection. Arch Intern Med. 2000. 160:2977–2982.19. Gallagher MJ, Raff GL. Use of multislice CT for the evaluation of emergency room patients with chest pain: the so-called "triple rule-out". Catheter Cardiovasc Interv. 2008. 71:92–99.20. Pannu HK, Alvarez W Jr, Fishman EK. Beta-blockers for cardiac CT: a primer for the radiologist. AJR Am J Roentgenol. 2006. 186:6 Suppl 2. S341–S345.21. Hoffmann U, Bamberg F, Chae CU, et al. Coronary computed tomography angiography for early triage of patients with acute chest pain: the ROMICAT (Rule Out Myocardial Infarction using Computer Assisted Tomography) trial. J Am Coll Cardiol. 2009. 53:1642–1650.22. Hamon M, Biondi-Zoccai GC, Malagutti P, et al. Diagnostic performance of multislice spiral computed tomography of coronary arteries as compared with conventional invasive coronary angiography: a meta-analysis. J Am Coll Cardiol. 2006. 48:1896–1910.23. Dokainish H, Pillai M, Murphy SA, et al. Prognostic implications of elevated troponin in patients with suspected acute coronary syndrome but no critical epicardial coronary disease: a TACTICS-TIMI-18 substudy. J Am Coll Cardiol. 2005. 45:19–24.24. Patel MR, Chen AY, Peterson ED, et al. Prevalence, predictors, and outcomes of patients with non-ST-segment elevation myocardial infarction and insignificant coronary disease: results from the can rapid risk stratification of unstable angina patients suppress adverse outcomes with early implementation of the ACC/AHA guidelines (CRUSADE) initiative. Am Heart J. 2006. 152:641–647.25. Goldstein JA, Gallagher MJ, O'Neill WW, Ross MA, O'Neil BJ, Raff GL. A randomized controlled trial of multi-slice coronary computed tomography for evaluation of acute chest pain. J Am Coll Cardiol. 2007. 49:863–871.26. Fleischmann D, Lin M. Remy-Jardin M, Remy J, editors. Contrast medium utilization. Integrated Cardiothoracic Imaging with MDCT. 2008. Berlin, Germany: Springer;53–63.27. Jakobs TF, Becker CR, Ohnesorge B, et al. Multislice helical CT of the heart with retrospective ECG gating: reduction of radiation exposure by ECG-controlled tube current modulation. Eur Radiol. 2002. 12:1081–1086.28. Poll LW, Cohnen M, Brachten S, Ewen K, Mödder U. Dose reduction in multi-slice CT of the heart by use of ECG-controlled tube current modulation ("ECG pulsing"): phantom measurements. Rofo. 2002. 174:1500–1505.29. Husmann L, Valenta I, Gaemperli O, et al. Feasibility of low-dose coronary CT angiography: first experience with prospective ECG-gating. Eur Heart J. 2008. 29:191–197.30. Stolzmann P, Scheffel H, Schertler T, et al. Radiation dose estimates in dual-source computed tomography coronary angiography. Eur Radiol. 2008. 18:592–599.31. Scheffel H, Alkadhi H, Leschka S, et al. Low-dose CT coronary angiography in the step-and-shoot mode: diagnostic performance. Heart. 2008. 94:1132–1137.32. Hirai N, Horiguchi J, Fujioka C, et al. Prospective versus retrospective ECG-gated 64-detector coronary CT angiography: assessment of image quality, stenosis, and radiation dose. Radiology. 2008. 248:424–430.33. Ketelsen D, Luetkhoff MH, Thomas C, et al. Estimation of the radiation exposure of a chest pain protocol with ECG-gating in dual-source computed tomography. Eur Radiol. 2009. 19:37–41.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Current Concepts of Vulnerable Plaque on Coronary CT Angiography
- Normal coronary CT angiography with subsequent adverse cardiac events
- Post-Infarct Cardiac Free Wall Rupture Detected by Multi-Detector Computed Tomography
- Debates over NICE Guideline Update: What Are the Roles of Nuclear Cardiology in the Initial Evaluation of Stable Chest Pain?
- Evolution of Cardiac CT Imaging and Education in Singapore