J Periodontal Implant Sci.
2015 Jun;45(3):82-93. 10.5051/jpis.2015.45.3.82.
Early radiographic diagnosis of peri-implantitis enhances the outcome of peri-implantitis treatment: a 5-year retrospective study after non-surgical treatment
- Affiliations
-
- 1Department of Periodontology, School of Dentistry, Wonkwang University, Iksan, Korea.
- 2Department of Periodontology, Section of Dentistry, Seoul National University Bundang Hospital, Seongnam, Korea. periolee@gmail.com
- 3Department of Oral and Maxillofacial Surgery, Section of Dentistry, Seoul National University Bundang Hospital, Seongnam, Korea.
- KMID: 1824937
- DOI: http://doi.org/10.5051/jpis.2015.45.3.82
Abstract
- PURPOSE
This retrospective study evaluated the relationship between the timing of peri-implantitis diagnosis and marginal bone level after a 5-year follow-up of non-surgical peri-implantitis treatment.
METHODS
Thirty-three patients (69 implants) were given peri-implantitis diagnosis in 2008-2009 in Seoul National University Bundang Hospital. Among them, 31 implants from 16 patients were included in this study. They were treated non-surgically in this hospital, and came for regular maintenance visits for at least 5 years after peri-implantitis treatment. Radiographic marginal bone levels at each interval were measured and statistical analysis was performed.
RESULTS
Timing of peri-implantitis was one of the significant factors affecting initial bone loss and total bone loss not additional bone after peri-implantitis diagnosis. Patients with cardiovascular disease and diabetic mellitus were positively influenced on both initial bone loss and total bone loss. Patients who needed periodontal treatment after implant placement showed a negative effect on bone loss compared to those who needed periodontal treatment before implant placement during entire periods. Implant location also significantly influenced on amounts of bone loss. Mandibular implants showed less bone loss than maxillary implants. Among surgical factors, combined use of autogenous and xenogenic bone graft materials showed a negative effect on bone loss compared to autogenous bone graft materials. Use of membrane negatively affected on initial bone loss but positively on additional bone loss and total bone loss. Thread exposure showed positive effects on initial bone loss and total bone loss.
CONCLUSIONS
Early peri-implantitis diagnosis led to early non-surgical intervention for peri-implantitis treatment, which resulted in the maintenance of the bone level as well as preservation of the implant.
MeSH Terms
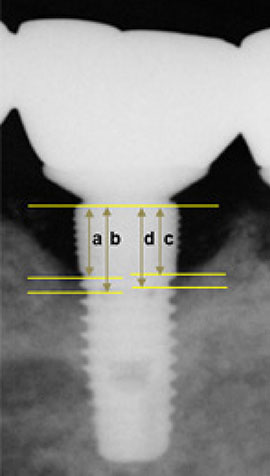
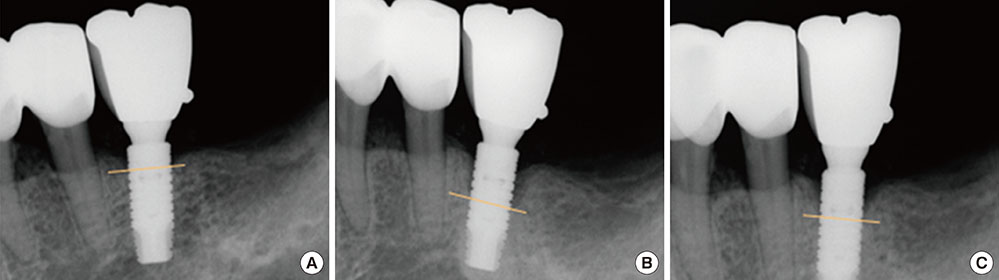
Figure
Reference
-
1. Lekholm U, Gunne J, Henry P, Higuchi K, Lindén U, Bergström C, et al. Survival of the Brånemark implant in partially edentulous jaws: a 10-year prospective multicenter study. Int J Oral Maxillofac Implants. 1999; 14:639–645.2. Schmidlin K, Schnell N, Steiner S, Salvi GE, Pjetursson B, Matuliene G, et al. Complication and failure rates in patients treated for chronic periodontitis and restored with single crowns on teeth and/or implants. Clin Oral Implants Res. 2010; 21:550–557.
Article3. Snauwaert K, Duyck J, van Steenberghe D, Quirynen M, Naert I. Time dependent failure rate and marginal bone loss of implant supported prostheses: a 15-year follow-up study. Clin Oral Investig. 2000; 4:13–20.
Article4. Esposito M, Hirsch JM, Lekholm U, Thomsen P. Biological factors contributing to failures of osseointegrated oral implants. (I). Success criteria and epidemiology. Eur J Oral Sci. 1998; 106:527–551.
Article5. Rosenberg ES, Cho SC, Elian N, Jalbout ZN, Froum S, Evian CI. A comparison of characteristics of implant failure and survival in periodontally compromised and periodontally healthy patients: a clinical report. Int J Oral Maxillofac Implants. 2004; 19:873–879.6. Berglundh T, Gotfredsen K, Zitzmann NU, Lang NP, Lindhe J. Spontaneous progression of ligature induced peri-implantitis at implants with different surface roughness: an experimental study in dogs. Clin Oral Implants Res. 2007; 18:655–661.
Article7. Heitz-Mayfield LJ. Peri-implant diseases: diagnosis and risk indicators. J Clin Periodontol. 2008; 35:292–304.
Article8. Berglundh T, Lindhe J, Marinello C, Ericsson I, Liljenberg B. Soft tissue reaction to de novo plaque formation on implants and teeth. An experimental study in the dog. Clin Oral Implants Res. 1992; 3:1–8.
Article9. Zitzmann NU, Berglundh T, Marinello CP, Lindhe J. Experimental peri-implant mucositis in man. J Clin Periodontol. 2001; 28:517–523.
Article10. Zitzmann NU, Berglundh T. Definition and prevalence of peri-implant diseases. J Clin Periodontol. 2008; 35:286–291.
Article11. Fransson C, Tomasi C, Pikner SS, Gröndahl K, Wennström JL, Leyland AH, et al. Severity and pattern of peri-implantitis-associated bone loss. J Clin Periodontol. 2010; 37:442–448.
Article12. Koldsland OC, Scheie AA, Aass AM. Prevalence of peri-implantitis related to severity of the disease with different degrees of bone loss. J Periodontol. 2010; 81:231–238.
Article13. Marrone A, Lasserre J, Bercy P, Brecx MC. Prevalence and risk factors for peri-implant disease in Belgian adults. Clin Oral Implants Res. 2013; 24:934–940.
Article14. Roos-Jansåker AM, Lindahl C, Renvert H, Renvert S. Nine- to fourteen-year follow-up of implant treatment. Part II: presence of peri-implant lesions. J Clin Periodontol. 2006; 33:290–295.
Article15. Zeza B, Pilloni A. Peri-implant mucositis treatments in humans: a systematic review. Ann Stomatol (Roma). 2012; 3:83–89.16. Sanz M, Chapple IL. Working Group 4 of the VIII European Workshop on Periodontology. Clinical research on peri-implant diseases: consensus report of Working Group 4. J Clin Periodontol. 2012; 39:Suppl 12. 202–206.
Article17. Roos-Jansåker AM, Renvert S, Egelberg J. Treatment of peri-implant infections: a literature review. J Clin Periodontol. 2003; 30:467–485.
Article18. Leonhardt A, Renvert S, Dahlén G. Microbial findings at failing implants. Clin Oral Implants Res. 1999; 10:339–345.
Article19. Mombelli A, Lang NP. The diagnosis and treatment of peri-implantitis. Periodontol 2000. 1998; 17:63–76.
Article20. Lang NP, Mombelli A, Tonetti MS, Brägger U, Hämmerle CH. Clinical trials on therapies for peri-implant infections. Ann Periodontol. 1997; 2:343–356.
Article21. Lang NP, Wilson TG, Corbet EF. Biological complications with dental implants: their prevention, diagnosis and treatment. Clin Oral Implants Res. 2000; 11:Suppl 1. 146–155.
Article22. Roccuzzo M, Bonino L, Dalmasso P, Aglietta M. Long-term results of a three arms prospective cohort study on implants in periodontally compromised patients: 10-year data around sandblasted and acid-etched (SLA) surface. Clin Oral Implants Res. 2014; 25:1105–1112.
Article23. Cecchinato D, Parpaiola A, Lindhe J. A cross-sectional study on the prevalence of marginal bone loss among implant patients. Clin Oral Implants Res. 2013; 24:87–90.
Article24. Charalampakis G, Rabe P, Leonhardt A, Dahlén G. A follow-up study of peri-implantitis cases after treatment. J Clin Periodontol. 2011; 38:864–871.
Article25. Armitage GC. Development of a classification system for periodontal diseases and conditions. Ann Periodontol. 1999; 4:1–6.
Article26. Renvert S, Aghazadeh A, Hallström H, Persson GR. Factors related to peri-implantitis - a retrospective study. Clin Oral Implants Res. 2014; 25:522–529.27. Schwarz F, Jepsen S, Herten M, Sager M, Rothamel D, Becker J. Influence of different treatment approaches on non-submerged and submerged healing of ligature induced peri-implantitis lesions: an experimental study in dogs. J Clin Periodontol. 2006; 33:584–595.
Article28. Checchi L, Montevecchi M, Gatto MR, Trombelli L. Retrospective study of tooth loss in 92 treated periodontal patients. J Clin Periodontol. 2002; 29:651–656.
Article29. Fardal Ø, Linden GJ. Tooth loss and implant outcomes in patients refractory to treatment in a periodontal practice. J Clin Periodontol. 2008; 35:733–738.
Article30. Lagervall M, Jansson LE. Treatment outcome in patients with peri-implantitis in a periodontal clinic: a retrospective study. J Periodontol. 2013; 84:1365–1373.
Article31. Serino G, Ström C. Peri-implantitis in partially edentulous patients: association with inadequate plaque control. Clin Oral Implants Res. 2009; 20:169–174.
Article32. Waerhaug J. Healing of the dento-epithelial junction following subgingival plaque control. II: As observed on extracted teeth. J Periodontol. 1978; 49:119–134.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Unusual bone regeneration following resective surgery and decontamination of peri-implantitis: a 6-year follow-up
- Full mouth rehabilitation in a patient with peri-implantitis: A case report
- Combined surgical therapy for the treatment of combined supraand intrabony defects in peri-implantitis
- Peri-Implantitis: Two Years Retrospective Study
- Adjunctive use of Gel-type Desiccating Agent for Regenerative Surgical Treatment of Peri-implantitis in Patients with Inaccessible Implant Surface: A Case Report