J Korean Soc Radiol.
2015 Jul;73(1):11-17. 10.3348/jksr.2015.73.1.11.
Stent Graft Placement for Dysfunctional Arteriovenous Grafts
- Affiliations
-
- 1Department of Radiology, CHA Bundang Medical Center, College of Medicine, CHA University, Seongnam, Korea.
- 2Department of Radiology, Chungnam National University Hospital, Daejeon, Korea. starzan@chol.com
- 3Department of Surgery, Chungnam National University Hospital, Daejeon, Korea.
- KMID: 1823917
- DOI: http://doi.org/10.3348/jksr.2015.73.1.11
Abstract
- PURPOSE
This study aimed to evaluate the usefulness and outcomes of stent graft use in dysfunctional arteriovenous grafts.
MATERIALS AND METHODS
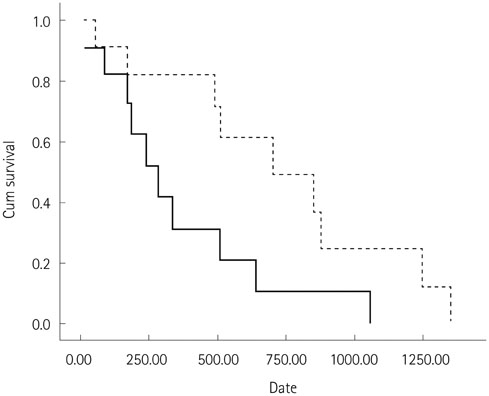
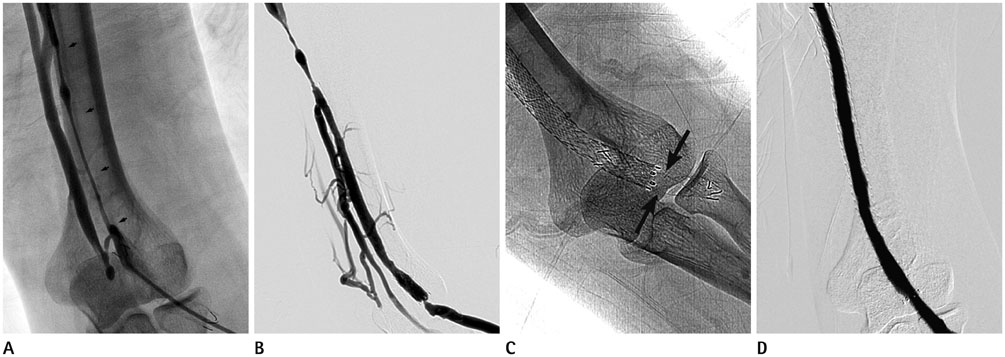
Eleven patients who underwent stent graft placement for a dysfunctional hemodialysis graft were included in this retrospective study. Expanded polytetrafluoroethylene covered stent grafts were placed at the venous anastomosis site in case of pseudoaneurysm, venous laceration, elastic recoil or residual restenosis despite the repeated angioplasty. The patency of the arteriovenous graft was evaluated using Kaplan-Meier analysis.
RESULTS
Primary and secondary mean patency was 363 days and 741 days. Primary patency at 3, 6, and 12 months was 82%, 73%, and 32%, respectively. Secondary patency at the 3, 6, 12, 24, and 36 months was improved to 91%, 82%, 82%, 50%, and 25%, respectively. Fractures of the stent graft were observed in 2 patients, but had no effect on the patency.
CONCLUSION
Stent graft placement in dysfunctional arteriovenous graft is useful and effective in prolonging graft patency.
MeSH Terms
Figure
Reference
-
1. Ravari H, Kazemzade GH, Modaghegh MH, Khashayar P. Patency rate and complications of polytetrafluoroethylene grafts compared with polyurethane grafts for hemodialysis access. Ups J Med Sci. 2010; 115:245–248.2. Clark TW, Hirsch DA, Jindal KJ, Veugelers PJ, LeBlanc J. Outcome and prognostic factors of restenosis after percutaneous treatment of native hemodialysis fistulas. J Vasc Interv Radiol. 2002; 13:51–59.3. Tessitore N, Mansueto G, Bedogna V, Lipari G, Poli A, Gammaro L, et al. A prospective controlled trial on effect of percutaneous transluminal angioplasty on functioning arteriovenous fistulae survival. J Am Soc Nephrol. 2003; 14:1623–1627.4. Rajan DK, Clark TW. Patency of Wallstents placed at the venous anastomosis of dialysis grafts for salvage of angioplasty-induced rupture. Cardiovasc Intervent Radiol. 2003; 26:242–245.5. Kariya S, Tanigawa N, Kojima H, Komemushi A, Shomura Y, Shiraishi T, et al. Peripheral stent placement in hemodialysis grafts. Cardiovasc Intervent Radiol. 2009; 32:960–966.6. Maya ID, Allon M. Outcomes of thrombosed arteriovenous grafts: comparison of stents vs angioplasty. Kidney Int. 2006; 69:934–937.7. Sreenarasimhaiah VP, Margassery SK, Martin KJ, Bander SJ. Salvage of thrombosed dialysis access grafts with venous anastomosis stents. Kidney Int. 2005; 67:678–684.8. Haskal ZJ, Trerotola S, Dolmatch B, Schuman E, Altman S, Mietling S, et al. Stent graft versus balloon angioplasty for failing dialysis-access grafts. N Engl J Med. 2010; 362:494–503.9. Webb KM, Cull DL, Carsten CG 3rd, Johnson BL, Taylor SM. Outcome of the use of stent grafts to salvage failed arteriovenous accesses. Ann Vasc Surg. 2010; 24:34–38.10. Nassar GM, Suki D, Rhee E, Khan AJ, Nguyen B, Achkar K. Outcomes of arteriovenous grafts following simultaneous thrombectomy and stent graft placement across the venous anastomosis. Semin Dial. 2014; 27:639–644.11. Karnabatidis D, Kitrou P, Spiliopoulos S, Katsanos K, Diamantopoulos A, Christeas N, et al. Stent-grafts versus angioplasty and/or bare metal stents for failing arteriovenous grafts: a cross-over longitudinal study. J Nephrol. 2013; 26:389–395.12. Chan MG, Miller FJ, Valji K, Bansal A, Kuo MD. Evaluating patency rates of an ultralow-porosity expanded polytetrafluoroethylene covered stent in the treatment of venous stenosis in arteriovenous dialysis circuits. J Vasc Interv Radiol. 2014; 25:183–189.13. Dolmatch BL, Duch JM, Winder R, Butler GM, Kershen M, Patel R, et al. Salvage of angioplasty failures and complications in hemodialysis arteriovenous access using the FLUENCY Plus Stent Graft: technical and 180-day patency results. J Vasc Interv Radiol. 2012; 23:479–487.14. Bent CL, Rajan DK, Tan K, Simons ME, Jaskolka J, Kachura J, et al. Effectiveness of stent-graft placement for salvage of dysfunctional arteriovenous hemodialysis fistulas. J Vasc Interv Radiol. 2010; 21:496–502.15. Vesely TM, Amin MZ, Pilgram T. Use of stents and stent grafts to salvage angioplasty failures in patients with hemodialysis grafts. Semin Dial. 2008; 21:100–104.16. Dale JD, Dolmatch BL, Duch JM, Winder R, Davidson IJ. Expanded polytetrafluoroethylene-covered stent treatment of angioplasty-related extravasation during hemodialysis access intervention: technical and 180-day patency. J Vasc Interv Radiol. 2010; 21:322–326.17. Gupta M, Rajan DK, Tan KT, Sniderman KW, Simons ME. Use of expanded polytetrafluoroethylene-covered nitinol stents for the salvage of dysfunctional autogenous hemodialysis fistulas. J Vasc Interv Radiol. 2008; 19:950–954.18. Shemesh D, Goldin I, Zaghal I, Berlowitz D, Raveh D, Olsha O. Angioplasty with stent graft versus bare stent for recurrent cephalic arch stenosis in autogenous arteriovenous access for hemodialysis: a prospective randomized clinical trial. J Vasc Surg. 2008; 48:1524–1531. 1531.e1–1531.e2.19. Anaya-Ayala JE, Smolock CJ, Colvard BD, Naoum JJ, Bismuth J, Lumsden AB, et al. Efficacy of covered stent placement for central venous occlusive disease in hemodialysis patients. J Vasc Surg. 2011; 54:754–759.20. Jones RG, Willis AP, Jones C, McCafferty IJ, Riley PL. Long-term results of stent-graft placement to treat central venous stenosis and occlusion in hemodialysis patients with arteriovenous fistulas. J Vasc Interv Radiol. 2011; 22:1240–1245.21. Kundu S, Modabber M, You JM, Tam P, Nagai G, Ting R. Use of PTFE stent grafts for hemodialysis-related central venous occlusions: intermediate-term results. Cardiovasc Intervent Radiol. 2011; 34:949–957.22. Welber A, Schur I, Sofocleous CT, Cooper SG, Patel RI, Peck SH. Endovascular stent placement for angioplasty-induced venous rupture related to the treatment of hemodialysis grafts. J Vasc Interv Radiol. 1999; 10:547–551.23. Vogel PM, Parise C. SMART stent for salvage of hemodialysis access grafts. J Vasc Interv Radiol. 2004; 15:1051–1060.24. Yoon YC, Shin BS, Ahn M, Park MH, Ohm JY, Kim HJ. Comparison of a nitinol stent versus balloon angioplasty for treatment of a dysfunctional arteriovenous graft. J Korean Soc Radiol. 2012; 66:519–526.25. Liang HL, Pan HB, Lin YH, Chen CY, Chung HM, Wu TH, et al. Metallic stent placement in hemodialysis graft patients after insufficient balloon dilation. Korean J Radiol. 2006; 7:118–124.26. Kakisis JD, Avgerinos E, Giannakopoulos T, Moulakakis K, Papapetrou A, Liapis CD. Balloon angioplasty vs nitinol stent placement in the treatment of venous anastomotic stenoses of hemodialysis grafts after surgical thrombectomy. J Vasc Surg. 2012; 55:472–478.27. Vogel PM, Parise C. Comparison of SMART stent placement for arteriovenous graft salvage versus successful graft PTA. J Vasc Interv Radiol. 2005; 16:1619–1626.28. Chan MR, Bedi S, Sanchez RJ, Young HN, Becker YT, Kellerman PS, et al. Stent placement versus angioplasty improves patency of arteriovenous grafts and blood flow of arteriovenous fistulae. Clin J Am Soc Nephrol. 2008; 3:699–705.29. Wong G, Li JM, Hendricks G, Eslami MH, Rohrer MJ, Cutler BS. Inhibition of experimental neointimal hyperplasia by recombinant human thrombomodulin coated ePTFE stent grafts. J Vasc Surg. 2008; 47:608–615.30. Saxon RR, Coffman JM, Gooding JM, Ponec DJ. Long-term patency and clinical outcome of the Viabahn stent-graft for femoropopliteal artery obstructions. J Vasc Interv Radiol. 2007; 18:1341–1349. quiz 135031. Kedora J, Hohmann S, Garrett W, Munschaur C, Theune B, Gable D. Randomized comparison of percutaneous Viabahn stent grafts vs prosthetic femoral-popliteal bypass in the treatment of superficial femoral arterial occlusive disease. J Vasc Surg. 2007; 45:10–16. discussion 16
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of a Nitinol Stent versus Balloon Angioplasty for Treatment of a Dysfunctional Arteriovenous Graft
- Bare-Metal Stent in Dysfunctional Hemodialysis Access: An Assessment of Circuit Patency according to Access Type and Stent Location
- Temporary Placement of Stent Grafts in Postsurgical Benign Biliary Strictures: a Single Center Experience
- Intervention of the Dysfunctional and Thrombosed Autogenous Vascular Access
- Percutaneous Intervention in Axillary Loop-Configured Arteriovenous Grafts for Chronic Hemodialysis Patients