Intestinal Stricture in Crohn's Disease
- Affiliations
-
- 1Department of Gastroenterology, Mackay Memorial Hospital, Taipei, Taiwan.
- 2Department of Gastroenterology, Mackay Junior College of Medicine, Nursing and Management, Taipei, Taiwan.
- 3Department of Gastroenterology, Mackay Medical College, New Taipei, Taiwan.
- 4Department of Internal Medicine, National Taiwan University Hospital and College of Medicine, Taipei, Taiwan. shuchenwei@ntu.edu.tw
- 5Department of Integrated Diagnostics and Therapeutics, National Taiwan University Hospital and College of Medicine, Taipei, Taiwan.
- 6Department of Medical Imaging, National Taiwan University Hospital and College of Medicine, Taipei, Taiwan.
- KMID: 1807373
- DOI: http://doi.org/10.5217/ir.2015.13.1.19
Abstract
- Crohn's disease (CD) is a disease with chronic inflammation of unknown etiology involving any part of the gastrointestinal tract. The incidence and prevalence of CD are increasing recently in Asia. Half of the CD patients will have intestinal complications, such as strictures or fistulas, within 20 years after diagnosis. Twenty-five percentage of CD patients have had at least one small bowel stricture and 10% have had at least one colonic stricture and lead to significant complications. Most of these patients will require at least one surgery during their lifetime. Early diagnosis and evaluation with adequate managements for the patients can prevent disability and mortality of these patient. Here, we reviewed the current incidence of CD with stricture, the etiology of stricture, and how to diagnose and manage the stricture.
MeSH Terms
Figure
Cited by 4 articles
-
Quality Indicators for Small Bowel Capsule Endoscopy
Ki-Nam Shim, Seong Ran Jeon, Hyun Joo Jang, Jinsu Kim, Yun Jeong Lim, Kyeong Ok Kim, Hyun Joo Song, Hyun Seok Lee, Jae Jun Park, Ji Hyun Kim, Jaeyoung Chun, Soo Jung Park, Dong-Hoon Yang, Yang Won Min, Bora Keum, Bo-In Lee
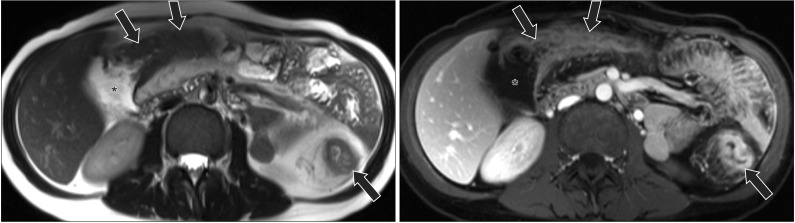
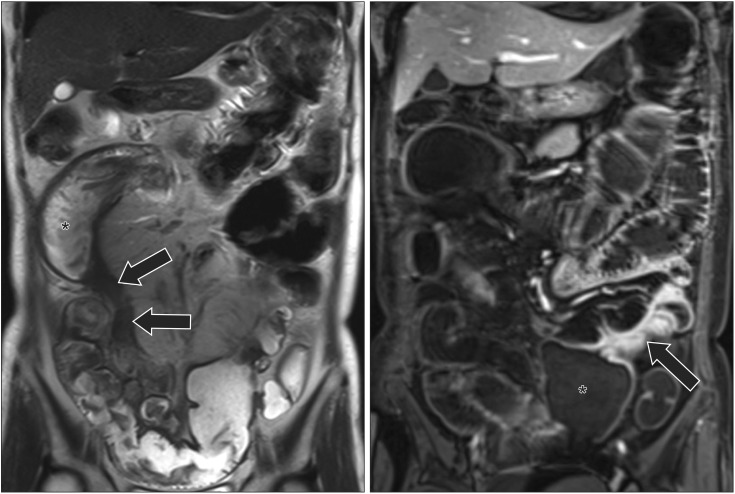
Clin Endosc. 2017;50(2):148-160. doi: 10.5946/ce.2017.030.Crohn’s disease at radiological imaging: focus on techniques and intestinal tract
Giuseppe Cicero, Silvio Mazziotti
Intest Res. 2021;19(4):365-378. doi: 10.5217/ir.2020.00097.Endoscopic balloon dilations for strictures of rectum, ileocecal valve and duodenum in a patient with X-linked inhibitor of apoptosis deficiency: a case report
Shinsuke Otagiri, Takehiko Katsurada, Kensuke Sakurai, Junichi Sugita, Naoya Sakamoto
Intest Res. 2022;20(2):274-277. doi: 10.5217/ir.2021.00029.Management of Crohn's disease in Taiwan: consensus guideline of the Taiwan Society of Inflammatory Bowel Disease
Shu-Chen Wei, Ting-An Chang, Te-Hsin Chao, Jinn-Shiun Chen, Jen-Wei Chou, Yenn-Hwei Chou, Chiao-Hsiung Chuang, Wen-Hung Hsu, Tien-Yu Huang, Tzu-Chi Hsu, Chun-Chi Lin, Hung-Hsin Lin, Jen-Kou Lin, Wei-Chen Lin, Yen-Hsuan Ni, Ming-Jium Shieh, I-Lun Shih, Chia-Tung Shun, Yuk-Ming Tsang, Cheng-Yi Wang, Horng-Yuan Wang, Meng-Tzu Weng, Deng-Chyang Wu, Wen-Chieh Wu, Hsu-Heng Yen, Jau-Min Wong
Intest Res. 2017;15(3):285-310. doi: 10.5217/ir.2017.15.3.285.
Reference
-
1. Prideaux L, Kamm MA, De Cruz PP, Chan FK, Ng SC. Inflammatory bowel disease in Asia: a systematic review. J Gastroenterol Hepatol. 2012; 27:1266–1280. PMID: 22497584.
Article2. Silverberg MS, Satsangi J, Ahmad T, et al. Toward an integrated clinical, molecular and serological classification of inflammatory bowel disease: report of a Working Party of the 2005 Montreal World Congress of Gastroenterology. Can J Gastroenterol. 2005; 19(Suppl A):5A–36A.
Article4. Chan G, Fefferman DS, Farrell RJ. Endoscopic assessment of inflammatory bowel disease: colonoscopy/esophagogastroduodenoscopy. Gastroenterol Clin North Am. 2012; 41:271–290. PMID: 22500517.
Article5. Paine E, Shen B. Endoscopic therapy in inflammatory bowel diseases (with videos). Gastrointest Endosc. 2013; 78:819–835. PMID: 24139079.6. Burke JP, Mulsow JJ, O'Keane C, Docherty NG, Watson RW, O'Connell PR. Fibrogenesis in Crohn's disease. Am J Gastroenterol. 2007; 102:439–448. PMID: 17156147.
Article7. Cosnes J, Nion-Larmurier I, Beaugerie L, Afchain P, Tiret E, Gendre JP. Impact of the increasing use of immunosuppressants in Crohn's disease on the need for intestinal surgery. Gut. 2005; 54:237–241. PMID: 15647188.
Article8. Peyrin-Biroulet L, Loftus EV Jr, Colombel JF, Sandborn WJ. The natural history of adult Crohn's disease in population-based cohorts. Am J Gastroenterol. 2010; 105:289–297. PMID: 19861953.
Article9. Ben-Horin S, Chowers Y. Review article: loss of response to anti-TNF treatments in Crohn's disease. Aliment Pharmacol Ther. 2011; 33:987–995. PMID: 21366636.
Article10. Morita N, Toki S, Hirohashi T, et al. Incidence and prevalence of inflammatory bowel disease in Japan: nationwide epidemiological survey during the year 1991. J Gastroenterol. 1995; 30(Suppl 8):1–4. PMID: 8563866.11. Kitahora T, Utsunomiya T, Yokota A. Epidemiological study of ulcerative colitis in Japan: incidence and familial occurrence. The Epidemiology Group of the Research Committee of Inflammatory Bowel Disease in Japan. J Gastroenterol. 1995; 30(Suppl 8):5–8. PMID: 8563890.12. Yao T, Matsui T, Hiwatashi N. Crohn's disease in Japan: diagnostic criteria and epidemiology. Dis Colon Rectum. 2000; 43:S85–S93. PMID: 11052483.13. Higashi A, Watanabe Y, Ozasa K, Hayashi K, Aoike A, Kawai K. Prevalence and mortality of ulcerative colitis and Crohn's disease in Japan. Gastroenterol Jpn. 1988; 23:521–526. PMID: 3215436.
Article14. Asakura K, Nishiwaki Y, Inoue N, Hibi T, Watanabe M, Takebayashi T. Prevalence of ulcerative colitis and Crohn's disease in Japan. J Gastroenterol. 2009; 44:659–665. PMID: 19424654.
Article15. Shin DH, Sinn DH, Kim YH, et al. Increasing incidence of inflammatory bowel disease among young men in Korea between 2003 and 2008. Dig Dis Sci. 2011; 56:1154–1159. PMID: 20844953.16. Yang SK, Yun S, Kim JH, et al. Epidemiology of inflammatory bowel disease in the Songpa-Kangdong district, Seoul, Korea, 1986-2005: a KASID study. Inflamm Bowel Dis. 2008; 14:542–549. PMID: 17941073.
Article17. Wei SC, Lin MH, Tung CC, et al. A nationwide population-based study of the inflammatory bowel diseases between 1998 and 2008 in Taiwan. BMC Gastroenterol. 2013; 13:166. PMID: 24314308.
Article18. Yamamoto T, Watanabe T. Surgery for luminal Crohn's disease. World J Gastroenterol. 2014; 20:78–90. PMID: 24415860.
Article19. Cleynen I, Gonzalez JR, Figueroa C, et al. Genetic factors conferring an increased susceptibility to develop Crohn's disease also influence disease phenotype: results from the IBDchip European Project. Gut. 2013; 62:1556–1565. PMID: 23263249.
Article20. Yano Y, Matsui T, Hirai F, et al. Cancer risk in Japanese Crohn's disease patients: investigation of the standardized incidence ratio. J Gastroenterol Hepatol. 2013; 28:1300–1305. PMID: 23488881.21. Ye BD, Yang SK, Cho YK, et al. Clinical features and long-term prognosis of Crohn's disease in Korea. Scand J Gastroenterol. 2010; 45:1178–1185. PMID: 20560811.
Article22. Wei SC, Ni YH, Yang HI, et al. A hospital-based study of clinical and genetic features of Crohn's disease. J Formos Med Assoc. 2011; 110:600–606. PMID: 21930071.
Article23. Rieder F, Fiocchi C. Mechanisms of tissue remodeling in inflammatory bowel disease. Dig Dis. 2013; 31:186–193. PMID: 24030223.
Article24. Rieder F, Fiocchi C. Intestinal fibrosis in inflammatory bowel disease - Current knowledge and future perspectives. J Crohns Colitis. 2008; 2:279–290. PMID: 21172225.
Article25. Armaka M, Apostolaki M, Jacques P, Kontoyiannis DL, Elewaut D, Kollias G. Mesenchymal cell targeting by TNF as a common pathogenic principle in chronic inflammatory joint and intestinal diseases. J Exp Med. 2008; 205:331–337. PMID: 18250193.26. Lichtenstein GR, Olson A, Travers S, et al. Factors associated with the development of intestinal strictures or obstructions in patients with Crohn's disease. Am J Gastroenterol. 2006; 101:1030–1038. PMID: 16606351.
Article27. Gelbmann CM, Mestermann S, Gross V, Kollinger M, Scholmerich J, Falk W. Strictures in Crohn's disease are characterised by an accumulation of mast cells colocalised with laminin but not with fibronectin or vitronectin. Gut. 1999; 45:210–217. PMID: 10403732.
Article28. Graham MF. Pathogenesis of intestinal strictures in Crohn's disease-an update. Inflamm Bowel Dis. 1995; 1:220–227. PMID: 23282393.
Article29. Hugot JP, Laurent-Puig P, Gower-Rousseau C, et al. Mapping of a susceptibility locus for Crohn's disease on chromosome 16. Nature. 1996; 379:821–823. PMID: 8587604.
Article30. Hugot JP. Genetic origin of IBD. Inflamm Bowel Dis. 2004; 10(Suppl 1):S11–S15. PMID: 15168824.31. Tung CC, Wong JM, Lee WC, et al. Combining TNFSF15 and ASCA IgA can be used as a predictor for the stenosis/perforating phenotype of Crohn's disease. J Gastroenterol Hepatol. 2014; 29:723–729. PMID: 24783249.
Article32. Rieder F, Zimmermann EM, Remzi FH, Sandborn WJ. Crohn's disease complicated by strictures: a systematic review. Gut. 2013; 62:1072–1084. PMID: 23626373.
Article33. Parente F, Maconi G, Bollani S, et al. Bowel ultrasound in assessment of Crohn's disease and detection of related small bowel strictures: a prospective comparative study versus x ray and intraoperative findings. Gut. 2002; 50:490–495. PMID: 11889068.
Article34. Migaleddu V, Scanu AM, Quaia E, et al. Contrast-enhanced ultrasonographic evaluation of inflammatory activity in Crohn's disease. Gastroenterology. 2009; 137:43–52. PMID: 19422826.
Article35. Horsthuis K, Bipat S, Bennink RJ, Stoker J. Inflammatory bowel disease diagnosed with US, MR, scintigraphy, and CT: meta-analysis of prospective studies. Radiology. 2008; 247:64–79. PMID: 18372465.36. Kralik R, Trnovsky P, Kopáčová M. Transabdominal ultrasonography of the small bowel. Gastroenterol Res Pract. doi: 10.1155/2013/896704. Published online 19 November 2013.
Article37. Dietrich CF. Significance of abdominal ultrasound in inflammatory bowel disease. Dig Dis. 2009; 27:482–493. PMID: 19897964.
Article38. Stidham RW, Xu J, Johnson LA, et al. Ultrasound elasticity imaging for detecting intestinal fibrosis and inflammation in rats and humans with Crohn's disease. Gastroenterology. 2011; 141:819–826. PMID: 21784048.
Article39. Masselli G, Gualdi G. CT and MR enterography in evaluating small bowel diseases: when to use which modality? Abdom Imaging. 2013; 38:249–259. PMID: 23011551.
Article40. Furukawa A, Saotome T, Yamasaki M, et al. Cross-sectional imaging in Crohn disease. Radiographics. 2004; 24:689–702. PMID: 15143222.41. Fiorino G, Bonifacio C, Malesci A, Balzarini L, Danese S. MRI in Crohn's disease--current and future clinical applications. Nat Rev Gastroenterol Hepatol. 2012; 9:23–31. PMID: 22105109.
Article42. Benitez JM, Meuwis MA, Reenaers C, Van Kemseke C, Meunier P, Louis E. Role of endoscopy, cross-sectional imaging and biomarkers in Crohn's disease monitoring. Gut. 2013; 62:1806–1816. PMID: 24203056.
Article43. Despott EJ, Gupta A, Burling D, et al. Effective dilation of small-bowel strictures by double-balloon enteroscopy in patients with symptomatic Crohn's disease (with video). Gastrointest Endosc. 2009; 70:1030–1036. PMID: 19640518.
Article44. Farmer RG, Hawk WA, Turnbull RB Jr. Indications for surgery in Crohn's disease: analysis of 500 cases. Gastroenterology. 1976; 71:245–250. PMID: 1084841.45. de Buck van Overstraeten A, Wolthuis A, D'Hoore A. Surgery for Crohn's disease in the era of biologicals: a reduced need or delayed verdict? World J Gastroenterol. 2012; 18:3828–3832. PMID: 22876034.46. Regueiro M, Schraut W, Baidoo L, et al. Infliximab prevents Crohn's disease recurrence after ileal resection. Gastroenterology. 2009; 136:441–450. PMID: 19109962.
Article47. de'Angelis N, Carra MC, Borrelli O, et al. Short- and long-term efficacy of endoscopic balloon dilation in Crohn's disease strictures. World J Gastroenterol. 2013; 19:2660–2667. PMID: 23674873.48. Van Assche G, Geboes K, Rutgeerts P. Medical therapy for Crohn's disease strictures. Inflamm Bowel Dis. 2004; 10:55–60. PMID: 15058528.
Article49. Brooker JC, Beckett CG, Saunders BP, Benson MJ. Long-acting steroid injection after endoscopic dilation of anastomotic Crohn's strictures may improve the outcome: a retrospective case series. Endoscopy. 2003; 35:333–337. PMID: 12664391.
Article50. Hassan C, Zullo A, De Francesco V, et al. Systematic review: Endoscopic dilatation in Crohn's disease. Aliment Pharmacol Ther. 2007; 26:1457–1464. PMID: 17903236.
Article51. Hoffmann JC, Heller F, Faiss S, et al. Through the endoscope balloon dilation of ileocolonic strictures: prognostic factors, complications, and effectiveness. Int J Colorectal Dis. 2008; 23:689–696. PMID: 18338175.52. Kwon YH, Jeon SW, Lee YK. Endoscopic management of refractory benign colorectal strictures. Clin Endosc. 2013; 46:472–475. PMID: 24143305.
Article53. Bonin EA, Baron TH. Update on the indications and use of colonic stents. Curr Gastroenterol Rep. 2010; 12:374–382. PMID: 20703837.
Article54. Lee JG, Yoo KH, Kwon CI, Ko KH, Hong SP. Angular positioning of stent increases bowel perforation after self-expandable metal stent placement for malignant colorectal obstruction. Clin Endosc. 2013; 46:384–389. PMID: 23964336.
Article55. Rejchrt S, Kopacova M, Brozik J, Bures J. Biodegradable stents for the treatment of benign stenoses of the small and large intestines. Endoscopy. 2011; 43:911–917. PMID: 21623562.
Article56. Lazarev M, Ullman T, Schraut WH, Kip KE, Saul M, Regueiro M. Small bowel resection rates in Crohn's disease and the indication for surgery over time: experience from a large tertiary care center. Inflamm Bowel Dis. 2010; 16:830–835. PMID: 19798731.57. Casillas S, Delaney CP. Laparoscopic surgery for inflammatory bowel disease. Dig Surg. 2005; 22:135–142. PMID: 16037671.
Article58. Casillas S, Delaney CP, Senagore AJ, Brady K, Fazio VW. Does conversion of a laparoscopic colectomy adversely affect patient outcome? Dis Colon Rectum. 2004; 47:1680–1685. PMID: 15540299.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Treatment of Rectal Stricture with Crohn's Disease Using Local Steroid Injection Following Dilation by Bougienation
- Current status of endoscopic balloon dilation for Crohn's disease
- High grade anorectal stricture complicating Crohn's disease: endoscopic treatment using insulated-tip knife
- A Case of Crohns Disease Misdiagnosed as Intestinal Tuberculosis
- Surgery in Pediatric Crohn's Disease: Indications, Timing and Post-Operative Management