Korean J Hepatobiliary Pancreat Surg.
2015 Feb;19(1):30-34. 10.14701/kjhbps.2015.19.1.30.
Customized left-sided hepatectomy and bile duct resection for perihilar cholangiocarcinoma in a patient with left-sided gallbladder and multiple combined anomalies
- Affiliations
-
- 1Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. shwang@amc.seoul.kr
- 2Department of Hepatobiliary and Liver Transplant Unit, General Surgery Department, Prince Sultan Military Medical City, Riyadh, Saudi Arabia.
- 3Department of Gastroenterology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- KMID: 1802237
- DOI: http://doi.org/10.14701/kjhbps.2015.19.1.30
Abstract
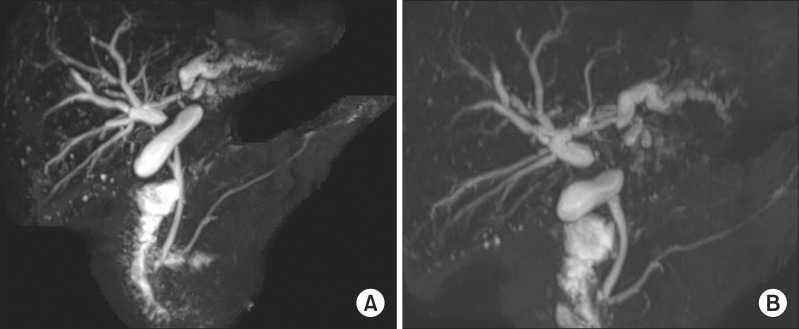
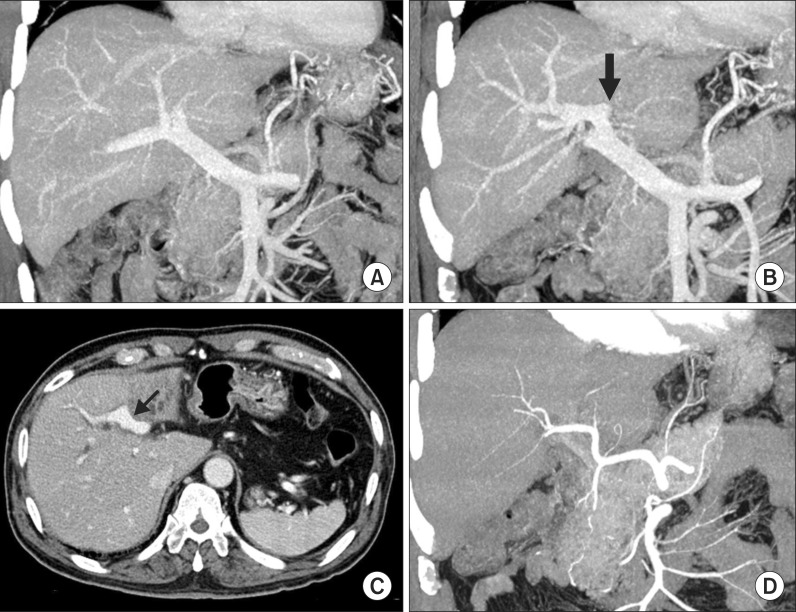
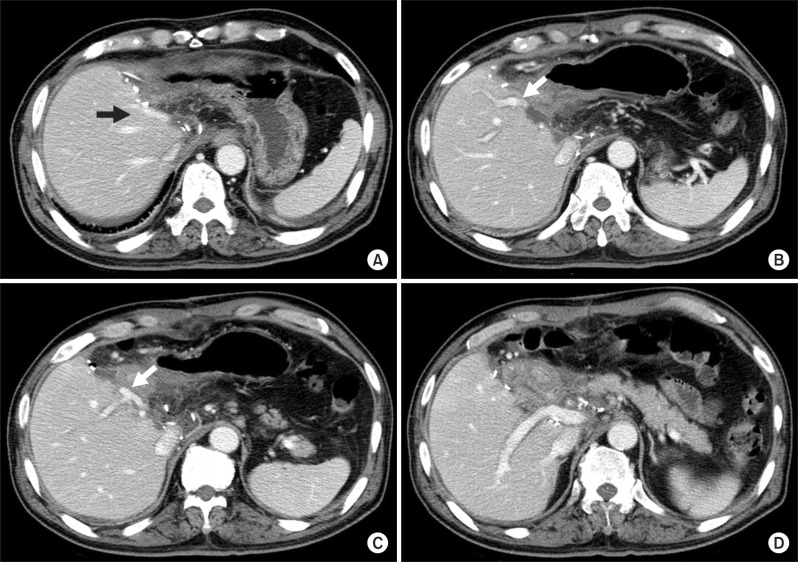
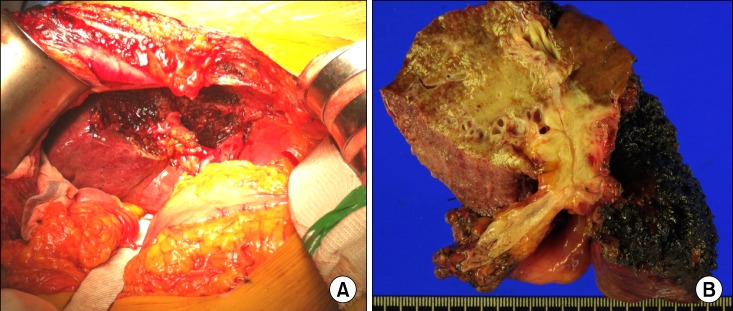
- Left-sided gallbladder (LSGB) is a rare anomaly, but it is often associated with multiple combined variations of the liver anatomy. We present the case of a patient with LSGB who underwent successful resection of perihilar cholangiocarcinoma. The patient was a 67-year-old male who presented with upper abdominal pain and obstructive jaundice. Initial imaging studies led to the diagnosis of Bismuth-Corlette type IIIB perihilar cholangiocarcinoma. Due to the unique location of the gallbladder and combined multiple hepatic anomalies, LSGB was highly suspected. During surgery after hilar dissection, we recognized that the tumor was located at the imaginary hilar bile duct bifurcation, but its actual location was corresponding to the biliary confluence of the left median and lateral sections. The extent of resection included extended left lateral sectionectomy, caudate lobe resection, and bile duct resection. Since some of the umbilical portion of the portal vein was invaded, it was resected and repaired with a portal vein branch patch. Due to anatomical variation of the biliary system, only one right-sided duct was reconstructed. The patient recovered uneventfully without any complication. LSGB should be recognized as a constellation of multiple hepatic anomalies, and therefore, thorough investigations are necessary to enable the performance of safe hepatic and biliary resections.
MeSH Terms
Figure
Reference
-
1. Hwang S, Lee SG, Park KM, Lee YJ, Ahn CS, Kim KH, et al. Hepatectomy of living donors with a left-sided gallbladder and multiple combined anomalies for adult-to-adult living donor liver transplantation. Liver Transpl. 2004; 10:141–146. PMID: 14755792.
Article2. Kaneoka Y, Yamaguchi A, Isogai M, Harada T. Hepatectomy for cholangiocarcinoma complicated with right umbilical portion: anomalous configuration of the intrahepatic biliary tree. J Hepatobiliary Pancreat Surg. 2000; 7:321–326. PMID: 10982634.
Article3. Nagai M, Kubota K, Kawasaki S, Takayama T, BandaiY , Makuuchi M. Are left-sided gallbladders really located on the left side? Ann Surg. 1997; 225:274–280. PMID: 9060583.
Article4. Asonuma K, Shapiro AM, Inomata Y, Uryuhara K, Uemoto S, Tanaka K. Living related liver transplantation from donors with the left-sided gallbladder/portal vein anomaly. Transplantation. 1999; 68:1610–1612. PMID: 10589965.
Article5. Ogawa T, Ohwada S, Ikeya T, Shiozaki H, Aiba S, Morishita Y. Left-sided gallbladder with anomalies of the intrahepatic portal vein and anomalous junction of the pancreaticobiliary ductal system: a case report. Hepatogastroenterology. 1995; 42:645–649. PMID: 8751228.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Laparoscopic cholecystectomy and common bile duct exploration for gallstone and common bile duct stone in a patient with a left-sided gallbladder: a case report
- Preduodenal Portal Vein and Left Sided Gallbladder in Hepatolithiasis Patient: A case report
- Left-sided Gallbladder: 2 cases
- Parenchyma-preserving hepatectomy including segments I + IV resection and bile duct resection in a patient with type IV perihilar cholangiocarcinoma: A case report with video clip
- Necrosectomy of hepatic left lateral section after blunt abdominal trauma in a patient who underwent central hepatectomy and bile duct resection for perihilar cholangiocarcinoma