Yonsei Med J.
2014 Sep;55(5):1246-1252. 10.3349/ymj.2014.55.5.1246.
Multidisciplinary Team Approach for Identifying Potential Candidate for Transcatheter Aortic Valve Implantation
- Affiliations
-
- 1Division of Cardiology, Severance Cardiovascular Hospital, Yonsei University College of Medicine, Seoul, Korea. mkhong61@yuhs.ac
- 2Severance Biomedical Science Institute, Yonsei University College of Medicine, Seoul, Korea.
- 3Division of Anesthesiology and Pain Medicine, Severance Cardiovascular Hospital, Yonsei University College of Medicine, Seoul, Korea.
- 4Division of Cardiovascular Surgery, Severance Cardiovascular Hospital, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 1799487
- DOI: http://doi.org/10.3349/ymj.2014.55.5.1246
Abstract
- PURPOSE
We sought to evaluate the clinical usefulness of decision making by a multidisciplinary heart team for identifying potential candidates for transcatheter aortic valve implantation (TAVI) in patients with symptomatic severe aortic stenosis.
MATERIALS AND METHODS
The multidisciplinary team consisted of two interventional cardiologists, two cardiovascular surgeons, one cardiac imaging specialist, and two cardiac anesthesiologists.
RESULTS
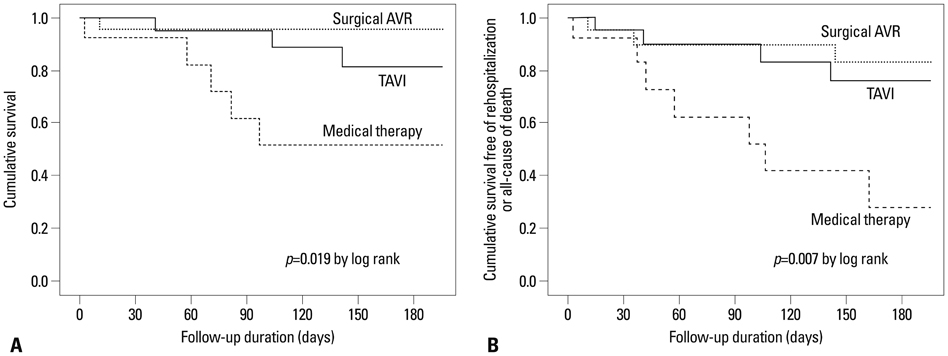
Out of 60 patients who were screened as potential TAVI candidates, 31 patients were initially recommended as appropriate for TAVI, and 20 of these 31 eventually underwent TAVI. Twenty-two patients underwent surgical aortic valve replacement (AVR), and 17 patients received only medical treatment. Patients who underwent TAVI and medical therapy were older than those who underwent surgical AVR (p<0.001). The logistic Euroscore was significantly highest in the TAVI group and lowest in the surgical AVR group (p=0.012). Most patients in the TAVI group (90%) and the surgical AVR group (91%) had severe cardiac symptoms, but only 47% in the medical therapy group had severe symptoms. The cumulative percentages of survival without re-hospitalization or all-cause death at 6 months for the surgical AVR, TAVI, and medical therapy groups were 84%, 75%, and 28%, respectively (p=0.007, by log-rank).
CONCLUSION
TAVI was recommended in half of the potential candidates following a multidisciplinary team approach and was eventually performed in one-third of these patients. One-third of the patients who were initially considered potential candidates received surgical AVR with favorable clinical outcomes.
MeSH Terms
Figure
Reference
-
1. Nkomo VT, Gardin JM, Skelton TN, Gottdiener JS, Scott CG, Enriquez-Sarano M. Burden of valvular heart diseases: a population-based study. Lancet. 2006; 368:1005–1011.
Article2. Bonow RO, Carabello BA, Chatterjee K, de Leon AC Jr, Faxon DP, Freed MD, et al. 2008 focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to revise the 1998 guidelines for the management of patients with valvular heart disease). Endorsed by the Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2008; 52:e1–e142.3. Iung B, Baron G, Butchart EG, Delahaye F, Gohlke-Bärwolf C, Levang OW, et al. A prospective survey of patients with valvular heart disease in Europe: The Euro Heart Survey on Valvular Heart Disease. Eur Heart J. 2003; 24:1231–1243.
Article4. Freed BH, Sugeng L, Furlong K, Mor-Avi V, Raman J, Jeevanandam V, et al. Reasons for nonadherence to guidelines for aortic valve replacement in patients with severe aortic stenosis and potential solutions. Am J Cardiol. 2010; 105:1339–1342.
Article5. Osswald BR, Gegouskov V, Badowski-Zyla D, Tochtermann U, Thomas G, Hagl S, et al. Overestimation of aortic valve replacement risk by EuroSCORE: implications for percutaneous valve replacement. Eur Heart J. 2009; 30:74–80.
Article6. Leontyev S, Walther T, Borger MA, Lehmann S, Funkat AK, Rastan A, et al. Aortic valve replacement in octogenarians: utility of risk stratification with EuroSCORE. Ann Thorac Surg. 2009; 87:1440–1445.
Article7. Piazza N, Wenaweser P, van Gameren M, Pilgrim T, Tzikas A, Otten A, et al. Relationship between the logistic EuroSCORE and the Society of Thoracic Surgeons Predicted Risk of Mortality score in patients implanted with the CoreValve ReValving system--a Bern-Rotterdam Study. Am Heart J. 2010; 159:323–329.
Article8. Kempfert J, Rastan A, Holzhey D, Linke A, Schuler G, van Linden A, et al. Transapical aortic valve implantation: analysis of risk factors and learning experience in 299 patients. Circulation. 2011; 124:11 Suppl. S124–S129.9. Kappetein AP, Head SJ, Généreux P, Piazza N, van Mieghem NM, Blackstone EH, et al. Updated standardized endpoint definitions for transcatheter aortic valve implantation: the Valve Academic Research Consortium-2 consensus document. J Am Coll Cardiol. 2012; 60:1438–1454.
Article10. Alli OO, Booker JD, Lennon RJ, Greason KL, Rihal CS, Holmes DR Jr. Transcatheter aortic valve implantation: assessing the learning curve. JACC Cardiovasc Interv. 2012; 5:72–79.11. Gurvitch R, Tay EL, Wijesinghe N, Ye J, Nietlispach F, Wood DA, et al. Transcatheter aortic valve implantation: lessons from the learning curve of the first 270 high-risk patients. Catheter Cardiovasc Interv. 2011; 78:977–984.12. Grube E, Schuler G, Buellesfeld L, Gerckens U, Linke A, Wenaweser P, et al. Percutaneous aortic valve replacement for severe aortic stenosis in high-risk patients using the second- and current third-generation self-expanding CoreValve prosthesis: device success and 30-day clinical outcome. J Am Coll Cardiol. 2007; 50:69–76.
Article13. Sinning JM, Ghanem A, Steinhäuser H, Adenauer V, Hammerstingl C, Nickenig G, et al. Renal function as predictor of mortality in patients after percutaneous transcatheter aortic valve implantation. JACC Cardiovasc Interv. 2010; 3:1141–1149.
Article14. Im E, Hong MK, Ko YG, Shin DH, Kim JS, Kim BK, et al. Comparison of early clinical outcomes following transcatheter aortic valve implantation versus surgical aortic valve replacement versus optimal medical therapy in patients older than 80 years with symptomatic severe aortic stenosis. Yonsei Med J. 2013; 54:596–602.
Article15. Cribier A, Eltchaninoff H, Tron C, Bauer F, Agatiello C, Sebagh L, et al. Early experience with percutaneous transcatheter implantation of heart valve prosthesis for the treatment of end-stage inoperable patients with calcific aortic stenosis. J Am Coll Cardiol. 2004; 43:698–703.
Article16. Webb JG, Pasupati S, Humphries K, Thompson C, Altwegg L, Moss R, et al. Percutaneous transarterial aortic valve replacement in selected high-risk patients with aortic stenosis. Circulation. 2007; 116:755–763.
Article17. Smith CR, Leon MB, Mack MJ, Miller DC, Moses JW, Svensson LG, et al. Transcatheter versus surgical aortic-valve replacement in high-risk patients. N Engl J Med. 2011; 364:2187–2198.
Article18. Dworakowski R, MacCarthy PA, Monaghan M, Redwood S, El-Gamel A, Young C, et al. Transcatheter aortic valve implantation for severe aortic stenosis-a new paradigm for multidisciplinary intervention: a prospective cohort study. Am Heart J. 2010; 160:237–243.
Article19. Bach DS, Cimino N, Deeb GM. Unoperated patients with severe aortic stenosis. J Am Coll Cardiol. 2007; 50:2018–2019.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Severe Aortic Stenosis Patient With High Operative Risk Treated by Transcatheter Aortic-Valve Implantation
- Expanding transcatheter aortic valve replacement into uncharted indications
- Echocardiography in Transcatheter Aortic Valve Implantation and Mitral Valve Clip
- Similar Morphology, but Different Function: Acute Improvement of Myocardial Longitudinal Strain after Percutaneous Transcatheter Aortic Valve Implantation Therapy in a Severe Aortic Stenosis Patient
- Recent updates in transcatheter aortic valve implantation