Brain Neurorehabil.
2014 Sep;7(2):126-130. 10.12786/bn.2014.7.2.126.
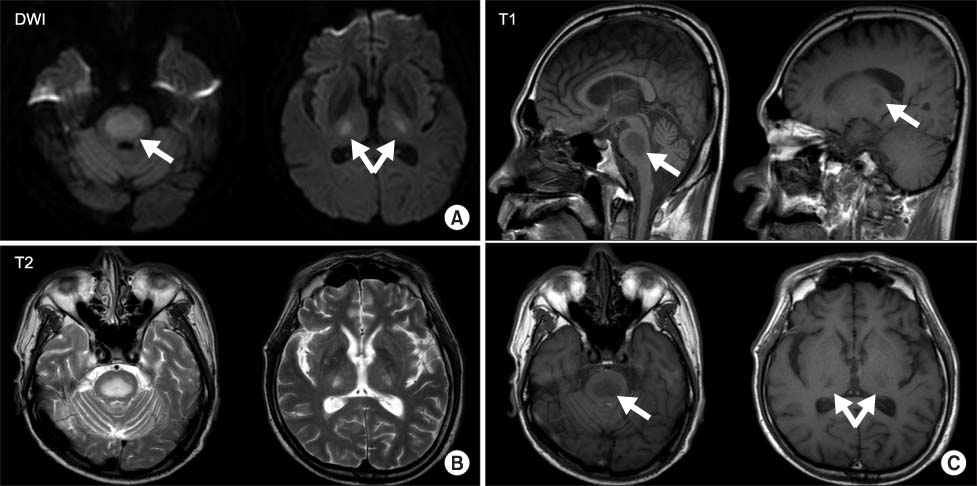
Recovery from a Complicated Case of Central Pontine and Extrapontine Myelinolysis by Dopaminergic Treatment: One-Year Follow-up: A Case Report
- Affiliations
-
- 1Department of Rehabilitation Medicine, College of Medicine, The Catholic University of Korea, Korea. lafolia@catholic.ac.kr
- KMID: 1797646
- DOI: http://doi.org/10.12786/bn.2014.7.2.126
Abstract
- Central pontine and extrapontine myelinolysis are well-recognized osmotic demyelination syndromes related to the rapid correction of hyponatremia, chronic alcoholism, and malnutrition. They are reported to show brain stem signs and various movement disorders. A 58-year-old man with a history of chronic alcoholism was admitted for dysarthria, dysphagia, and gait disturbance that had developed five days after a right forearm cellulitis. Magnetic resonance imaging revealed demyelinating patterns in the central portion of the pons and both thalami. He showed severe extrapyramidal symptoms with truncal swaying and postural instability that resulted in severe gait disturbance. Postural instability showed little improvement after conventional physical therapy, but his symptoms markedly improved after five days of dopamine administration. Cessation of dopamine agents was attempted two times, but postural instability and gait disturbance recurred. Therefore, medication was continued for one year. The patient showed stable gait and no further deterioration of postural instability during dopamine therapy.
MeSH Terms
Figure
Reference
-
1. Martin RJ. Central pontine and extrapontine myelinolysis: the osmotic demyelination syndromes. J Neurol Neurosurg Psychiatry. 2004; 75:Suppl 3. iii22–iii28.
Article2. Brown WD. Osmotic demyelination disorders: central pontine and extrapontine myelinolysis. Curr Opin Neurol. 2000; 13:691–697.
Article3. An JY, Park SK, Han SR, Song IU. Central pontine and extrapontinemyelinolysis that developed during alcohol withdrawal, without hyponatremia, in a chronic alcoholic. Intern Med. 2010; 49:615–618.4. Nasrallah HA, Brecher M, Paulsson B. Placebo-level incidence of extrapyramidal symptoms (EPS) with quetiapine in controlled studies of patients with bipolar mania. Bipolar Disord. 2006; 8:467–474.
Article5. Gocht A, Colmant HJ. Central pontine and extrapontine myelinolysis: a report of 58 cases. Clin Neuropathol. 1987; 6:262–270.6. Kleinschmidt-Demasters BK, Rojiani AM, Filley CM. Central and extrapontine myelinolysis: then...and now. J Neuropathol Exp Neurol. 2006; 65:1–11.7. Abbott R, Silber E, Felber J, Ekpo E. Osmotic demyelination syndrome. BMJ. 2005; 331:829–830.
Article8. Sadeh M, Goldhammer Y. Extrapyramidal syndrome responsive to dopaminergic treatment following recovery from central pontine myelinolysis. Eur Neurol. 1993; 33:48–50.
Article9. Kim JS, Lee KS, Han SR, Chung YA. Decreased striatal dopamine transporter binding in a patient with extrapontine myelinolysis. Mov Disord. 2003; 18(3):342–345.
Article10. Blumenfeld Hal. Neuroanatomy through clinical cases. 2nd ed. Sunderland: Sinauer;2010. p. 748–750.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Subacute Onset Choreoathetosis as Sequelae of Central Pontine and Extrapontine Myelinolysis
- A case of central pontine and extrapontine myelinolysis with early hypermetabolism on 18FDG-PET scan
- Neuropsychological Findings of Extrapontine Myelinolysis without Central Pontine Myelinolysis: Initial and Follow-up Evaluation
- Central Pontine and Extrapontine Myelinolysis in a Patient with Traumatic Brain Injury Following Not Rapid Correction of Hyponatremia: A Case Report
- Central Pontine and EXtrapontine Myelinolysis