J Korean Med Sci.
2014 Jun;29(6):793-797. 10.3346/jkms.2014.29.6.793.
The Effect of Body Mass Index on Survival in Advanced Epithelial Ovarian Cancer
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Korea University College of Medicine, Seoul, Korea.
- 2Department of Obstetrics and Gynecology, Kyung Hee University Hospital at Gangdong, Seoul, Korea.
- 3Department of Obstetrics and Gynecology, Gachon University Gil Medical Center, Incheon, Korea.
- 4Department of Gynecologic Oncology, College of Medicine, CHA University, Seongnam, Korea. callen1013@gmail.com
- KMID: 1796941
- DOI: http://doi.org/10.3346/jkms.2014.29.6.793
Abstract
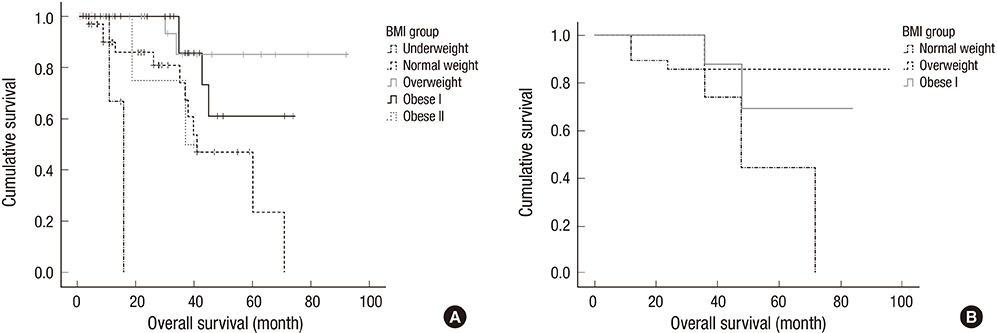
- Controversy remains regarding the effect of obesity on the survival of patients with ovarian cancer in Asia. This study examined the impact of obesity on the survival outcomes in advanced epithelial ovarian cancer (EOC) using Asian body mass index (BMI) criteria. The medical records of patients undergoing surgery for advanced (stage III and IV) EOC were reviewed. Statistical analyses included ANOVA, chi-square test, Kaplan-Meier survival and Cox regression analysis. Among all 236 patients, there were no differences in overall survival according to BMI except in underweight patients. In a multivariate Cox analysis, surgical optimality and underweight status were independent and significant prognostic factors for survival (HR, 2.302; 95% CI, 1.326-3.995; P=0.003 and HR, 8.622; 95% CI, 1.871-39.737; P = 0.006, respectively). In the subgroup of serous histology and optimal surgery, overweight and obese I patients showed better survival than normal weight patients (P = 0.012). We found that underweight BMI and surgical optimality are independent risk factors for the survival of patients with advanced ovarian cancer. High BMI groups (overweight, obese I and II) are not associated with the survival of advanced EOC patient. However, in the subgroup of EOC patients with serous histology and after optimal operation, overweight and obese I group patients show better survival than the normal weight group patients.
Keyword
MeSH Terms
Figure
Reference
-
1. Siegel R, Naishadham D, Jemal A. Cancer statistics, 2013. CA Cancer J Clin. 2013; 63:11–30.2. Jung KW, Won YJ, Kong HJ, Oh CM, Seo HG, Lee JS. Cancer statistics in Korea: incidence, mortality, survival and prevalence in 2010. Cancer Res Treat. 2013; 45:1–14.3. Howlader N, Noone AM, Krapcho M, Neyman N, Aminou R, Waldron W, Altekruse SF, Kosary CL, Ruhl J, Tatalovich Z, et al. Previous version: SEER Cancer Statistics review, 1975-2009 (vintage 2009 populations). accessed on 1 March 2013. Available at http://seer.cancer.gov/archive/csr/1975_2009_pops09.4. Ballard-Barbash R, Swanson CA. Body weight: estimation of risk for breast and endometrial cancers. Am J Clin Nutr. 1996; 63:437S–441S.5. Canchola AJ, Chang ET, Bernstein L, Largent JA, Reynolds P, Deapen D, Henderson KD, Ursin G, Horn-Ross PL. Body size and the risk of ovarian cancer by hormone therapy use in the California Teachers Study cohort. Cancer Causes Control. 2010; 21:2241–2248.6. Sharma D, Wang J, Fu PP, Sharma S, Nagalingam A, Mells J, Handy J, Page AJ, Cohen C, Anania FA, et al. Adiponectin antagonizes the oncogenic actions of leptin in hepatocellular carcinogenesis. Hepatology. 2010; 52:1713–1722.7. Misra A, Chowbey P, Makkar BM, Vikram NK, Wasir JS, Chadha D, Joshi SR, Sadikot S, Gupta R, Gulati S, et al. Consensus statement for diagnosis of obesity, abdominal obesity and the metabolic syndrome for Asian Indians and recommendations for physical activity, medical and surgical management. J Assoc Physicians India. 2009; 57:163–170.8. Shiwaku K, Anuurad E, Enkhmaa B, Nogi A, Kitajima K, Shimono K, Yamane Y, Oyunsuren T. Overweight Japanese with body mass indexes of 23.0-24.9 have higher risks for obesity-associated disorders: a comparison of Japanese and Mongolians. Int J Obes Relat Metab Disord. 2004; 28:152–158.9. World Health Organization. International Association for the Study of Obesity. International Obesity Task Force. The Asia-Pacific perspective: redefining obesity and its treatment. Sydney: Health Communications Australia;2000.10. Pavelka JC, Brown RS, Karlan BY, Cass I, Leuchter RS, Lagasse LD, Li AJ. Effect of obesity on survival in epithelial ovarian cancer. Cancer. 2006; 107:1520–1524.11. Yang L, Klint A, Lambe M, Bellocco R, Riman T, Bergfeldt K, Persson I, Weiderpass E. Predictors of ovarian cancer survival: a population-based prospective study in Sweden. Int J Cancer. 2008; 123:672–679.12. Matthews KS, Straughn JM Jr, Kemper MK, Hoskins KE, Wang W, Rocconi RP. The effect of obesity on survival in patients with ovarian cancer. Gynecol Oncol. 2009; 112:389–393.13. Skírnisdóttir I, Sorbe B. Body mass index as a prognostic factor in epithelial ovarian cancer and correlation with clinico-pathological factors. Acta Obstet Gynecol Scand. 2010; 89:101–107.14. Barakat RR, Berchuck A, Markman M, Randall ME. Principles and practice of gynecologic oncology. 6th ed. Philadelphia: Lippincott Williams & Wilkins;2013.15. World Health Organization. Obesity: preventing and managing the global epidemic. Geneva: World Health Organization;2000.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Recurrent Early-stage Epithelial Ovarian Cancer Presenting as Bone Metastasis
- An overview of the current debate between using minimally invasive surgery versus laparotomy for interval cytoreductive surgery in epithelial ovarian cancer
- The Prognostic Significance of Serum CA 125 Levels in Patients with Advanced Serous Epithelial Ovarian Cancer
- Advanced ovarian cancer: what should be the standard of care?
- Maximal cytoreductive effort in epithelial ovarian cancer surgery