J Korean Med Sci.
2014 Jan;29(1):53-60. 10.3346/jkms.2014.29.1.53.
Intestinal Diffuse Large B-Cell Lymphoma: An Evaluation of Different Staging Systems
- Affiliations
-
- 1Department of Pathology, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea. jrhuh@amc.seoul.kr
- 2Department of Oncology, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea.
- KMID: 1796915
- DOI: http://doi.org/10.3346/jkms.2014.29.1.53
Abstract
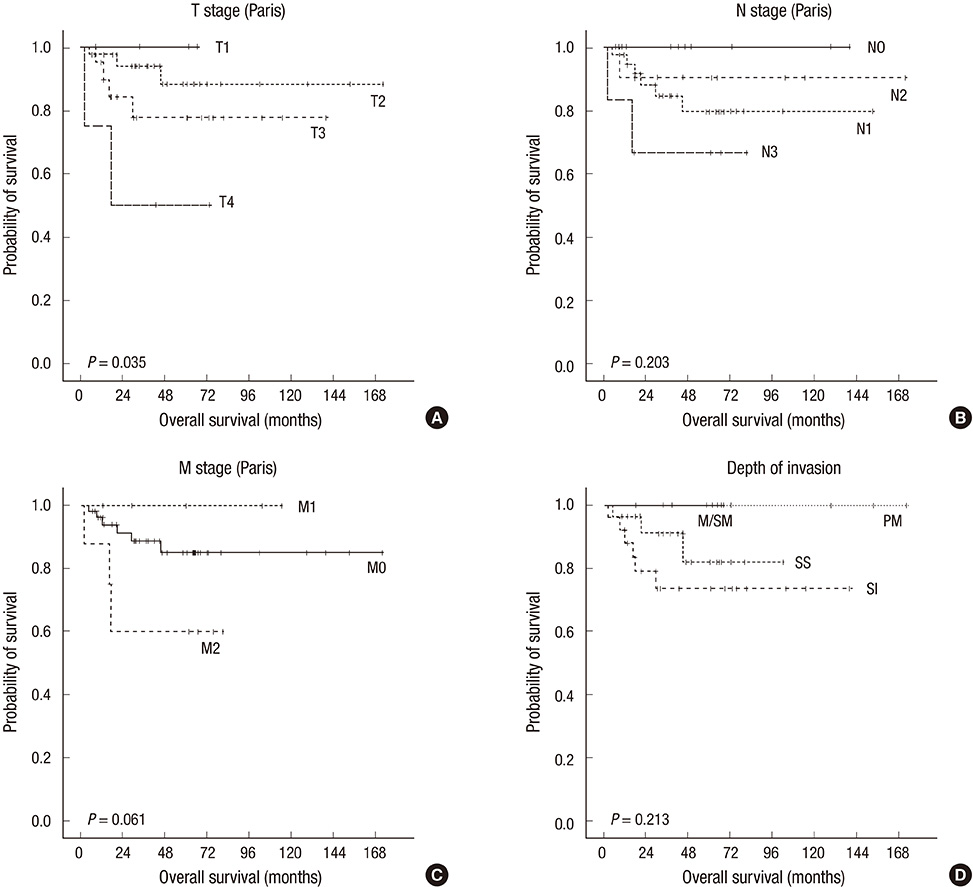
- The gastrointestinal tract is the most common primary extranodal site for diffuse large B-cell lymphoma (DLBCL). However, there is no consensus on the most appropriate staging system for intestinal DLBCL. We evaluated the utility of the modified Ann Arbor system, the Lugano system, and the Paris staging system (a modification of the Tumor, Node, Metastases [TNM] staging for epithelial tumors) in 66 cases of resected intestinal DLBCL. The cases were treated with surgery, plus either cyclophosphamide, doxorubicin, vincristine, and prednisolone (CHOP) chemotherapy alone (n=26) or with the addition of rituximab immunotherapy (n=40). Median follow-up time was 40.4 months (range, 2.1-171.6 months). Fifty-six patients (84.8%) achieved complete remission. The overall 5-yr survival rate was 86.4% (57/66). Of the stage categories defined for each staging system, only the T stage of the Paris classification showed prognostic significance for overall survival by univariate analysis. However, none of the stage parameters was significantly correlated with patient survival on multivariate analysis. In conclusion, the results suggest that the T stage of the Paris classification system may be a prognostic indicator in intestinal DLBCL. The results also imply that in surgically resected intestinal DLBCL, the addition of rituximab to the CHOP regimen does not confer significant survival advantage.
Keyword
MeSH Terms
-
Adolescent
Adult
Aged
Antibodies, Monoclonal, Murine-Derived/therapeutic use
Antineoplastic Combined Chemotherapy Protocols/therapeutic use
Cyclophosphamide/therapeutic use
Doxorubicin/therapeutic use
Female
Humans
Immunologic Factors/therapeutic use
Intestinal Neoplasms/*classification/drug therapy/mortality/surgery
Lymphoma, Large B-Cell, Diffuse/*classification/drug therapy/mortality/surgery
Male
Middle Aged
Neoplasm Staging/*methods
Prednisone/therapeutic use
Retrospective Studies
Survival
Survival Rate
Treatment Outcome
Vincristine/therapeutic use
Young Adult
Antibodies, Monoclonal, Murine-Derived
Immunologic Factors
Vincristine
Doxorubicin
Cyclophosphamide
Prednisone
Figure
Reference
-
1. Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, Thiele J, Vzrdiman JW. WHO classification of tumours of haematopoietic and lymphoid tissues. 4th ed. Lyon: IARC;2008.2. Gobbi PG, Ghirardelli ML, Cavalli C, Baldini L, Broglia C, Clò V, Bertè R, Ilariucci F, Carotenuto M, Piccinini L, et al. The role of surgery in the treatment of gastrointestinal lymphomas other than low-grade MALT lymphomas. Haematologica. 2000; 85:372–380.3. Ghimire P, Wu GY, Zhu L. Primary gastrointestinal lymphoma. World J Gastroenterol. 2011; 17:697–707.4. Beaton C, Davies M, Beynon J. The management of primary small bowel and colon lymphoma: a review. Int J Colorectal Dis. 2012; 27:555–563.5. Ruskone-Fourmestraux A, Delmer A, Hennequin C. Gastro-intestinal lymphomas. Gastroenterol Clin Biol. 2006; 30:2S81–2S90.6. Pfreundschuh M, Trümper L, Osterborg A, Pettengell R, Trneny M, Imrie K, Ma D, Gill D, Walewski J, Zinzani PL, et al. CHOP-like chemotherapy plus rituximab versus CHOP-like chemotherapy alone in young patients with good-prognosis diffuse large-B-cell lymphoma: a randomised controlled trial by the MabThera International Trial (MInT) Group. Lancet Oncol. 2006; 7:379–391.7. Daum S, Ullrich R, Heise W, Dederke B, Foss HD, Stein H, Thiel E, Zeitz M, Riecken EO. Intestinal non-Hodgkin's lymphoma: a multicenter prospective clinical study from the German Study Group on Intestinal non-Hodgkin's Lymphoma. J Clin Oncol. 2003; 21:2740–2746.8. Lee J, Kim WS, Kim K, Ahn JS, Jung CW, Lim HY, Kang WK, Park K, Ko YH, Kim YH, et al. Prospective clinical study of surgical resection followed by CHOP in localized intestinal diffuse large B cell lymphoma. Leuk Res. 2007; 31:359–364.9. Kim SJ, Kang HJ, Kim JS, Oh SY, Choi CW, Lee SI, Won JH, Kim MK, Kwon JH, Mun YC, et al. Comparison of treatment strategies for patients with intestinal diffuse large B-cell lymphoma: surgical resection followed by chemotherapy versus chemotherapy alone. Blood. 2011; 117:1958–1965.10. Musshoff K. Clinical staging classification of non-Hodgkin's lymphomas (author's transl). Strahlentherapie. 1977; 153:218–221.11. Radaszkiewicz T, Dragosics B, Bauer P. Gastrointestinal malignant lymphomas of the mucosa-associated lymphoid tissue: factors relevant to prognosis. Gastroenterology. 1992; 102:1628–1638.12. Rohatiner A, d'Amore F, Coiffier B, Crowther D, Gospodarowicz M, Isaacson P, Lister TA, Norton A, Salem P, Shipp M, et al. Report on a workshop convened to discuss the pathological and staging classifications of gastrointestinal tract lymphoma. Ann Oncol. 1994; 5:397–400.13. Ruskoné-Fourmestraux A, Dragosics B, Morgner A, Wotherspoon A, De Jong D. Paris staging system for primary gastrointestinal lymphomas. Gut. 2003; 52:912–913.14. Lewin KJ, Ranchod M, Dorfman RF. Lymphomas of the gastrointestinal tract: a study of 117 cases presenting with gastrointestinal disease. Cancer. 1978; 42:693–707.15. Koch P, del Valle F, Berdel WE, Willich NA, Reers B, Hiddemann W, Grothaus-Pinke B, Reinartz G, Brockmann J, Temmesfeld A, et al. Primary gastrointestinal non-Hodgkin's lymphoma: I. anatomic and histologic distribution, clinical features, and survival data of 371 patients registered in the German Multicenter Study GIT NHL 01/92. J Clin Oncol. 2001; 19:3861–3873.16. Chuang SS, Ye H, Du MQ, Lu CL, Dogan A, Hsieh PP, Huang WT, Jung YC. Histopathology and immunohistochemistry in distinguishing Burkitt lymphoma from diffuse large B-cell lymphoma with very high proliferation index and with or without a starry-sky pattern: a comparative study with EBER and FISH. Am J Clin Pathol. 2007; 128:558–564.17. Bellan C, Stefano L, Giulia de F, Rogena EA, Lorenzo L. Burkitt lymphoma versus diffuse large B-cell lymphoma: a practical approach. Hematol Oncol. 2010; 28:53–56.18. Hans CP, Weisenburger DD, Greiner TC, Gascoyne RD, Delabie J, Ott G, Müller-Hermelink HK, Campo E, Braziel RM, Jaffe ES, et al. Confirmation of the molecular classification of diffuse large B-cell lymphoma by immunohistochemistry using a tissue microarray. Blood. 2004; 103:275–282.19. Greene FL, Page DL, Fleming ID. AJCC cancer staging manual: TNM classification of malignant tumors. 6th ed. New York: Springer-Verlag;2002.20. Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A. AJCC cancer staging handbook. 7th ed. New York: Springer;2010.21. Miller AB, Hoogstraten B, Staquet M, Winkler A. Reporting results of cancer treatment. Cancer. 1981; 47:207–214.22. Kako S, Oshima K, Sato M, Terasako K, Okuda S, Nakasone H, Yamazaki R, Tanaka Y, Tanihara A, Kawamura Y, et al. Clinical outcome in patients with small-intestinal non-Hodgkin lymphoma. Leuk Lymphoma. 2009; 50:1618–1624.23. Ferrucci PF, Zucca E. Primary gastric lymphoma pathogenesis and treatment: what has changed over the past 10 years? Br J Haematol. 2007; 136:521–538.24. Psyrri A, Papageorgiou S, Economopoulos T. Primary extranodal lymphomas of stomach: clinical presentation, diagnostic pitfalls and management. Ann Oncol. 2008; 19:1992–1999.25. Nakamura S, Matsumoto T, Iida M, Yao T, Tsuneyoshi M. Primary gastrointestinal lymphoma in Japan: a clinicopathologic analysis of 455 patients with special reference to its time trends. Cancer. 2003; 97:2462–2473.26. Shimodaira M, Tsukamoto Y, Niwa Y, Goto H, Hase S, Hayakawa T, Nagasaka T. A proposed staging system for primary gastric lymphoma. Cancer. 1994; 73:2709–2715.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Primary Cutaneous Diffuse Large B-cell Lymphoma
- Relapse of Ocular Lymphoma following Primary Testicular Diffuse Large B-cell Lymphoma
- Gastrointestinal Lymphoma
- A Case of Diffuse Large B Cell Lymphoma Transformed from a Duodenal Low Grade MALT Lymphoma
- A Case of Epstein-Barr Virus-Positive Diffuse Large B-Cell Lymphoma Occurring in Thyroid Gland