J Korean Med Sci.
2010 Jul;25(7):1077-1079. 10.3346/jkms.2010.25.7.1077.
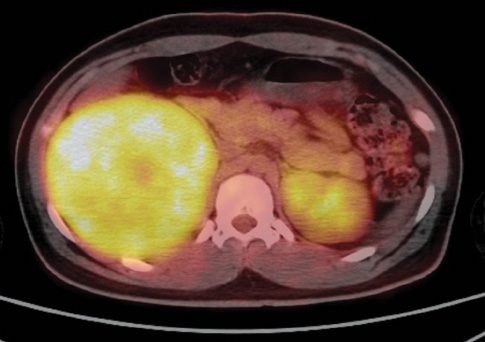
Virilizing Adrenocortical Oncocytoma in a Child: A Case Report
- Affiliations
-
- 1Department of Pediatrics, Hanyang University College of Medicine, Seoul, Korea. cord@hanyang.ac.kr
- 2Department of Pharmacology, Hanyang University College of Medicine, Seoul, Korea.
- KMID: 1792960
- DOI: http://doi.org/10.3346/jkms.2010.25.7.1077
Abstract
- Functioning adrenocortical oncocytomas are extremely rare and most reported patients are 40-60 yr of age. To our knowledge, only 2 cases of functioning adrenocortical oncocytomas have been reported in childhood. We report a case of functioning adrenocortical oncocytoma in a 14-yr-old female child presenting with virilization. She presented with deepening of the voice and excessive hair growth, and elevation of plasma testosterone and dehydroepiandrosterone sulfate. She had an adrenalectomy. The completely resected tumor composed predominantly of oncocytes without atypical mitosis and necrosis. A discussion of this case and a review of the literature on this entity are presented.
Keyword
MeSH Terms
Figure
Reference
-
1. Yildiz BO. Diagnosis of hyperandrogenism: clinical criteria. Best Pract Res Clin Endocrinol Metab. 2006. 20:167–176.
Article2. Chundler RM, Kay R. Adrenocortical carcinoma in children. Urol Clin North Am. 1989. 16:469–479.3. Michalkiewicz E, Sandrini R, Figueiredo B, Miranda EC, Caran E, Oliveira-Filho AG, Marques R, Pianovski MA, Lacerda L, Cristofani LM, Jenkins J, Rodriguez-Galindo C, Ribeiro RC. Clinical and outcome characteristics of children with adrenocortical tumors: A report from the international pediatric adrenocortical tumor registry. J Clin Oncol. 2004. 22:838–845.
Article4. Chen TS, McNally M, Hulbert W, Di Sant'Agnese PA, Huang J. Renal oncocytosis presenting in childhood. Int J Surg Pathol. 2003. 11:325–329.5. Tahar GT, Nejib KN, Sadok SS, Rachid LM. Adrenocortical oncocytoma: a case report and review of literature. J Pediatr Surg. 2008. 43:E1–E3.
Article6. Bisceglia M, Ludovico O, Di Mattia A, Ben-Dor D, Sandbank J, Pasquinelli G, Lau SK, Weiss LM. Adrenocortical oncocytic tumors: report of 10 cases and review of the literature. Int J Surg Pathol. 2004. 12:231–243.
Article7. Juliano JJ, Cody RL, Suh JH. Metastatic adrenocortical oncocytoma: a case report. Urol Oncol. 2008. 26:198–201.
Article