Korean J Gastroenterol.
2011 Jul;58(1):53-57. 10.4166/kjg.2011.58.1.53.
Steroid Responsive Pancreatic Mass-Forming Type 2 Autoimmune Pancreatitis
- Affiliations
-
- 1Department of Internal Medicine, The Catholic University of Korea College of Medicine, Seoul, Korea. wwjjaang@catholic.ac.kr
- 2Department of Pathology, The Catholic University of Korea College of Medicine, Seoul, Korea.
- KMID: 1792816
- DOI: http://doi.org/10.4166/kjg.2011.58.1.53
Abstract
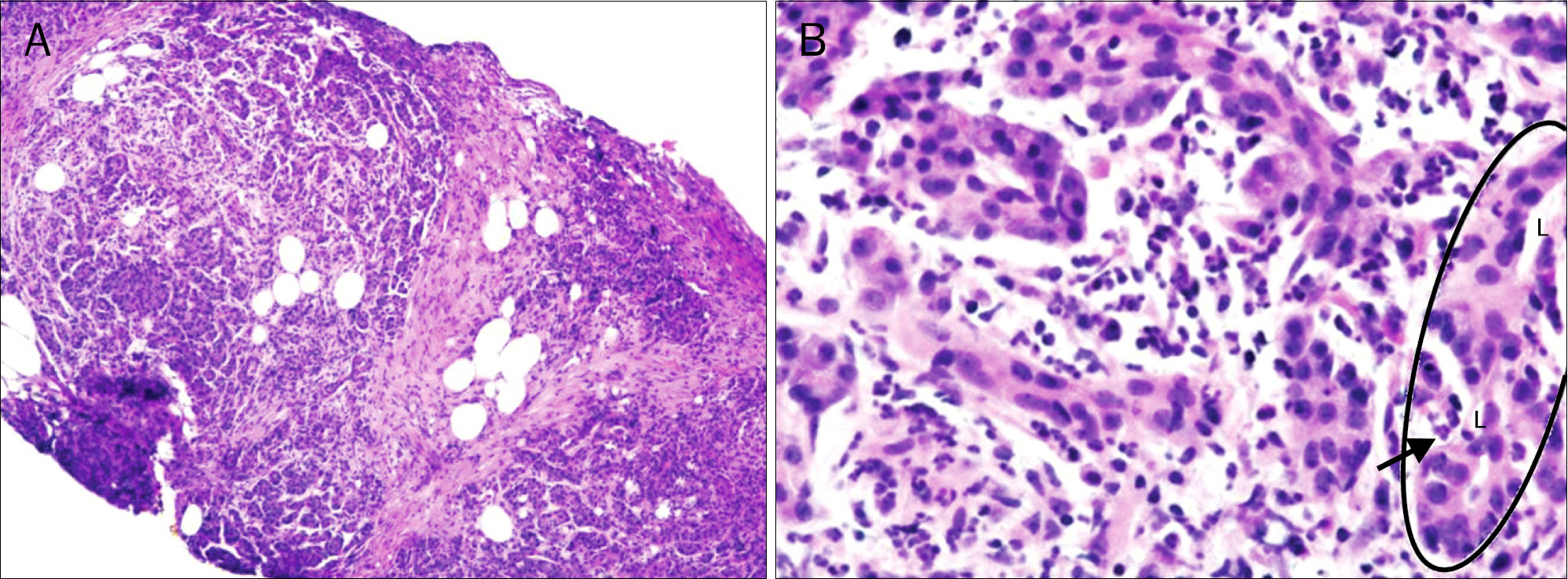
- Autoimmune pancreatitis (AIP) has two distinct subsets. Type 1 AIP or lymphoplasmacytic sclerosing pancreatitis is systemic disease with the elevation in serum levels of the IgG4. Type 2 AIP, also called duct-centric pancreatitis, features granulocyte epithelial lesions with duct obstruction in the pancreas without systemic involvement. Here, we report a case of type 2 AIP diagnosed by pathology, which is the first report in Korea. The case is a 56-year-old woman who presented with anorexia and vomiting. Computed tomography revealed mass-like lesion in the pancreatic head and the compression of the distal common bile duct and the head portion of the main pancreatic duct. Serum levels of the IgG4 were normal. Histologic examination revealed a dense neutrophil infiltration in the pancreatic parenchyme associated with extensive fibrosis, thereby confirming the diagnosis of type 2 AIP. The abnormalities in the clinical, laboratory, and radiological findings improved after oral steroid treatment.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Sarles H, Sarles JC, Muratore R, Guien C. Chronic inflammatory sclerosis of the pancreas–an autonomous pancreatic disease? Am J Dig Dis. 1961; 6:688–698.
Article2. Yoshida K, Toki F, Takeuchi T, Watanabe S, Shiratori K, Hayashi N. Chronic pancreatitis caused by an autoimmune abnormality. Proposal of the concept of autoimmune pancreatitis. Dig Dis Sci. 1995; 40:1561–1568.3. Park DH, Kim MH, Chari ST. Recent advances in autoimmune pancreatitis. Gut. 2009; 58:1680–1689.
Article4. Okazaki K, Chiba T. Autoimmune related pancreatitis. Gut. 2002; 51:1–4.
Article5. Hamano H, Kawa S, Horiuchi A, et al. High serum IgG4 concentrations in patients with sclerosing pancreatitis. N Engl J Med. 2001; 344:732–738.
Article6. Ectors N, Maillet B, Aerts R, et al. Nonalcoholic duct destructive chronic pancreatitis. Gut. 1997; 41:263–268.
Article7. Notohara K, Burgart LJ, Yadav D, Chari S, Smyrk TC. Idiopathic chronic pancreatitis with periductal lymphoplasmacytic infiltration: clinicopathologic features of 35 cases. Am J Surg Pathol. 2003; 27:1119–1127.8. Klöppel G. Chronic pancreatitis, pseudotumors and other tumor-like lesions. Mod Pathol. 2007; 20(Suppl 1):S113–S131.
Article9. Zhang L, Notohara K, Levy MJ, Chari ST, Smyrk TC. IgG4-positive plasma cell infiltration in the diagnosis of autoimmune pancreatitis. Mod Pathol. 2007; 20:23–28.
Article10. Kim KP, Kim M, Lee YJ, et al. Clinical characteristics of 17 cases of autoimmune chronic pancreatitis. Korean J Gastroenterol. 2004; 43:112–119.11. Kim JY, Chang HS, Kim MH, et al. A case of autoimmune chronic pancreatitis improved with oral steroid therapy. Korean J Gastroenterol. 2002; 39:304–308.12. Park SJ, Kim MH, Moon SH, et al. Clinical characteristics, recurrence features, and treatment outcomes of 55 patients with autoimmune pancreatitis. Korean J Gastroenterol. 2008; 52:230–246.13. Lee JY, Park DH, Park SH, et al. Two cases of seronegative, main pancreatic ductal narrowing, chronic pancreatitis that were responsive to short-term steroid treatment. Korean J Med. 2007; 72(Suppl 2):S103–S109.14. Zamboni G, Lüttges J, Capelli P, et al. Histopathological features of diagnostic and clinical relevance in autoimmune pancreatitis: a study on 53 resection specimens and 9 biopsy specimens. Virchows Arch. 2004; 445:552–563.
Article15. Klöppel G, Lüttges J, Löhr M, Zamboni G, Longnecker D. Autoimmune pancreatitis: pathological, clinical, and immuno-logical features. Pancreas. 2003; 27:14–19.
Article16. Yadav D, Notahara K, Smyrk TC, et al. Idiopathic tumefactive chronic pancreatitis: clinical profile, histology, and natural history after resection. Clin Gastroenterol Hepatol. 2003; 1:129–135.
Article17. Kamisawa T, Egawa N, Nakajima H. Autoimmune pancreatitis is a systemic autoimmune disease. Am J Gastroenterol. 2003; 98:2811–2812.
Article18. Takahashi N, Kawashima A, Fletcher JG, Chari ST. Renal involvement in patients with autoimmune pancreatitis: CT and MR imaging findings. Radiology. 2007; 242:791–801.
Article19. Okazaki K, Kawa S, Kamisawa T, et al. Japanese clinical guidelines for autoimmune pancreatitis. Pancreas. 2009; 38:849–866.20. Detlefsen S, Mohr Drewes A, Vyberg M, Klöppel G. Diagnosis of autoimmune pancreatitis by core needle biopsy: application of six microscopic criteria. Virchows Arch. 2009; 454:531–539.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Mass-forming focal-type autoimmune pancreatitis difficult to differentiate from pancreatic cancer
- Differentiation of Mass-Forming Autoimmune Pancreatitis from Pancreatic Cancer Using A 2-Week Steroid Trial
- Localized Mass-Forming Autoimmune Pancreatitis Associated with an Intraductal Papillary Mucinous Neoplasm Mimicking Pancreatic Cancer
- Autoimmune Pancreatitis Featuring a Pseudocyst Requiring Drainage despite Steroid Therapy
- Treatment and Relapse of Autoimmune Pancreatitis