Korean J Gastroenterol.
2010 Apr;55(4):217-224. 10.4166/kjg.2010.55.4.217.
Diagnosis and Management of Esophageal Chest Pain
- Affiliations
-
- 1Department of Internal Medicine, Soonchunhyang University School of Medicine, Bucheon, Korea. sjhong@schbc.ac.kr
- KMID: 1792771
- DOI: http://doi.org/10.4166/kjg.2010.55.4.217
Abstract
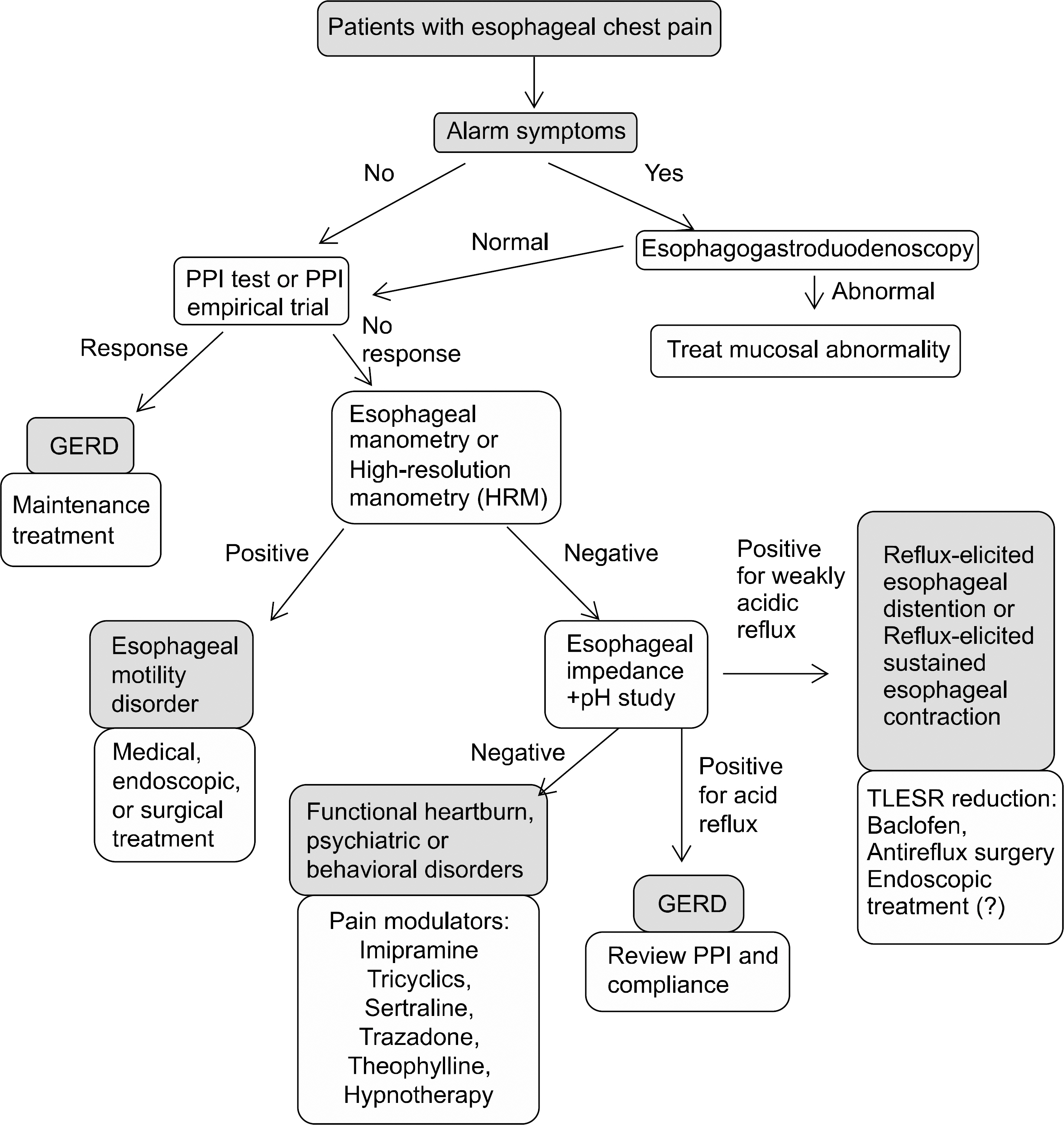
- Esophageal pain that manifests as heartburn or chest pain, is a prevalent problem. Esophageal chest pain is most often caused by gastroesophageal reflux disease (GERD), but can also result from inflammatory processes, infections involving the esophagus, and contractions of the esophageal muscle. The mechanisms and pathways of esophageal chest pain are poorly understood. Vagal and spinal afferent pathways carry sensory information from the esophagus. Recently, esophageal hypersensitivity is identified as an important factor in the development of esophageal pain. A number of techniques are available to evaluate esophageal chest pain such as endoscopy and/or proton-pump inhibitor trial, esophageal manometry, a combined impedance-pH study, and esophageal ultrasound imaging. Proton pump inhibitors (PPIs) have the huge success in the treatment of GERD. Other drugs such as imipramine, trazadone, sertraline, tricyclics, and theophylline have been introduced for the control of esophageal chest pain in partial responders to PPI and the patients with esophageal hypersensitivity. Novel drugs which act on different targets are anticipated to treat esophageal pain in the future.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Efficacy of Proton Pump Inhibitor in Patients with Non-cardiac Chest
Sun Hyung Kang
Korean J Gastroenterol. 2020;75(6):311-313. doi: 10.4166/kjg.2020.75.6.311.
Reference
-
1. Fass R, Dickman R. Non-cardiac chest pain: an update. Neurogastroenterol Motil. 2006; 18:408–417.
Article2. Kim JH, Rhee PL, Park EH, Son HJ, Kim JJ, Rhee JC. Clinical usefulness of subgrouping of patients with non-cardiac chest pain according to characteristic symptoms in Korea. J Gastroenterol Hepatol. 2007; 22:320–325.
Article3. Kim JH, Sinn DH, Son HJ, Kim JJ, Rhee JC, Rhee PL. Comparison of one-week and two-week empirical trial with a high-dose rabeprazole in non-cardiac chest pain patients. J Gastroenterol Hepatol. 2009; 24:1504–1509.
Article4. Balaban DH, Yamamoto Y, Liu J, et al. Sustained esophageal contraction: a marker of esophageal chest pain identified by intraluminal ultrasonography. Gastroenterology. 1999; 116:29–37.
Article5. Fruergaard P, Launbjerg J, Hesse B, et al. The diagnoses of patients admitted with acute chest pain but without myocardial infarction. Eur Heart J. 1996; 17:1028–1034.
Article6. Martinez SD, Malagon IB, Garewal HS, Fass R. Non-erosive reflux disease (NERD)–acid reflux and symptom patterns. Aliment Pharmacol Ther. 2003; 17:537–545.7. Douglas A Drossman. Rome III: The Functional Gastrointestinal Disorders. 3rd ed.McLean, Va: Degnon Associates, Inc.;2006.8. Fass R, Tougas G. Functional heartburn: the stimulus, the pain and the brain. Gut. 2002; 51:885–892.
Article9. Rodriguez-Stanley S, Robinson M, Earnest DL, Greenwood- Van Meerveld B, Miner PB Jr. Esophageal hypersensitivity may be a major cause of heartburn. Am J Gastroenterol. 1999; 94:628–631.
Article10. Mayer EA. Spinal and supraspinal modulation of visceral sensation. Gut. 2000; 47(suppl 4):iv69–72.
Article11. Tack J, Koek G, Demedts I, Sifrim D, Janssens J. Gastroesophageal reflux disease poorly responsive to single-dose proton pump inhibitors in patients without Barrett's esophagus: acid reflux, bile reflux, or both? Am J Gastroenterol. 2004; 99:981–989.
Article12. Ang D, Sifrim D, Tack J. Mechanisms of heartburn. Nat Clin Pract Gastroenterol Hepatol. 2008; 5:383–392.
Article13. Blackshaw LA, Grundy D. Effects of 5-hydroxytryptamine on discharge of vagal mucosal afferent fibres from the upper gastrointestinal tract of the ferret. J Auton Nerv Syst. 1993; 45:41–50.
Article14. Cervero F. Sensory innervationsof the viscera: peripheral ba-sis of visceral pain. Physiol Rev. 1994; 74:95–138.15. Page AJ, O'Donnell TA, Blackshaw LA. P2X purinoceptor- induced sensitization of ferret vagal mechanoreceptors in oesophageal inflammation. J Physiol. 2000; 523:403–411.16. Sengupta JN, Saha JK, Goyal RK. Differential sensitivity to brakykinin of esophageal distension-sensitive mechanoreceptors in vagal and sympathetic afferents of the opossum. J Neurophysiol. 1992; 68:1053–1067.17. Slattery JA, Page AJ, Dorian DL, Brierley SM, Blackshaw LA. Potentiation of mouse vagal afferent mechanosensitivity by ionotropic and metabotropic glutamate receptors. J Physiol. 2006; 577:295–306.
Article18. Matthews PJ, Aziz Q, Facer P, Davis JB, Thompson DG, Anand P. Increased capsaicin receptor TRPV1 nerve fibres in the inflamed human oesophagus. Eur J Gastroenterol Hepatol. 2004; 16:897–902.
Article19. Bhat YM, Bielefeldt K. Capsaicin receptor (TRPV1) and non-erosive reflux disease. Eur J Gastroeterol Hepatol. 2006; 18:263–270.
Article20. Page AJ, Blackshaw LA. GABA(B) receptors inhibit mechanosensitivity of primary afferent endings. J Neurosci. 1999; 19:8597–8602.21. Partosoedarso ER, Young RL, Blackshaw LA. GABA(B) receptors on vagal afferent pathways: peripheral and central inhibition. Am J Physiol Gastrointest Liver Physiol. 2001; 280:G658–668.
Article22. Page AJ, Slattery JA, Brierley SM, Jacoby AS, Blackshaw LA. Involvement of galanin receptors 1 and 2 in the modulation of mouse vagal afferent mechanosensitivity. J Physiol. 2007; 583:675–684.
Article23. Page AJ, Young RL, Martin CM, et al. Metabotropic glutamate receptors inhibit mechanosensitivity in vagal sensory neurons. Gastroenterology. 2005; 128:402–410.
Article24. Page AJ, O'Donnell TA, Blackshaw LA. Opioid modulation of ferret vagal afferent mechanosensitivity. Am J Physiol Gastrointest Liver Physiol. 2008; 294:G963–970.
Article25. Dray A. Inflammatory mediators of pain. Br J Anaesth. 1995; 75:125–131.
Article26. Armstrong D, Marshall JK, Chiba N, et al. Canadian Consensus Conference on the management of gastroesophageal reflux disease in adults-update 2004. Can J Gastroenterol. 2005; 19:15–35.27. Vakil N, Moayyedi P, Fennerty MB, Talley NJ. Limited value of alarm features in the diagnosis of upper gastrointestinal malignance: systematic review and metaanalysis. Gastroenterology. 2006; 131:390–401.28. Gonsalves N, Policarpio-Nicolas M, Zhang Q, Rao MS, Hirano I. Histopathologic variability and endoscopic correlates in adults with eosinophilic esophagitis. Gastrointest Endosc. 2006; 64:313–319.
Article29. Williams D, Thompson DG, Heggie L, Bancewicz J. Res-ponses of the human esophagus to experimental intraluminal distension. Am J Physiol. 1993; 265:G196–203.
Article30. Balaban DH, Yamamoto Y, Liu J, et al. Sustained esophageal contraction: a marker of esophageal chest pain identified by intraluminal ultrasonography. Gastroenterology. 1999; 116:29–37.
Article31. Fass R, Fennerty MB, Ofman JJ, et al. The clinical and eco-nomic value of a short course of omeprazole in patients with noncardiac chest pain. Gastroenterology. 1998; 115:42–49.
Article32. Balaban D, Yamamoto Y, Liu J, et al. Sustained esophageal contraction: a marker of esophageal chest pain identified by intraluminal ultrasonography. Gastroenterology. 1999; 116:29–37.
Article33. Richter JE, Dalton CB, Bradley LA, Castell DO. Oral nifedipine in the treatment of noncardiac chest pain in patients with nutcracker esophagus. Gastroenterology. 1987; 93:21–28.34. Kikendall JW, Mellow MH. Effect of sublingual nitroglycerin and lon-acting nitrate preparations on esophageal motility. Gastroenterology. 1980; 79:703–706.35. Miller LS, Pullela SV, Parkman HP, et al. Treatment of chest pain in patients with noncardiac, nonreflux, nonachalasia spastic esophageal motor disorders using botulinum toxin injection into the gastroesophageal junction. Am J Gastroenterol. 2002; 97:1640–1646.
Article36. Patti MG, Gorodner MV, Galvani C. Spectrum of esophageal motility disorders: implications for diagnosis and treatment. Arch Surg. 2005; 140:442–448.37. Cannon RO 3rd, Quyyumi AA, Mincemoyer R, et al. Imipramine in patients with chest pain despite normal coronary angiograms. N Engl J Med. 1994; 330:1411–1417.
Article38. Clouse RE, Lustman PJ, Eckert TC, Ferney DM, Griffith LS. Low dose trazadone for symptomatic patients with esophageal contaction abnormalities. A double-blind placebo-controlled trial. Gastroenterology. 1987; 92:1027–1036.39. Varia I, Logue E, O'Conner C, et al. Randomized trial of sertraline in patients with unexplained chest pain of non-cardiac origin. Am Heart J. 2000; 140:367–372.
Article40. Prakash C, Clouse RE. Longterm outcome from tricyclic an-ti-depressant therapy of functional chest pain. Dig Dis Sci. 1999; 44:2373–2379.41. Rao SS, Mudipalli RS, Mujica V, Utech CL, Zhao X, Conklin JL. An open-label trial of theophylline for functional chest pain. Dig Dis Sci. 2002; 47:2763–2768.42. Rao SS, Mudipalli RS, Remes-Troche JM, Utech CL, Zimmerman B. Theophylline improves esophageal chest pain-a randomized, placebo-controlled study. Am J Gastroenterol. 2007; 102:930–938.
Article44. Jones H, Cooper P, Miller V, Brooks N, Whorwell PJ. Treatment of non-cardiac chest pain: a controlled trial of hyp-notherapy. Gut. 2006; 55:1403–1408.
Article43. Remes-Troche JM, Chahal P, Mudipalli R, Rao SS. Adeno-sine modulates oesophageal sensorimotor function in humans. Gut. 2009; 58:1049–1055.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Diagnosis and Management of Functional Chest Pain in the Rome IV Era
- Noncardiac Chest Pain: Epidemiology, Natural Course and Pathogenesis
- Diagnosis of Achalasia
- The Role of High Resolution Manometry in Non-Cardiac Chest Pain
- Esophageal Actinomycosis after Insertion of Esophageal Stent: A Case of Surgical Experience