Korean J Gastroenterol.
2009 Jun;53(6):378-382. 10.4166/kjg.2009.53.6.378.
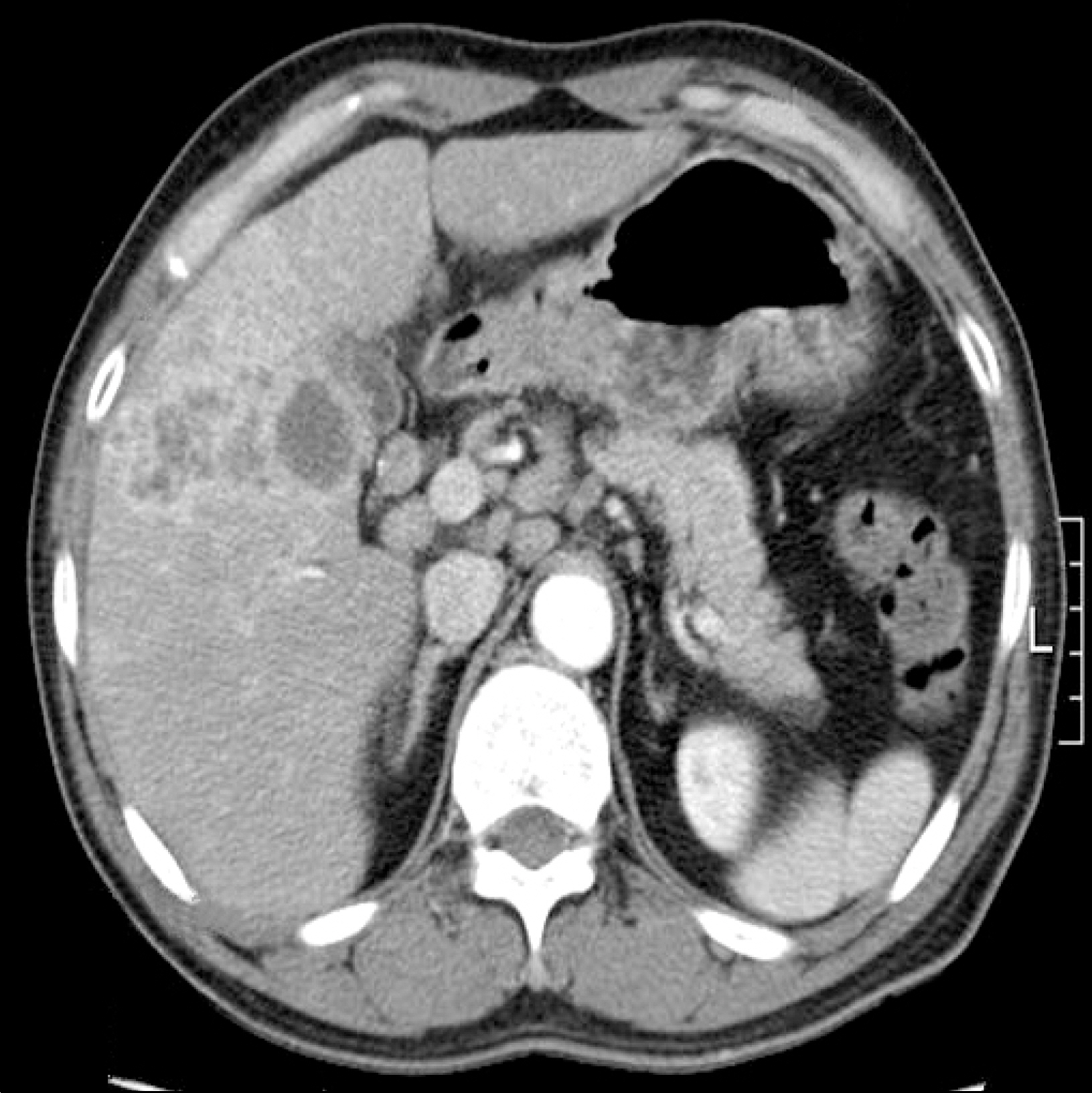
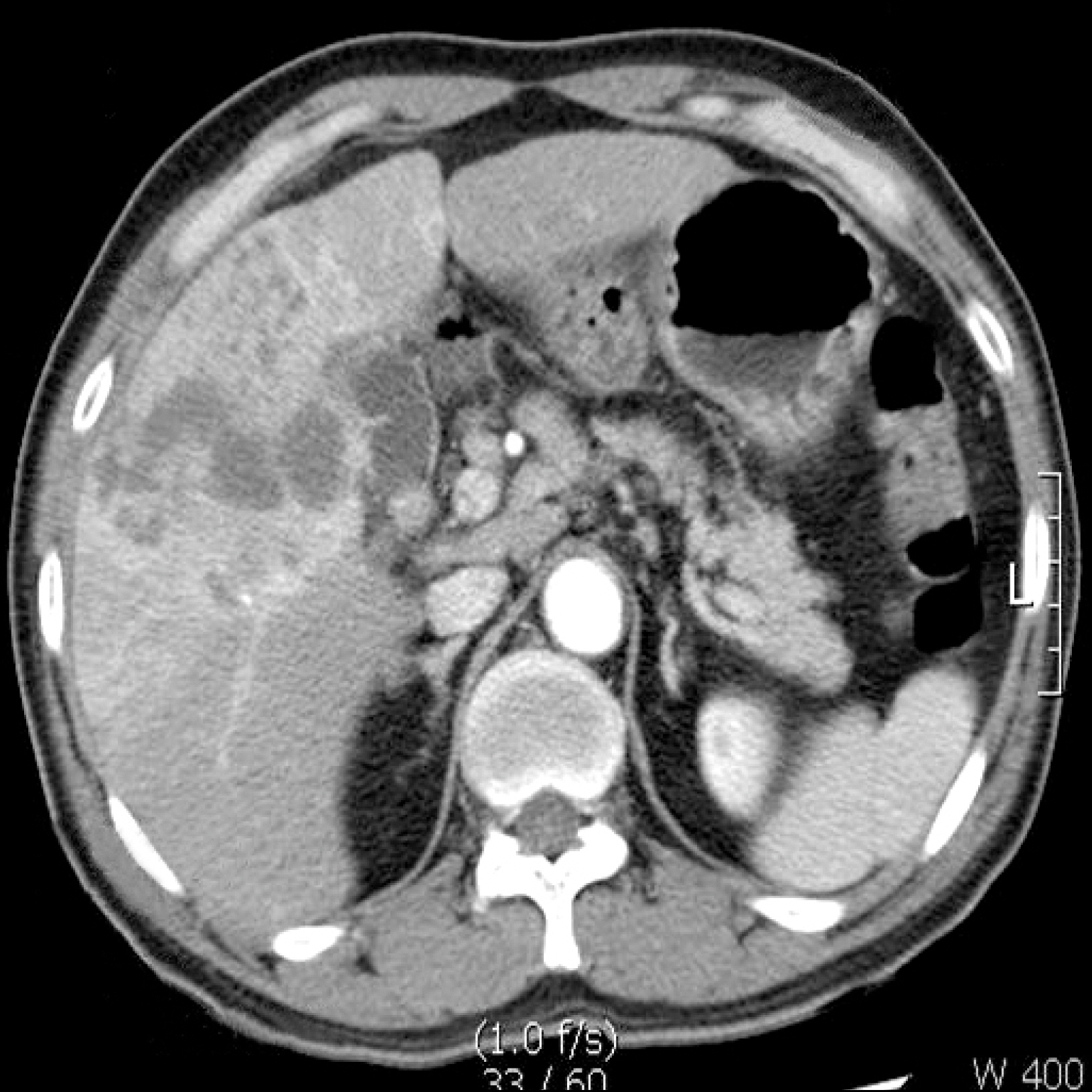
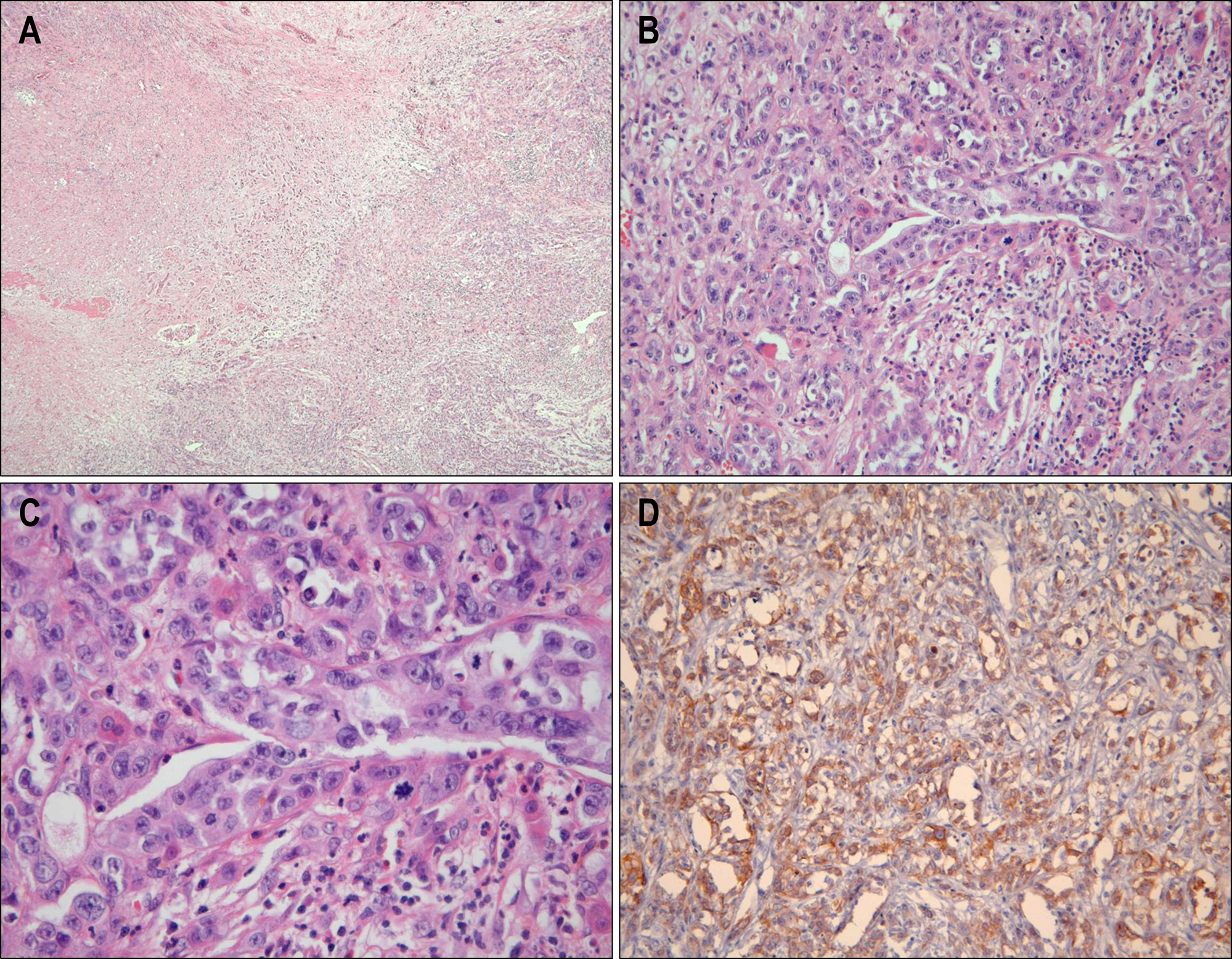
A Case of Hepatocellular Carcinoma Combined with Liver Abscess
- Affiliations
-
- 1Department of Internal Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea. swchoi2253@catholic.ac.kr
- 2Department of Surgery, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- KMID: 1792756
- DOI: http://doi.org/10.4166/kjg.2009.53.6.378
Abstract
- Hepatocellular calcinoma (HCC) is the fifth most common cancer and the third leading cause of cancer-related deaths worldwide. It is important to diagnose HCC exactly before management is attempted. But, the clinical presentations and radiologic findings of liver abscess, HCC, and metastatic tumor to the liver may be quite similar, and procedures such as serum tumor marker assay, computerized tomography, and ultrasonography of the liver cannot make a specific diagnosis. We report a case of HCC successfully diagnosed by surgery which was misconceived as liver abscess and not improved by medical treatment.
Keyword
MeSH Terms
Figure
Reference
-
1. Parikh S, Hyman D. Hepatocellular cancer: a guide for the internist. Am J Med. 2007; 120:194–202.
Article2. Yeh TS, Jan YY, Jeng LB, Chen TC, Hwang TL, Chen MF. Hepatocellular carcinoma presenting as pyogenic liver abscess: characteristics, diagnosis, and management. Clin Infect Dis. 1998; 26:1224–1226.
Article3. Kew MC, Geddes EW. Hepatocellular carcinoma in rural southern African blacks. Medicine (Baltimore). 1982; 61:98–108.
Article4. Lee JW, Lee JS, Kim EK, Kim SN, Choo SY. A clinical study of primary hepatoma. Korean J Gastroenterol. 1990; 22:583–588.5. Choi TY, Kim JP, Kim BH, et al. Two case of primary hepatocellular carcinoma presenting with high fever and leukocytosis mimicking liver abscess. Korean J Gastroenterol. 1993; 25:573–580.6. Berman C. The primary cancer of the liver Bull N Y Acad Med. 1959; 35:275–292.7. Okuda K, Kondo Y, Nakano M, et al. Hepatocellular carcinoma presenting with pyrexia and leukocytosis: report of five cases. Hepatology. 1991; 13:695–700.
Article8. Klotz SA, Penn RL. Clinical differentiation of abscess from neoplasm in newly diagnosed space-occupying lesions of the liver. South Med J. 1987; 80:1537–1541.9. Sung YJ, Yu SE, Park SM, et al. Hepatocellular carcinoma incidentally discovered by liver abscess associated with CBD stone and cholangitis. Korean J Hepatol. 1999; 5:253–258.10. Chen MF, Jan YY, Wang CS, et al. A reappraisal of cholangiocarcinoma in patient with hepatolithiasis. Cancer. 1993; 71:2461–2465.
Article11. Chou FF, Sheen-Chen SM, Chen YS, Chen MC, Chen FC, Tai DI. Prognostic factors for pyogenic abscess of the liver. J Am Coll Surg. 1994; 179:727–732.12. Branum GD, Tyson GS, Branum MA, Meyers WC. Hepatic abscess: changes in etiology, diagnosis, and management. Ann Surg. 1990; 212:655–662.
Article13. Shimokawa Y, Okuda K, Kubo Y, et al. Serum glutamic ox-alacetic transaminase/glutamic pyruvic transaminase ratios in hepatocellular carcinoma. Cancer. 1977; 40:319–324.
Article14. Chung YF, Thng CH, Lui HF, et al. Clinical mimicry of hepatocellular carcinoma: imaging-pathological correlation. Singa-pore Med J. 2005; 46:31–36.15. Mcdonald MI, Corey GR, Gallis HA, Durack DT. Single and multiple pyogenic liver abscesses. Natural history, diagnosis and treatment, with emphasis on percutaneous drainage. Medicine (Baltimore). 1984; 63:291–302.16. Liaw YF, Lin DY. Transcatheter hepatic arterial embolization in the treatment of hepatocellular carcinoma. Hepatogastroenterology. 1990; 37:484–488.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Combined Hepatocellular-cholangiocarcinoma Mimicking Pyogenic Liver Abscess
- Two case of primary hepatocellular carcinoma presenting with high fever and leukocytosis mimicking liver abscess
- A Case of Transcatheter Arterial Embolization-nduced Hepatobronchial Fistula in a Patient with Hepatocellular Carcinoma
- A Case of Anoxic Pseudolobular Necrosis of the Liver Associated with Cirrhosis
- Rare Case of Pyogenic Brain Abscess after Transarterial Chemoembolization in a Patient with Hepatocellular Carcinoma: Case Report and Literature Review