Korean J Ophthalmol.
2014 Feb;28(1):1-11. 10.3341/kjo.2014.28.1.1.
Graded Decompression of Orbital Fat and Wall in Patients with Graves' Orbitopathy
- Affiliations
-
- 1Department of Ophthalmology, Institute of Vision Research, Yonsei University College of Medicine, Seoul, Korea. yoonjs@yuhs.ac
- 2Department of Ophthalmology, Soonchunhyang Bucheon Hospital, Soonchunhyang University College of Medicine, Bucheon, Korea.
- KMID: 1792088
- DOI: http://doi.org/10.3341/kjo.2014.28.1.1
Abstract
- PURPOSE
To investigate the results of graded decompression of orbital fat and walls in Graves' orbitopathy (GO) considering the degree of proptosis reduction at surgery and preoperative computed tomography (CT) findings.
METHODS
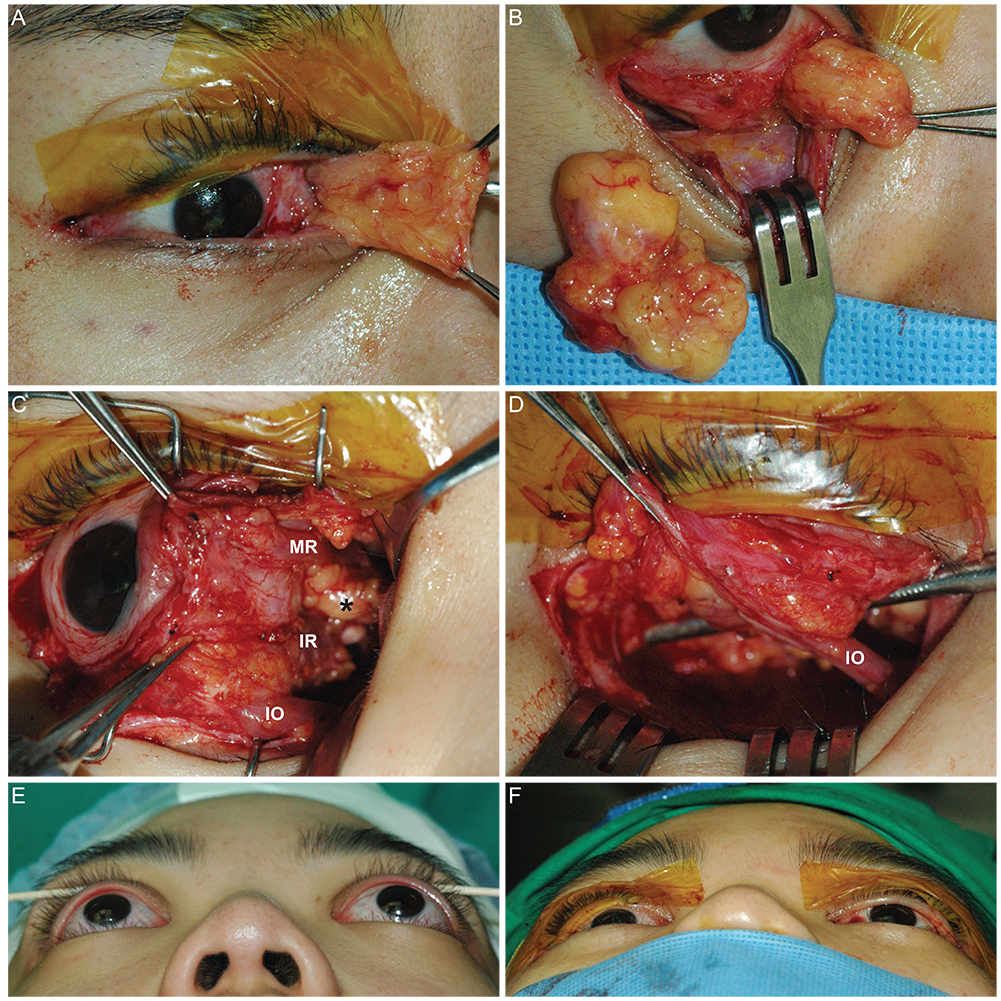
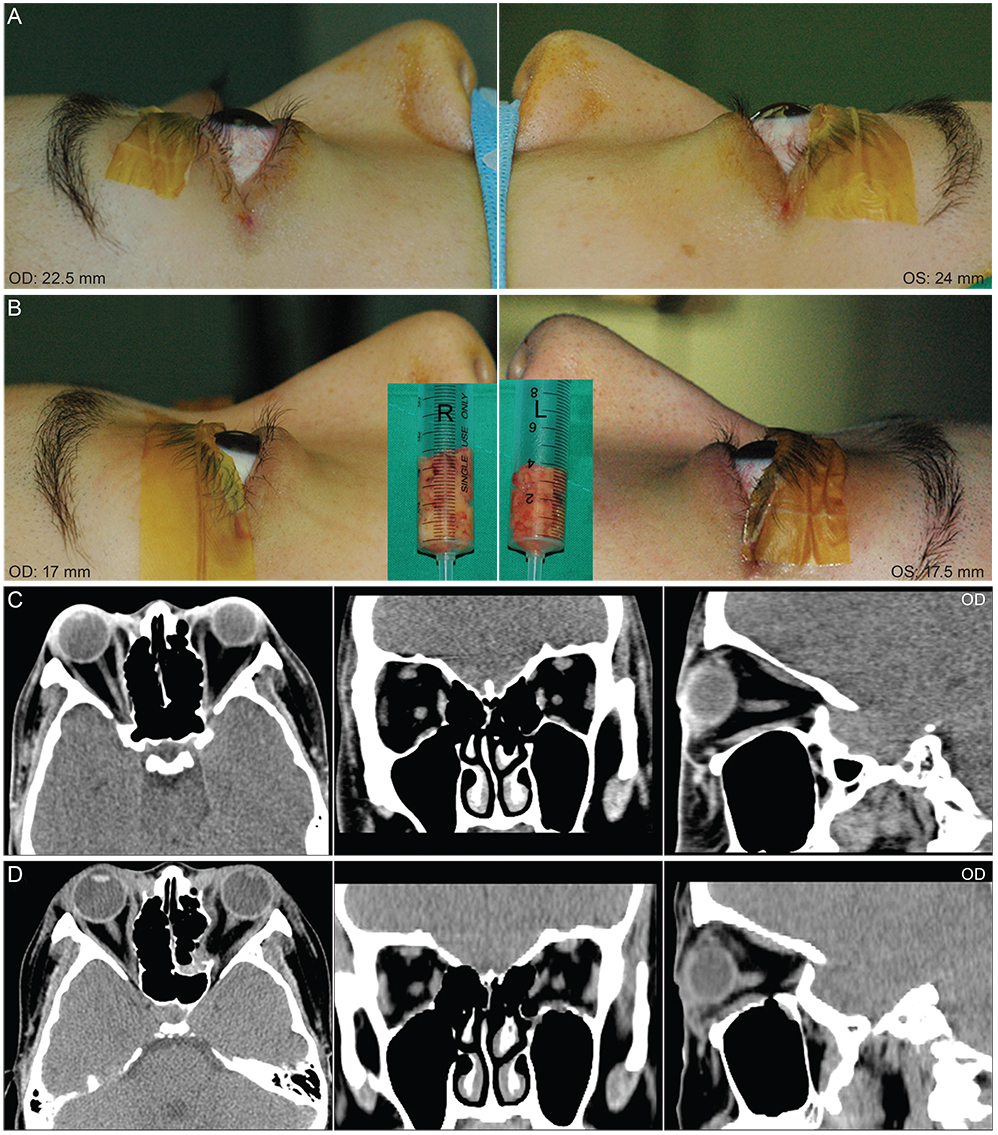
This is a retrospective interventional case series. Graded orbital fat and wall decompression was performed in 90 orbits of 55 patients. In patients with enlarged extraocular muscles and minimal orbital fat proliferation in preoperative CT scans, one- or two-wall decompression of posterior orbit was performed with minimal fat excision. In other cases, the maximal amount of fat tissue was removed from the post-septal area to the apex. If the proptosis was not satisfactorily symmetrically reduced at surgery, one- or two-wall decompression was performed successively. Symmetric reduction of proptosis was consistently confirmed intraoperatively to assure that a desired amount of exophthalmos reduction was achieved.
RESULTS
Four types of decompression were performed: fat only (group 1), fat and one-wall (group 2), fat and two-wall (group 3), and two-wall and minimal fat decompression (group 4). The mean preoperative Hertel value (20.6 +/- 2.8 mm) was reduced significantly at six months postoperatively (16.1 +/- 2.3 mm). Proptosis significantly decreased with a mean of 4.3 +/- 1.7 mm, and the reduction was greatest (5.1 +/- 2.1 mm) in group 3. In group 1, a significant correlation between Hertel change and the volume of resected orbital fat was found (r = 0.479). Diplopia was newly developed or aggravated postoperatively in eight patients, and six of these patients were in group 3. With the exception of one patient, visual acuity improved to nearly normal postoperatively in all patients with optic neuropathy.
CONCLUSIONS
Graded orbital decompression of orbital fat and bony walls, as assessed by the degree of proptosis reduction during surgery, was effective and predictable with minimal complications in GO patients with vision-threatening or cosmetically disfiguring proptosis.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
The Clinical Result of Medial Orbital Decompression in Patients with Thyroid-associated Orbitopathy
Na Ri Park, Jeong Kyu Lee
J Korean Ophthalmol Soc. 2019;60(11):1015-1020. doi: 10.3341/jkos.2019.60.11.1015.Three Wall Orbital Decompression for Compressive Optic Neuropathy in Thyroid Ophthalmopathy
Ji Ah Song, Joo Yeon Kim, Soo Jung Lee, Jae Hwan Kwon
Korean J Otorhinolaryngol-Head Neck Surg. 2019;62(2):125-130. doi: 10.3342/kjorl-hns.2017.00479.
Reference
-
1. Lim JI, Bressler NM, Marsh MJ, Bressler SB. Laser treatment of choroidal neovascularization in patients with angioid streaks. Am J Ophthalmol. 1993; 116:414–423.2. Wiegand TW, Rogers AH, McCabe F, et al. Intravitreal bevacizumab (Avastin) treatment of choroidal neovascularisation in patients with angioid streaks. Br J Ophthalmol. 2009; 93:47–51.3. Menchini U, Virgili G, Introini U, et al. Outcome of choroidal neovascularization in angioid streaks after photodynamic therapy. Retina. 2004; 24:763–771.4. Bartalena L, Pinchera A, Marcocci C. Management of Graves' ophthalmopathy: reality and perspectives. Endocr Rev. 2000; 21:168–199.5. Lyons CJ, Rootman J. Orbital decompression for disfiguring exophthalmos in thyroid orbitopathy. Ophthalmology. 1994; 101:223–230.6. Garrity JA, Fatourechi V, Bergstralh EJ, et al. Results of transantral orbital decompression in 428 patients with severe Graves' ophthalmopathy. Am J Ophthalmol. 1993; 116:533–547.7. Leone CR Jr, Piest KL, Newman RJ. Medial and lateral wall decompression for thyroid ophthalmopathy. Am J Ophthalmol. 1989; 108:160–166.8. Goh MS, McNab AA. Orbital decompression in Graves' orbitopathy: efficacy and safety. Intern Med J. 2005; 35:586–591.9. Kikkawa DO, Pornpanich K, Cruz RC Jr, et al. Graded orbital decompression based on severity of proptosis. Ophthalmology. 2002; 109:1219–1224.10. Horn JD. Status of toric intraocular lenses. Curr Opin Ophthalmol. 2007; 18:58–61.11. Kacker A, Kazim M, Murphy M, et al. "Balanced" orbital decompression for severe Graves' orbitopathy: technique with treatment algorithm. Otolaryngol Head Neck Surg. 2003; 128:228–235.12. Bailey KL, Tower RN, Dailey RA. Customized, single-incision, three-wall orbital decompression. Ophthal Plast Reconstr Surg. 2005; 21:1–9.13. Baldeschi L, MacAndie K, Hintschich C, et al. The removal of the deep lateral wall in orbital decompression: its contribution to exophthalmos reduction and influence on consecutive diplopia. Am J Ophthalmol. 2005; 140:642–647.14. Chiarelli AG, De Min V, Saetti R, et al. Surgical management of thyroid orbitopathy. J Plast Reconstr Aesthet Surg. 2010; 63:240–246.15. Trokel S, Kazim M, Moore S. Orbital fat removal. Decompression for Graves orbitopathy. Ophthalmology. 1993; 100:674–682.16. Unal M, Leri F, Konuk O, Hasanreisoglu B. Balanced orbital decompression combined with fat removal in Graves ophthalmopathy: do we really need to remove the third wall? Ophthal Plast Reconstr Surg. 2003; 19:112–118.17. Alsuhaibani AH, Carter KD, Policeni B, Nerad JA. Orbital volume and eye position changes after balanced orbital decompression. Ophthal Plast Reconstr Surg. 2011; 27:158–163.18. Kulwin DR, Cotton RT, Kersten RC. Combined approach to orbital decompression. Otolaryngol Clin North Am. 1990; 23:381–390.19. Elisevich K, Allen L, Bite U, Colcleugh R. Decompression for dysthyroid ophthalmopathy via the orbital rim approach. Technical note. J Neurosurg. 1994; 80:580–583.20. McCord CD Jr. Current trends in orbital decompression. Ophthalmology. 1985; 92:21–33.21. Tallstedt L, Papatziamos G, Lundblad L, Anggard A. Results of transantral orbital decompression in patients with thyroid-associated ophthalmopathy. Acta Ophthalmol Scand. 2000; 78:206–210.22. Stanley RJ, McCaffrey TV, Offord KP, DeSanto LW. Superior and transantral orbital decompression procedures. Effects on increased intraorbital pressure and orbital dynamics. Arch Otolaryngol Head Neck Surg. 1989; 115:369–373.23. Kalmann R, Mourits MP, van der Pol JP, Koornneef L. Coronal approach for rehabilitative orbital decompression in Graves' ophthalmopathy. Br J Ophthalmol. 1997; 81:41–45.24. Liao SL, Huang SW. Correlation of retrobulbar volume change with resected orbital fat volume and proptosis reduction after fatty decompression for Graves ophthalmopathy. Am J Ophthalmol. 2011; 151:465–469.25. Alsuhaibani AH, Carter KD, Policeni B, Nerad JA. Effect of orbital bony decompression for Graves' orbitopathy on the volume of extraocular muscles. Br J Ophthalmol. 2011; 95:1255–1258.26. Alper MG. Pioneers in the history of orbital decompression for Graves' ophthalmopathy RU Kroenlein (1847-1910), O. Hirsch (1877-1965) and H.C. Naffziger (1884-1961). Doc Ophthalmol. 1995; 89:163–171.27. Van der Wal KG, de Visscher JG, Boukes RJ, Smeding B. Surgical treatment of Graves orbitopathy: a modified balanced technique. Int J Oral Maxillofac Surg. 2001; 30:254–258.28. Richter DF, Stoff A, Olivari N. Transpalpebral decompression of endocrine ophthalmopathy by intraorbital fat removal (Olivari technique): experience and progression after more than 3000 operations over 20 years. Plast Reconstr Surg. 2007; 120:109–123.29. Olivari N. Transpalpebral decompression of endocrine ophthalmopathy (Graves' disease) by removal of intraorbital fat: experience with 147 operations over 5 years. Plast Reconstr Surg. 1991; 87:627–641.30. Trokel S, Kazim M, Moore S. Orbital fat removal. Decompression for Graves orbitopathy. Ophthalmology. 1993; 100:674–682.31. Wu CH, Chang TC, Liao SL. Results and predictability of fat-removal orbital decompression for disfiguring graves exophthalmos in an Asian patient population. Am J Ophthalmol. 2008; 145:755–759.32. Robert PY, Rivas M, Camezind P, et al. Decrease of intraocular pressure after fat-removal orbital decompression in Graves disease. Ophthal Plast Reconstr Surg. 2006; 22:92–95.33. Goldberg RA, Kim AJ, Kerivan KM. The lacrimal keyhole, orbital door jamb, and basin of the inferior orbital fissure. Three areas of deep bone in the lateral orbit. Arch Ophthalmol. 1998; 116:1618–1624.34. Goldberg RA, Weinberg DA, Shorr N, Wirta D. Maximal, three-wall, orbital decompression through a coronal approach. Ophthalmic Surg Lasers. 1997; 28:832–843.35. Seiff SR, Tovilla JL, Carter SR, Choo PH. Modified orbital decompression for dysthyroid orbitopathy. Ophthal Plast Reconstr Surg. 2000; 16:62–66.36. Kazim M, Trokel SL, Acaroglu G, Elliott A. Reversal of dysthyroid optic neuropathy following orbital fat decompression. Br J Ophthalmol. 2000; 84:600–605.37. Nunery WR, Nunery CW, Martin RT, et al. The risk of diplopia following orbital floor and medial wall decompression in subtypes of ophthalmic Graves' disease. Ophthal Plast Reconstr Surg. 1997; 13:153–160.38. Garrity JA. Orbital lipectomy (fat decompression) for thyroid eye disease: an operation for everyone? Am J Ophthalmol. 2011; 151:399–400.39. Chng CL, Seah LL, Khoo DH. Ethnic differences in the clinical presentation of Graves' ophthalmopathy. Best Pract Res Clin Endocrinol Metab. 2012; 26:249–258.40. Sasim IV, de Graaf ME, Berendschot TT, et al. Coronal or swinging eyelid decompression for patients with disfiguring proptosis in Graves' orbitopathy? Comparison of results in one center. Ophthalmology. 2005; 112:1310–1315.41. Ben Simon GJ, Schwarcz RM, Mansury AM, et al. Minimally invasive orbital decompression: local anesthesia and hand-carved bone. Arch Ophthalmol. 2005; 123:1671–1675.42. Chang M, Baek S, Lee TS. Long-term outcomes of unilateral orbital fat decompression for thyroid eye disease. Graefes Arch Clin Exp Ophthalmol. 2013; 251:935–939.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Long-term Result of Fat Orbital Decompression
- Associations between Orbital Morphology and Exophthalmos Changes after Endoscopic Orbital Decompression to Treat Thyroid-related Orbitopathy
- Evaluation of Stereotactic Navigation During Orbital Decompression in Thyroid-Associated Orbitopathy Patients
- Orbital Decompression for Dysthyroid Orbitopathy
- Endoscopic Orbital Decompression for Dysthyroid Orbitopathy