Ann Lab Med.
2014 Jul;34(4):328-331. 10.3343/alm.2014.34.4.328.
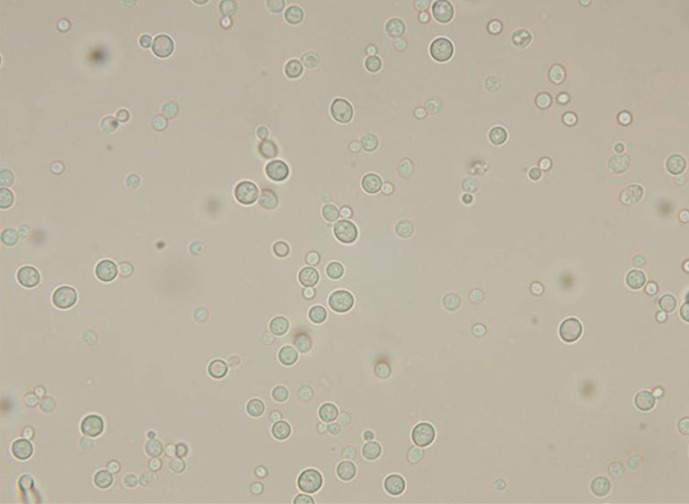
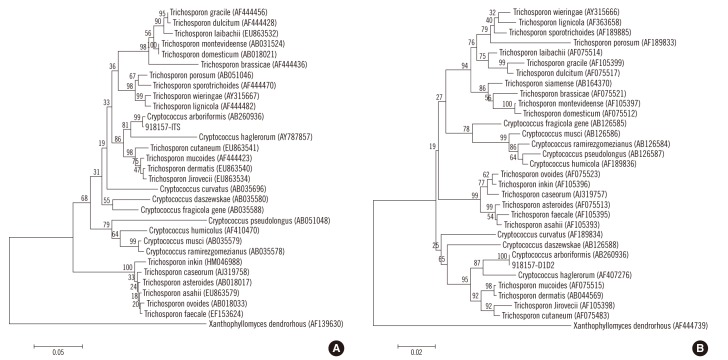
First Case of Continuous Ambulatory Peritoneal Dialysis-Related Peritonitis Caused by Cryptococcus arboriformis
- Affiliations
-
- 1Department of Rehabilitation Medicine, Eulji General Hospital, College of Medicine, Eulji University, Seoul, Korea.
- 2Department of Laboratory Medicine, Eulji General Hospital, College of Medicine, Eulji University, Seoul, Korea. jdchae@eulji.ac.kr
- 3Department of Internal Medicine, Eulji General Hospital, College of Medicine, Eulji University, Seoul, Korea.
- 4Division of Nephrology, Eulji General Hospital, College of Medicine, Eulji University, Seoul, Korea.
- 5Department of Laboratory Medicine, Inje University College of Medicine, Busan, Korea.
- 6Department of Laboratory Medicine, University of Ulsan College of Medicine and Asan Medical Center, Seoul, Korea.
- KMID: 1791944
- DOI: http://doi.org/10.3343/alm.2014.34.4.328
Abstract
- No abstract available.
MeSH Terms
-
Amphotericin B/therapeutic use
Antifungal Agents/pharmacology/therapeutic use
Cryptococcosis/*diagnosis/drug therapy/microbiology
Cryptococcus/classification/drug effects/*isolation & purification
DNA, Ribosomal/chemistry/metabolism
Fluconazole/therapeutic use
Humans
Male
Microbial Sensitivity Tests
Middle Aged
Peritoneal Dialysis, Continuous Ambulatory
Peritonitis/*diagnosis/etiology
Phylogeny
Saccharomyces cerevisiae/drug effects/isolation & purification
Sequence Homology, Nucleic Acid
Amphotericin B
Antifungal Agents
DNA, Ribosomal
Fluconazole
Figure
Reference
-
1. Davenport A. Peritonitis remains the major clinical complication of peritoneal dialysis: the London, UK, peritonitis audit 2002-2003. Perit Dial Int. 2009; 29:297–302. PMID: 19458302.
Article2. Matuszkiewicz-Rowinska J. Update on fungal peritonitis and its treatment. Perit Dial Int. 2009; 29(Suppl 2):S161–S165. PMID: 19270208.
Article3. Miles R, Hawley CM, McDonald SP, Brown FG, Rosman JB, Wiggins KJ, et al. Predictors and outcomes of fungal peritonitis in peritoneal dialysis patients. Kidney Int. 2009; 76:622–628. PMID: 19516241.
Article4. Nikitidou O, Liakopoulos V, Kiparissi T, Divani M, Leivaditis K, Dombros N. Peritoneal dialysis-related infections recommendations: 2010 update. What is new? Int Urol Nephrol. 2012; 44:593–600. PMID: 21744125.
Article5. Indhumathi E, Chandrasekaran V, Jagadeswaran D, Varadarajan M, Abraham G, Soundararajan P. The risk factors and outcome of fungal peritonitis in continuous ambulatory peritoneal dialysis patients. Indian J Med Microbiol. 2009; 27:59–61. PMID: 19172063.
Article6. Rosa NG, Silva S, Lopes JA, Branco P, de Almeida E, Ribeiro C, et al. Fungal peritonitis in peritoneal dialysis patients: Is previous antibiotic therapy an essential condition? Mycoses. 2007; 50:79–81. PMID: 17302754.
Article7. Yinnon AM, Solages A, Treanor JJ. Cryptococcal peritonitis: report of a case developing during continuous ambulatory peritoneal dialysis and review of the literature. Clin Infect Dis. 1993; 17:736–741. PMID: 8268358.
Article8. Mocan H, Murphy AV, Beattie TJ, McAllister TA. Fungal peritonitis in children on continuous ambulatory peritoneal dialysis. Scott Med J. 1989; 34:494–496. PMID: 2799371.
Article9. Sinnott JT 4th, Rodnite J, Emmanuel PJ, Campos A. Cryptococcus laurentii infection complicating peritoneal dialysis. Pediatr Infect Dis J. 1989; 8:803–805. PMID: 2594458.
Article10. Sugita T, Takashima M, Sano A, Nishimura K, Kinebuchi T, Yamaguchi S, et al. Cryptococcus arboriformis Sp. Nov., a novel anamorphic basidiomycetous yeast species isolated from a patient's urine. Microbiol Immunol. 2007; 51:543–545. PMID: 17579264.11. Piraino B, Bailie GR, Bernardini J, Boeschoten E, Gupta A, Holmes C, et al. Peritoneal dialysis-related infections recommendations: 2005 update. Perit Dial Int. 2005; 25:107–131. PMID: 15796137.
Article12. Chang TI, Kim HW, Park JT, Lee DH, Lee JH, Yoo TH, et al. Early catheter removal improves patient survival in peritoneal dialysis patients with fungal peritonitis: results of ninety-four episodes of fungal peritonitis at a single center. Perit Dial Int. 2011; 31:60–66. PMID: 20505136.
Article13. Keane WF, Bailie GR, Boeschoten E, Gokal R, Golper TA, Holmes CJ, et al. Adult peritoneal dialysis-related peritonitis treatment recommendations: 2000 update. Perit Dial Int. 2000; 20:396–411. PMID: 11007371.
Article14. Fera MT, La Camera E, De Sarro A. New triazoles and echinocandins: mode of action, in vitro activity and mechanisms of resistance. Expert Rev Anti Infect Ther. 2009; 7:981–998. PMID: 19803707.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Continuous Ambulatory Peritoneal Dialysis Related Peritonitis Caused by Ochrobactrum anthropi
- A Case Report of Mycobacterium abscessus Peritonitis in a Patient on Continuous Ambulatory Peritoneal Dialysis
- The three cases of fungal peritonitis due to trichosporon beigelii during continuous ambulatory peritoneal dialysis
- A Case of Cryptococcal Peritonitis and Causative Organisms of Peritonitis in a Continuous Ambulatory Peritoneal Dialysis Patient
- Candida zeylanoides Peritonitis in a Continuous Ambulatory Peritoneal Dialysis Patient