Korean J Gastroenterol.
2014 Jul;64(1):49-53. 10.4166/kjg.2014.64.1.49.
Recurrence of Multiple Focal Nodular Hyperplasia in a Young Male Patient
- Affiliations
-
- 1Department of Internal Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 2Department of Hospital Pathology, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 3Department of General Surgery, College of Medicine, The Catholic University of Korea, Seoul, Korea. parkiy@catholic.ac.kr
- KMID: 1791895
- DOI: http://doi.org/10.4166/kjg.2014.64.1.49
Abstract
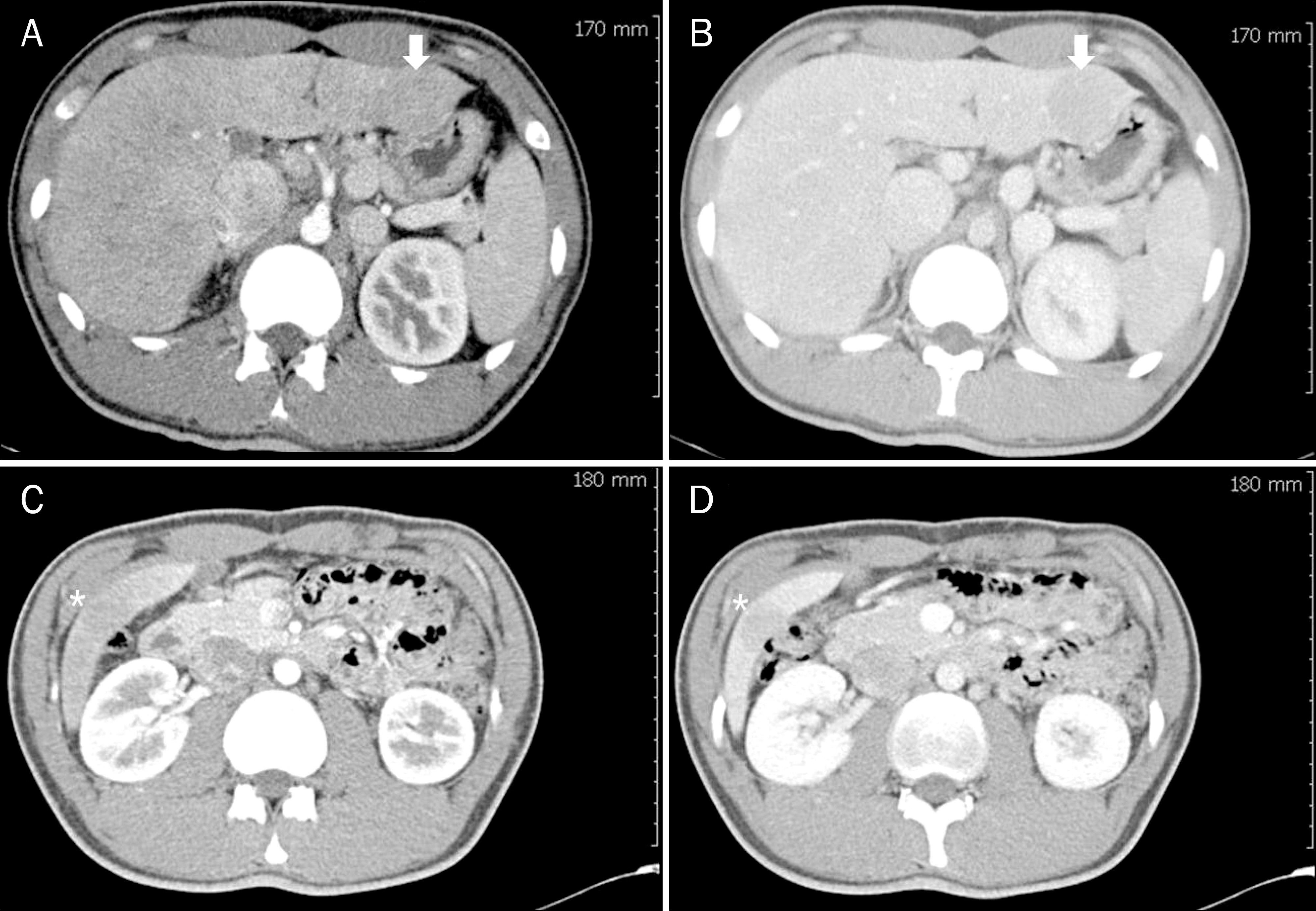
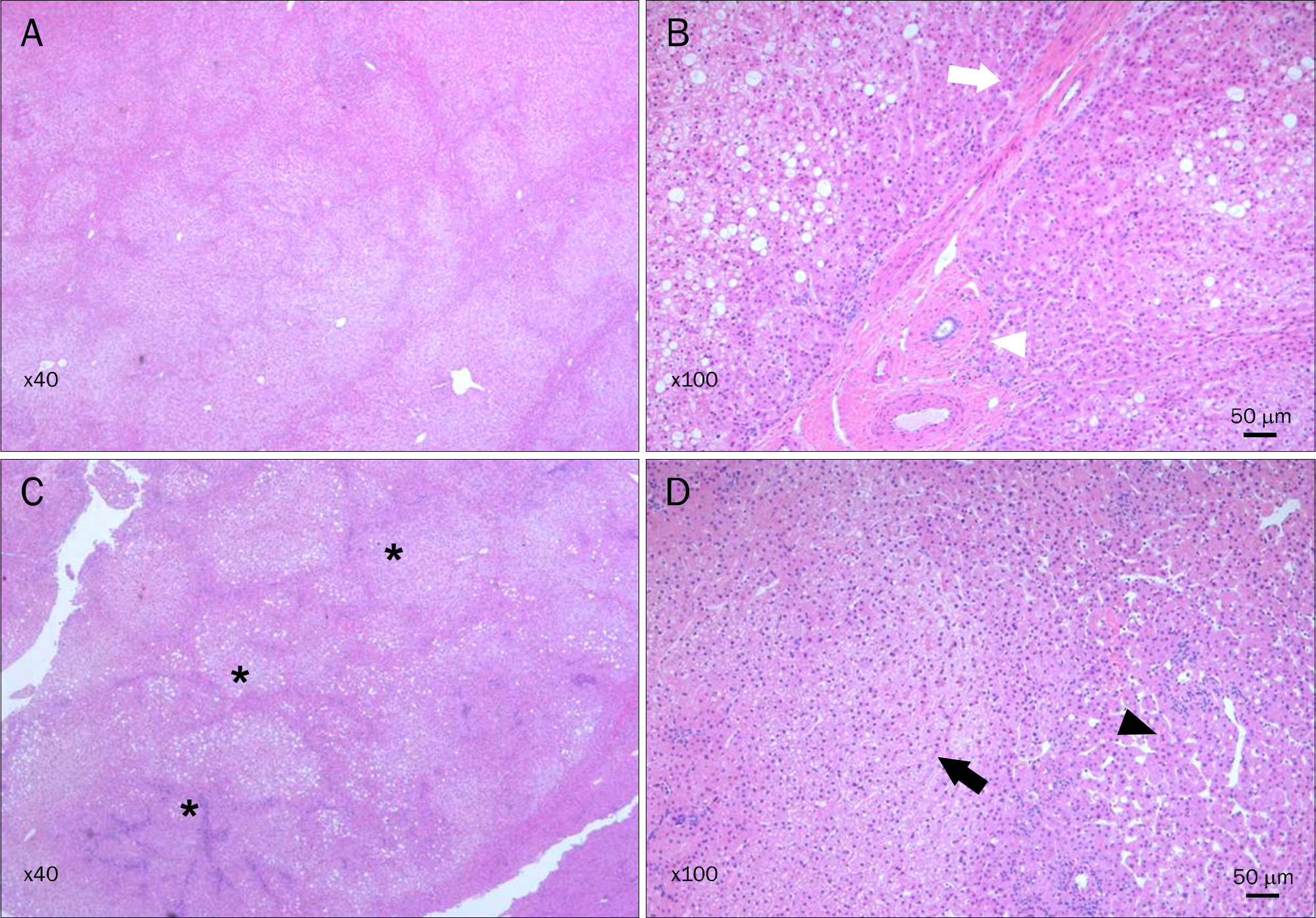
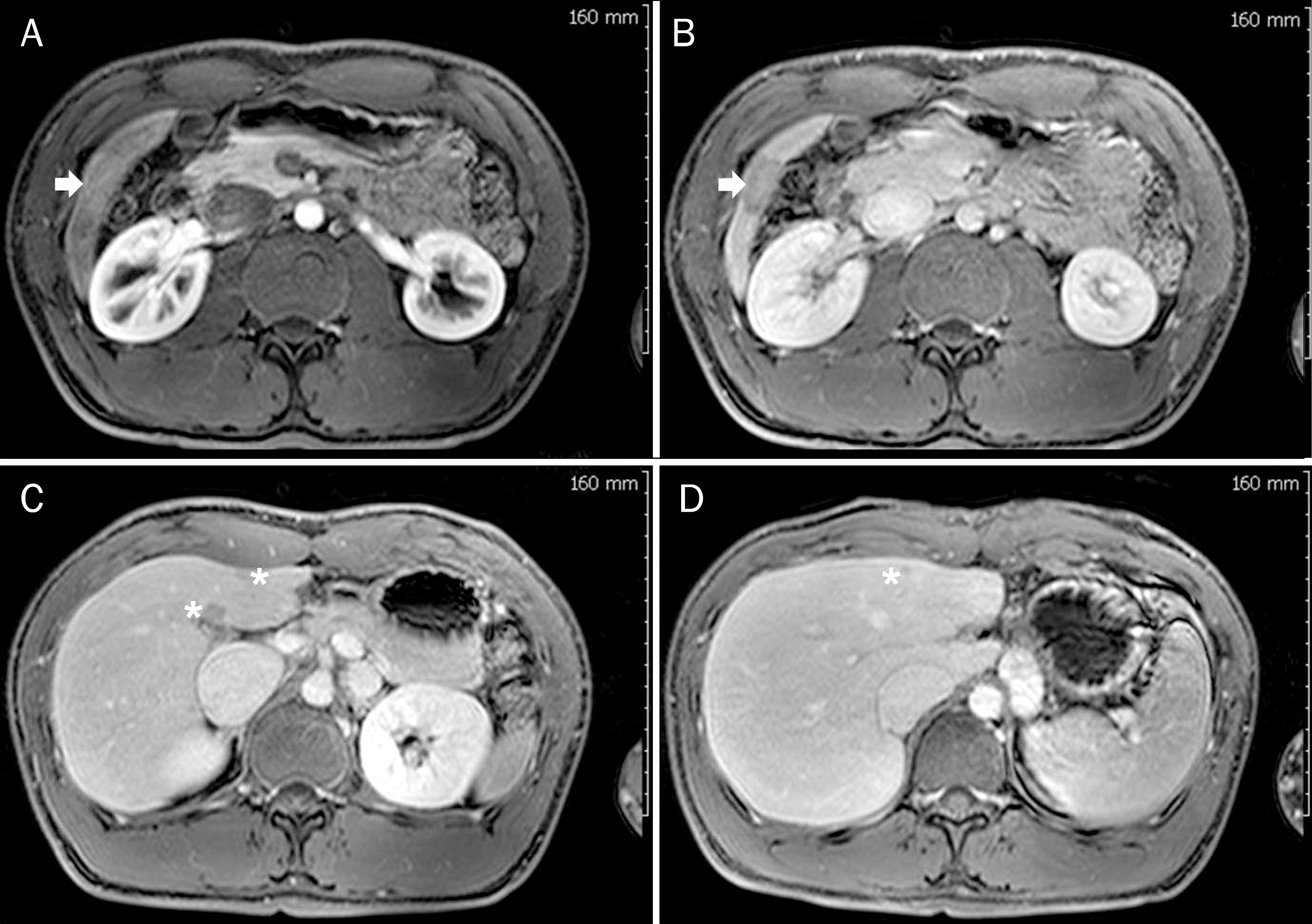
- Focal nodular hyperplasia (FNH) is the second most common benign hepatic tumor that is usually found in women. Diagnosis of FNH mainly depends on imaging studies such as color Doppler flow imaging, computed tomography, and magnetic resonance imaging. It is characterized by the presence of stellate central scar and is nowadays incidentally diagnosed with increasing frequency due to advances in radiologic imaging technique. FNH typically presents as a single lesion in 70% of cases and generally does not progress to malignancy or recur after resection. Herein, we report a case of a young male patient with recurrent multiple FNH who underwent surgical resection for presumed hepatic adenoma on computed tomography.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Cristiano A, Dietrich A, Spina JC, Ardiles V, de Santibañes E. Focal nodular hyperplasia and hepatic adenoma: current diagnosis and management. Updates Surg. 2014; 66:9–21.
Article2. Carlson SK, Johnson CD, Bender CE, Welch TJ. CT of focal nodular hyperplasia of the liver. AJR Am J Roentgenol. 2000; 174:705–712.
Article3. Wanless IR, Mawdsley C, Adams R. On the pathogenesis of focal nodular hyperplasia of the liver. Hepatology. 1985; 5:1194–1200.
Article4. Shen YH, Fan J, Wu ZQ, et al. Focal nodular hyperplasia of the liver in 86 patients. Hepatobiliary Pancreat Dis Int. 2007; 6:52–57.5. Sudour H, Mainard L, Baumann C, Clement L, Salmon A, Bordigoni P. Focal nodular hyperplasia of the liver following hematopoietic SCT. Bone Marrow Transplant. 2009; 43:127–132.
Article6. Kim J, Nikiforov YE, Moulton JS, Lowy AM. Multiple focal nodular hyperplasia of the liver in a 21-year-old woman. J Gastrointest Surg. 2004; 8:591–595.
Article7. Fabre A, Audet P, Vilgrain V, et al. Histologic scoring of liver biopsy in focal nodular hyperplasia with atypical presentation. Hepatology. 2002; 35:414–420.
Article8. Procacci C, Fugazzola C, Cinquino M, et al. Contribution of CT to characterization of focal nodular hyperplasia of the liver. Gastrointest Radiol. 1992; 17:63–73.
Article9. Finley AC, Hosey JR, Noone TC, Shackelford DM, Varadarajulu S. Multiple focal nodular hyperplasia syndrome: diagnosis with dynamic, gadolinium-enhanced MRI. Magn Reson Imaging. 2005; 23:511–513.
Article10. Bieze M, Bennink RJ, El-Massoudi Y, et al. The use of 18F-fluo-romethylcholine PET/CT in differentiating focal nodular hyperplasia from hepatocellular adenoma: a prospective study of diagnostic accuracy. Nucl Med Commun. 2013; 34:146–154.11. Sadowski DC, Lee SS, Wanless IR, Kelly JK, Heathcote EJ. Progressive type of focal nodular hyperplasia characterized by multiple tumors and recurrence. Hepatology. 1995; 21:970–975.
Article12. Shetty JB, Amrapurkar AD, Shenoy AS. Multiple focal nodular hyperplasia, an incidental finding on autopsy. Indian J Pathol Microbiol. 2011; 54:822–824.13. Wanless IR, Albrecht S, Bilbao J, et al. Multiple focal nodular hyperplasia of the liver associated with vascular malformations of various organs and neoplasia of the brain: a new syndrome. Mod Pathol. 1989; 2:456–462.14. Devarbhavi H, Abraham S, Kamath PS. Significance of nodular regenerative hyperplasia occurring de novo following liver transplantation. Liver Transpl. 2007; 13:1552–1556.
Article15. Donadon M, Di Tommaso L, Roncalli M, Torzilli G. Multiple focal nodular hyperplasias induced by oxaliplatin-based chemotherapy. World J Hepatol. 2013; 5:340–344.
Article