Korean J Gastroenterol.
2014 Apr;63(4):253-257. 10.4166/kjg.2014.63.4.253.
A Case of Alpha-cell Nesidioblastosis and Hyperplasia with Multiple Glucagon-producing Endocrine Cell Tumor of the Pancreas
- Affiliations
-
- 1Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea. bang7028@yuhs.ac
- 2Department of Surgery, Yonsei University College of Medicine, Seoul, Korea.
- 3Department of Pathology, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 1791884
- DOI: http://doi.org/10.4166/kjg.2014.63.4.253
Abstract
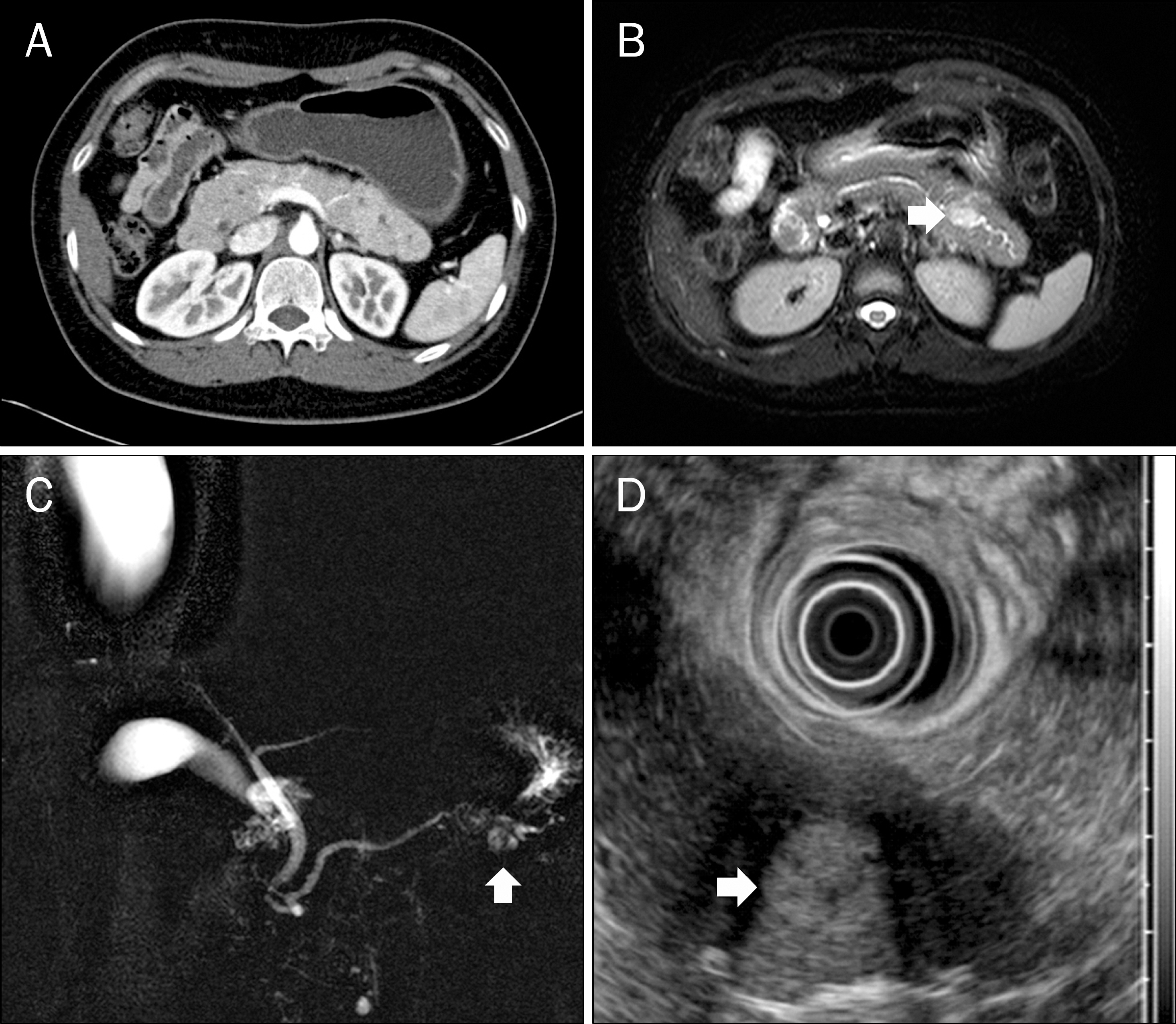
- Nesidioblastosis is a term used to describe pathologic overgrowth of pancreatic islet cells. It also means maldistribution of islet cells within the ductules of exocrine pancreas. Generally, nesidioblastosis occurs in beta-cell and causes neonatal hyperinsulinemic hypoglycemia or adult noninsulinoma pancreatogenous hypoglycemia syndrome. Alpha-cell nesidioblastosis and hyperplasia is an extremely rare disorder. It often accompanies glucagon-producing marco- and mircoadenoma without typical glucagonoma syndrome. A 35-year-old female was referred to our hospital with recurrent acute pancreatitis. On radiologic studies, 1.5 cm sized mass was noted in pancreas tail. Cytological evaluation with EUS-fine-needle aspiration suggested serous cystadenoma. She received distal pancreatectomy. The histologic examination revealed a 1.7 cm sized neuroendocrine tumor positive for immunohistochemical staining with glucagon antibody. Multiple glucagon-producing micro endocrine cell tumors were scattered next to the main tumor. Additionally, diffuse hyperplasia of pancreatic islets and ectopic proliferation of islet cells in centroacinar area, findings compatible to nesidioblastosis, were seen. These hyperplasia and almost all nesidioblastic cells were positive for glucagon immunochemistry. Even though serum glucagon level still remained higher than the reference value, she has been followed-up without any evidence of recurrence or hormone related symptoms. Herein, we report a case of alpha-cell nesidioblastosis and hyperplasia combined with glucagon-producing neuroendocrine tumor with literature review.
MeSH Terms
-
Adult
Chromogranin A/blood
Female
Glucagon/*metabolism
Glucagon-Secreting Cells/metabolism
Humans
Hyperplasia/complications/*diagnosis
Islets of Langerhans/metabolism/ultrasonography
Nesidioblastosis/complications/*diagnosis
Neuroendocrine Tumors/complications/*diagnosis/pathology
Pancreas/*pathology
Tomography, X-Ray Computed
Chromogranin A
Glucagon
Figure
Reference
-
References
1. Zumkeller W. Nesidioblastosis. Endocr Relat Cancer. 1999; 6:421–428.
Article2. van der Wal BC, de Krijger RR, de Herder WW, et al. Adult hyperinsulinemic hypoglycemia not caused by an insulinoma: a report of two cases. Virchows Arch. 2000; 436:481–486.
Article3. Wängberg B, Nilsson O, Grimelius L, Lundell L, Ahlman H. Nesidiodysplasia. A rare cause of hyperinsulinemia in an adult patient. Lakartidningen. 1999; 96:4655–4657.4. Delonlay P, Simon A, Galmiche-Rolland L, et al. Neonatal hyper-insulinism: clinicopathologic correlation. Hum Pathol. 2007; 38:387–399.
Article5. Witteles RM, Straus II FH, Sugg SL, Koka MR, Costa EA, Kaplan EL. Adult-onset nesidioblastosis causing hypoglycemia: an important clinical entity and continuing treatment dilemma. Arch Surg. 2001; 136:656–663.6. Rahier J, Fält K, Müntefering H, Becker K, Gepts W, Falkmer S. The basic structural lesion of persistent neonatal hypoglycae-mia with hyperinsulinism: deficiency of pancreatic D cells or hyperactivity of B cells? Diabetologia. 1984; 26:282–289.
Article7. Balas D, Senegas-Balas F, Delvaux M, et al. Silent human pancreatic glucagonoma and "A" nesidioblastosis. Pancreas. 1988; 3:734–739.
Article8. Martignoni ME, Kated H, Stiegler M, et al. Nesidioblastosis with glucagon-reactive islet cell hyperplasia: a case report. Pancreas. 2003; 26:402–405.
Article9. Yu R, Nissen NN, Dhall D, Heaney AP. Nesidioblastosis and hyperplasia of alpha cells, microglucagonoma, and nonfunctioning islet cell tumor of the pancreas: review of the literature. Pancreas. 2008; 36:428–431.10. Ouyang D, Dhall D, Yu R. Pathologic pancreatic endocrine cell hyperplasia. World J Gastroenterol. 2011; 17:137–143.
Article11. Zhou C, Dhall D, Nissen NN, Chen CR, Yu R. Homozygous P86S mutation of the human glucagon receptor is associated with hy-perglucagonemia, alpha cell hyperplasia, and islet cell tumor. Pancreas. 2009; 38:941–946.12. Henopp T, Anlauf M, Schmitt A, et al. Glucagon cell adenoma-tosis: a newly recognized disease of the endocrine pancreas. J Clin Endocrinol Metab. 2009; 94:213–217.
Article13. Novaes G, Chetto-de-Queiroz A, De-Carvalho-Cardoso C, Burla-cchini-de-Carvalho MH, Ribeiro-Filho LA, Oliveira-Gonçalves A. Nesidioblastosis associated with chronic experimental pancreatitis produced by a scorpion toxin, tityustoxin, in rats. Braz J Med Biol Res. 1990; 23:1149–1151.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Two cases of islet cell hyperplasia with nesidioblastosis
- Diffuse Nesidioblastosis of the Pancreasin Adult with Persistent Hyperinsulinemic Hypoglycemia
- Nesidioblastosis of the Pancreas
- A Case of Surgical Treatment of Nesidioblastosis with Hyperinsulinemic Hypoglycemia in an Adult
- Multiple Pancreatic Islet Cell Tumors with Diverse Hormonal Expression in a Multiple Endocrine Neoplasia Type I Patient: A Case Report