J Korean Med Sci.
2014 Jul;29(7):950-956. 10.3346/jkms.2014.29.7.950.
Relationship between Neutrophil-to-Lymphocyte Ratio and Plaque Components in Patients with Coronary Artery Disease: Virtual Histology Intravascular Ultrasound Analysis
- Affiliations
-
- 1The Division of Cardiology, Chonnam National University Hospital, Gwangju, Korea. hyj200@hanmail.net
- 2College of Nursing, Chonnam National University, Gwangju, Korea.
- KMID: 1789954
- DOI: http://doi.org/10.3346/jkms.2014.29.7.950
Abstract
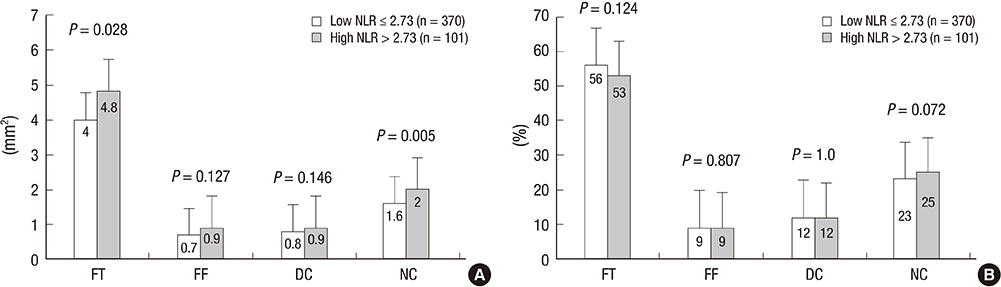
- The aim of this study was to evaluate the relation between neutrophil-to-lymphocyte ratio (NLR) and plaque components assessed by virtual histology-intravascular ultrasound in 399 coronary artery disease (CAD) patients with 471 coronary lesions. We classified the lesions into two groups according to the NLR on admission {low NLR group (NLR< or =2.73 [n=370]) vs. high NLR group (NLR>2.73 [n=101])}. By volumetric analysis, total atheroma and the absolute necrotic core (NC) volumes were significantly greater in high NLR group (249.9+/-149.7 microL vs. 192.5+/-127.7 microL, P=0.001, and 32.7+/-26.8 microL vs. 22.8+/-19.4 microL, P=0.001, respectively) and thin-cap fibroatheroma (TCFA) was observed more frequently in high NLR group (33% vs. 18%, P=0.001). ST segment elevation myocardial infarction (odds ratio [OR], 2.159; 95% CI, 1.000-4.660, P=0.050) and NLR>2.73 (OR, 1.848; 95% CI, 1.016-3.360, P=0.044) and total atheroma volume (OR, 1.003; 95% CI, 1.001-1.004, P=0.004) were the independent predictors of TCFA. CAD patients with high NLR had more vulnerable plaque components (greater NC-containing plaques) than those with low NLR.
MeSH Terms
-
Aged
C-Reactive Protein/analysis
Coronary Angiography
Coronary Artery Disease/*diagnosis/pathology
Female
Hospitals, University
Humans
Lymphocytes/*cytology
Male
Middle Aged
Neutrophils/*cytology
Odds Ratio
Patients
Plaque, Atherosclerotic/metabolism/*pathology
Retrospective Studies
Ultrasonography, Interventional
C-Reactive Protein
Figure
Reference
-
1. Libby P, Ridker PM, Maseri A. Inflammation and atherosclerosis. Circulation. 2002; 105:1135–1143.2. Margolis KL, Manson JE, Greenland P, Rodabough RJ, Bray PF, Safford M, Grimm RH Jr, Howard BV, Assaf AR, Prentice R. Leukocyte count as a predictor of cardiovascular events and mortality in postmenopausal women: the Women's Health Initiative Observational Study. Arch Intern Med. 2005; 165:500–508.3. Duffy BK, Gurm HS, Rajagopal V, Gupta R, Ellis SG, Bhatt DL. Usefulness of an elevated neutrophil to lymphocyte ratio in predicting long-term mortality after percutaneous coronary intervention. Am J Cardiol. 2006; 97:993–996.4. Muhmmed Suliman MA, Bahnacy Juma AA, Ali Almadhani AA, Pathare AV, Alkindi SS, Uwe Werner F. Predictive value of neutrophil to lymphocyte ratio in outcomes of patients with acute coronary syndrome. Arch Med Res. 2010; 41:618–622.5. Arbel Y, Finkelstein A, Halkin A, Birati EY, Revivo M, Zuzut M, Shevach A, Berliner S, Herz I, Keren G, et al. Neutrophil/lymphocyte ratio is related to the severity of coronary artery disease and clinical outcome in patients undergoing angiography. Atherosclerosis. 2012; 225:456–460.6. Horne BD, Anderson JL, John JM, Weaver A, Bair TL, Jensen KR, Renlund DG, Muhlestein JB. Intermountain Heart Collaborative Study Group. Which white blood cell subtypes predict increased cardiovascular risk? J Am Coll Cardiol. 2005; 45:1638–1643.7. Tamhane UU, Aneja S, Montgomery D, Rogers EK, Eagle KA, Gurm HS. Association between admission neutrophil to lymphocyte ratio and outcomes in patients with acute coronary syndrome. Am J Cardiol. 2008; 102:653–657.8. Núñez J, Núñez E, Bodí V, Sanchis J, Miñana G, Mainar L, Santas E, Merlos P, Rumiz E, Darmofal H, et al. Usefulness of the neutrophil to lymphocyte ratio in predicting long-term mortality in ST segment elevation myocardial infarction. Am J Cardiol. 2008; 101:747–752.9. Cho KH, Jeong MH, Ahmed K, Hachinohe D, Choi HS, Chang SY, Kim MC, Hwang SH, Park KH, Lee MG, et al. Value of early risk stratification using hemoglobin level and neutrophil-to-lymphocyte ratio in patients with ST-elevation myocardial infarction undergoing primary percutaneous coronary intervention. Am J Cardiol. 2011; 107:849–856.10. Park JJ, Jang HJ, Oh IY, Yoon CH, Suh JW, Cho YS, Youn TJ, Cho GY, Chae IH, Choi DJ. Prognostic value of neutrophil to lymphocyte ratio in patients presenting with ST-elevation myocardial infarction undergoing primary percutaneous coronary intervention. Am J Cardiol. 2013; 111:636–642.11. Turak O, Ozcan F, Isleyen A, Tok D, Sokmen E, Buyukkaya E, Aydogdu S, Akpek M, Kaya MG. Usefulness of the neutrophil-to-lymphocyte ratio to predict bare-metal stent restenosis. Am J Cardiol. 2012; 110:1405–1410.12. Roberts WL, Moulton L, Law TC, Farrow G, Cooper-Anderson M, Savory J, Rifai N. Evaluation of nine automated high-sensitivity C-reactive protein methods: implications for clinical and epidemiological applications: part 2. Clin Chem. 2001; 47:418–425.13. Reiber JH, van der Zwet PM, Koning G, von Land CD, van Meurs B, Gerbrands JJ, Buis B, van Voorthuisen AE. Accuracy and precision of quantitative digital coronary arteriography: observer-, short-, and medium-term variabilities. Cathet Cardiovasc Diagn. 1993; 28:187–198.14. Mintz GS, Nissen SE, Anderson WD, Bailey SR, Erbel R, Fitzgerald PJ, Pinto FJ, Rosenfield K, Siegel RJ, Tuzcu EM, et al. American College of Cardiology Clinical Expert Consensus Document on Standards for Acquisition, Measurement and Reporting of Intravascular Ultrasound Studies (IVUS): a report of the American College of Cardiology Task Force on Clinical Expert Consensus Documents. J Am Coll Cardiol. 2001; 37:1478–1492.15. Nair A, Kuban BD, Tuzcu EM, Schoenhagen P, Nissen SE, Vince DG. Coronary plaque classification with intravascular ultrasound radiofrequency data analysis. Circulation. 2002; 106:2200–2206.16. Rodriguez-Granillo GA, García-García HM, Mc Fadden EP, Valgimigli M, Aoki J, de Feyter P, Serruys PW. In vivo intravascular ultrasound-derived thin-cap fibroatheroma detection using ultrasound radiofrequency data analysis. J Am Coll Cardiol. 2005; 46:2038–2042.17. Imtiaz F, Shafique K, Mirza SS, Ayoob Z, Vart P, Rao S. Neutrophil lymphocyte ratio as a measure of systemic inflammation in prevalent chronic diseases in Asian population. Int Arch Med. 2012; 5:2.18. Haim M, Boyko V, Goldbourt U, Battler A, Behar S. Predictive value of elevated white blood cell count in patients with preexisting coronary heart disease: the Bezafibrate Infarction Prevention Study. Arch Intern Med. 2004; 164:433–439.19. Madjid M, Fatemi O. Components of the complete blood count as risk predictors for coronary heart disease: in-depth review and update. Tex Heart Inst J. 2013; 40:17–29.20. Nakachi T, Kosuge M, Hibi K, Ebina T, Hashiba K, Mitsuhashi T, Endo M, Umemura S, Kimura K. C-reactive protein elevation and rapid angiographic progression of nonculprit lesion in patients with non-ST-segment elevation acute coronary syndrome. Circ J. 2008; 72:1953–1959.21. Burke AP, Tracy RP, Kolodgie F, Malcom GT, Zieske A, Kutys R, Pestaner J, Smialek J, Virmani R. Elevated C-reactive protein values and atherosclerosis in sudden coronary death: association with different pathologies. Circulation. 2002; 105:2019–2023.22. Fowler AJ, Agha RA. Neutrophil/lymphocyte ratio is related to the severity of coronary artery disease and clinical outcome in patients undergoing angiography: the growing versatility of NLR. Atherosclerosis. 2013; 228:44–45.23. Virmani R, Burke AP, Farb A, Kolodgie FD. Pathology of the vulnerable plaque. J Am Coll Cardiol. 2006; 47:C13–C18.24. Virmani R, Burke AP, Kolodgie FD, Farb A. Pathology of the thin-cap fibroatheroma: a type of vulnerable plaque. J Interv Cardiol. 2003; 16:267–272.25. Burke AP, Kolodgie FD, Zieske A, Fowler DR, Weber DK, Varghese PJ, Farb A, Virmani R. Morphologic findings of coronary atherosclerotic plaques in diabetics: a postmortem study. Arterioscler Thromb Vasc Biol. 2004; 24:1266–1271.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Practical Application of Coronary Imaging Devices in Cardiovascular Intervention
- Relationship between Coronary Artery Calcium Score by Multidetector Computed Tomography and Plaque Components by Virtual Histology Intravascular Ultrasound
- Neutrophil-to-Lymphocyte Ratio for Risk Assessment in Coronary Artery Disease and Carotid Artery Atherosclerosis
- The Relationship Between Body Mass Index and Left Main Coronary Artery Architecture: A Virtual Histology Intravascular Ultrasound Analysis
- Tissue Characterization of Coronary Plaques Using Intravascular Ultrasound/Virtual Histology