J Korean Med Sci.
2011 Oct;26(10):1277-1285. 10.3346/jkms.2011.26.10.1277.
Carcinoma ex Pleomorphic Adenoma of the Salivary Glands: Distinct Clinicopathologic Features and Immunoprofiles Between Subgroups According to Cellular Differentiation
- Affiliations
-
- 1Department of Pathology, Hallym University College of Medicine, Kangnam Sacred Heart Hospital, Seoul, Korea.
- 2Department of Pathology, Chung-Ang University College of Medicine, Chung-Ang University Hospital, Seoul, Korea.
- 3Department of Otorhinolaryngology, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea.
- 4Department of Pathology, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea. kjc@amc.seoul.kr
- KMID: 1785983
- DOI: http://doi.org/10.3346/jkms.2011.26.10.1277
Abstract
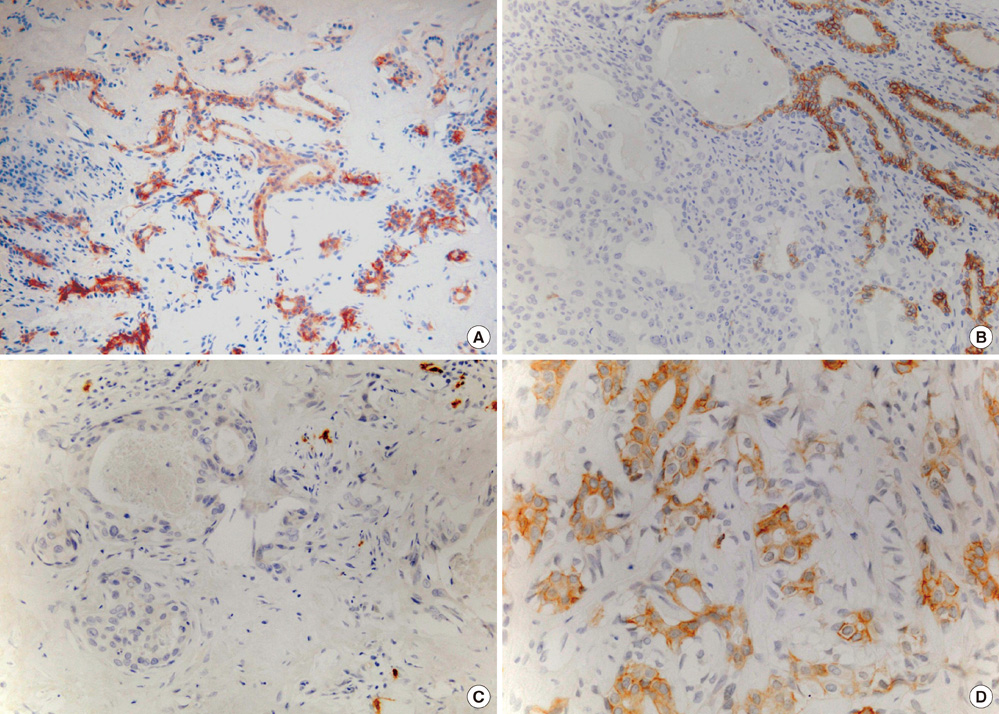
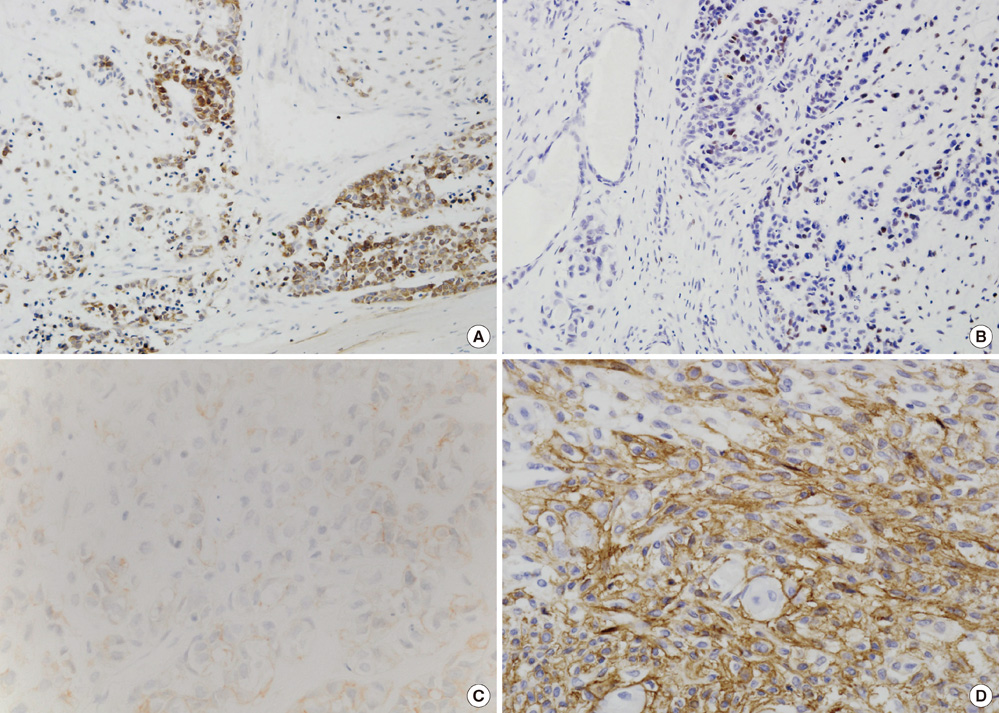
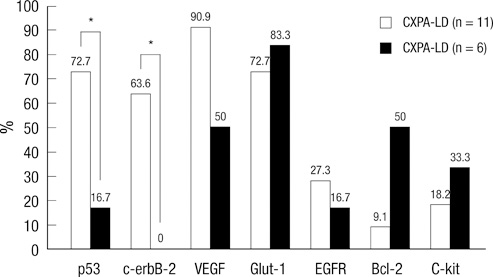
- In carcinoma ex pleomorphic adenoma (CXPA), pleomorphic adenoma (PA) and diverse carcinoma components showing luminal (ductal) or non-luminal (myoepithelial) differentiation coexist. To elucidate the clinicopathological implications of cellular differentiation in CXPA and the potential role of p53, vascular endothelial growth factor (VEGF), c-erbB-2, c-kit, and glucose transporter 1 (Glut-1) in carcinogenesis, we analyzed 11 CXPAs with luminal differentiation (CXPAs-LD) and 6 CXPAs with non-luminal differentiation (CXPAs-NLD) and compared protein expressions in residual PAs and carcinomas by immunohistochemistry. Among the CXPAs-LD, 5 were invasive and 8 were histologically high-grade tumors. The 5-year survival rate was 72.7%. P53, c-erbB-2, VEGF, and Glut-1 were more immunoreactive in carcinoma components than in PAs (P = 0.008, 0.004, 0.002, and 0.024, respectively); c-erbB-2 overexpression was associated with high histological grade (P = 0.024). Carcinoma components frequently lacked c-kit expression (P = 0.009). CXPAs-NLD were all low-grade and invasive with a larger mean tumor size (5.2 cm) than CXPAs-LD (3.3 cm) (P = 0.040). The patients remained disease-free without significant immunohistochemical expression. The immunoprofiles and clinical course of CXPA differed according to cellular differentiation. Therefore, it is important to report the histological subtype and to assess potential biomarkers in diagnostic and therapeutic trials.
Keyword
MeSH Terms
-
Adenoma, Pleomorphic/*immunology/metabolism/*pathology
Adult
Aged
Carcinoma/*immunology/metabolism/*pathology
Cell Differentiation
Female
Glucose Transport Proteins, Facilitative/metabolism
Humans
Male
Middle Aged
Proto-Oncogene Proteins c-kit/metabolism
Receptor, erbB-2/metabolism
Salivary Gland Neoplasms/*immunology/metabolism/*pathology
Tumor Markers, Biological/*analysis
Tumor Suppressor Protein p53/metabolism
Vascular Endothelial Growth Factor A/metabolism
Figure
Cited by 1 articles
-
Frequent apocrine changes in pleomorphic adenoma with malignant transformation: a possible pre-malignant step in ductal carcinoma ex pleomorphic adenoma
Joon Seon Song, Yeseul Kim, Yoon-Se Lee, Seung-Ho Choi, Soon Yuhl Nam, Sang Yoon Kim, Kyung-Ja Cho
J Pathol Transl Med. 2023;57(3):158-165. doi: 10.4132/jptm.2023.03.13.
Reference
-
1. Luna MA, Batsakis JG, Tortoledo ME, del Junco GW. Carcinomas ex monomorphic adenoma of salivary glands. J Laryngol Otol. 1989. 103:756–759.2. Lewis JE, Olsen KD, Sebo TJ. Carcinoma ex pleomorphic adenoma: pathologic analysis of 73 cases. Hum Pathol. 2001. 32:596–604.3. Olsen KD, Lewis JE. Carcinoma ex pleomorphic adenoma: a clinicopathologic review. Head Neck. 2001. 23:705–712.4. Altemani A, Martins MT, Freitas L, Soares F, Araújo NS, Araújo VC. Carcinoma ex pleomorphic adenoma (CXPA): immunoprofile of the cells involved in carcinomatous progression. Histopathology. 2005. 46:635–641.5. Ihrler S, Weiler C, Hirschmann A, Sendelhofert A, Lang S, Guntinas-Lichius O, Arnold G, Zietz C, Harrison JD. Intraductal carcinoma is the precursor of carcinoma ex pleomorphic adenoma and is often associated with dysfunctional p53. Histopathology. 2007. 51:362–371.6. LiVolsi VA, Perzin KH. Malignant mixed tumors arising in salivary glands. I. Carcinomas arising in benign mixed tumors: a clinicopathologic study. Cancer. 1977. 39:2209–2230.7. Hashimoto K, Yamamoto H, Shiratsuchi H, Nakashima T, Tamiya S, Higaki Y, Komune S, Tsuneyoshi M, Oda Y. S100P expression in ductal type of carcinoma ex pleomorphic adenoma. Am J Surg Pathol. 2011. 35:346–355.8. Cheuk W, Chan JK. Fletcher CD, editor. Salivary gland tumors. Diagnostic histopathology of tumors. 2007. London: Elsevier;239–326.9. Tortoledo ME, Luna MA, Batsakis JG. Carcinomas ex pleomorphic adenoma and malignant mixed tumors. Histomorphologic indexes. Arch Otolaryngol. 1984. 110:172–176.10. Katabi N, Gomez D, Klimstra DS, Carlson DL, Lee N, Ghossein R. Prognostic factors of recurrence in salivary carcinoma ex pleomorphic adenoma, with emphasis on the carcinoma histologic subtype: a clinicopathologic study of 43 cases. Hum Pathol. 2010. 41:927–934.11. Demasi AP, Furuse C, Soares AB, Altemani A, Araújo VC. Peroxiredoxin I, platelet-derived growth factor A, and platelet-derived growth factor receptor alpha are overexpressed in carcinoma ex pleomorphic adenoma: association with malignant transformation. Hum Pathol. 2009. 40:390–397.12. Barnes L, Eveson JW, Reichart P, Sidransky D. Barnes L, Reichart P, Sidransky D, editors. Tumours of the salivary glands. Pathology and genetics of head and neck tumours. 2005. Lyon: International Agency for Research on Cancer (IARC) Press;209–282.13. Zietz C, Rössle M, Haas C, Sendelhofert A, Hirschmann A, Sturzl M, Löhrs U. MDM-2 oncoprotein overexpression, p53 gene mutation, and VEGF up-regulation in angiosarcomas. Am J Pathol. 1998. 153:1425–1433.14. DeRoche TC, Hoschar AP, Hunt JL. Immunohistochemical evaluation of androgen receptor, HER-2/neu, and p53 in benign pleomorphic adenomas. Arch Pathol Lab Med. 2008. 132:1907–1911.15. Williams MD, Roberts DB, Kies MS, Mao L, Weber RS, El-Naggar AK. Genetic and expression analysis of HER-2 and EGFR genes in salivary duct carcinoma: empirical and therapeutic significance. Clin Cancer Res. 2010. 16:2266–2274.16. Ettl T, Schwarz S, Kleinsasser N, Hartmann A, Reichert TE, Driemel O. Overexpression of EGFR and absence of C-KIT expression correlate with poor prognosis in salivary gland carcinomas. Histopathology. 2008. 53:567–577.17. Han H, Silverman JF, Santucci TS, Macherey RS, d'Amato TA, Tung MY, Weyant RJ, Landreneau RJ. Vascular endothelial growth factor expression in stage I non-small cell lung cancer correlates with neoangiogenesis and a poor prognosis. Ann Surg Oncol. 2001. 8:72–79.18. Mori Y, Tsukinoki K, Yasuda M, Miyazawa M, Kaneko A, Watanabe Y. Glucose transporter type 1 expression are associated with poor prognosis in patients with salivary gland tumors. Oral Oncol. 2007. 43:563–569.19. Gnepp DR, Brandwein-Gensler MS, El-Naggar AK, Nagao T. Barnes L, Eveson JW, Reichart P, Sidransky D, editors. Carcinoma ex pleomorphic adenoma. Pathology and genetics of head and neck tumours. 2005. Lyon: IARC;242–243.20. Sato M, Hayashi Y, Yoshida H, Yanagawa T, Yura Y, Nitta T. Search for specific markers of neoplastic epithelial duct and myoepithelial cell lines established from human salivary gland and characterization of their growth in vitro. Cancer. 1984. 54:2959–2967.21. Savera AT, Sloman A, Huvos AG, Klimstra DS. Myoepithelial carcinoma of the salivary glands: a clinicopathologic study of 25 patients. Am J Surg Pathol. 2000. 24:761–774.22. Deguchi H, Hamano H, Hayashi Y. c-myc, ras p21 and p53 expression in pleomorphic adenoma and its malignant form of the human salivary glands. Acta Pathol Jpn. 1993. 43:413–422.23. Yamamoto Y, Kishimoto Y, Wistuba II, Virmani AK, Vuitch F, Gazdar AF, Albores-Saavedra J. DNA analysis at p53 locus in carcinomas arising from pleomorphic adenomas of salivary glands: comparison of molecular study and p53 immunostaining. Pathol Int. 1998. 48:265–272.24. Müller S, Vigneswaran N, Gansler T, Gramlich T, DeRose PB, Cohen C. c-erbB-2 oncoprotein expression and amplification in pleomorphic adenoma and carcinoma ex pleomorphic adenoma: relationship to prognosis. Mod Pathol. 1994. 7:628–632.25. Nagler RM, Kerner H, Ben-Eliezer S, Minkov I, Ben-Itzhak O. Prognostic role of apoptotic, Bcl-2, c-erbB-2 and p53 tumor markers in salivary gland malignancies. Oncology. 2003. 64:389–398.26. Sugano S, Mukai K, Tsuda H, Hirohashi S, Furuya S, Shimosato Y, Ebihara S, Takeyama I. Immunohistochemical study of c-erbB-2 oncoprotein overexpression in human major salivary gland carcinoma: an indicator of aggressiveness. Laryngoscope. 1992. 102:923–927.27. Sharon E, Kelly RJ, Szabo E. Sustained response of carcinoma ex pleomorphic adenoma treated with trastuzumab and capecitabine. Head Neck Oncol. 2010. 2:12.28. Swelam W, Ida-Yonemochi H, Maruyama S, Ohshiro K, Cheng J, Saku T. Vascular endothelial growth factor in salivary pleomorphic adenomas: one of the reasons for their poorly vascularized stroma. Virchows Arch. 2005. 446:653–662.29. Andreadis D, Epivatianos A, Poulopoulos A, Nomikos A, Papazoglou G, Antoniades D, Barbatis C. Detection of C-KIT (CD117) molecule in benign and malignant salivary gland tumours. Oral Oncol. 2006. 42:57–65.30. Horiuchi C, Tsukuda M, Taguchi T, Ishiguro Y, Okudera K, Inoue T. Correlation between FDG-PET findings and GLUT1 expression in salivary gland pleomorphic adenomas. Ann Nucl Med. 2008. 22:693–698.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pleomorphic adenoma of the cheek in the young patient: report of a case
- A Case of Pleomorphic Adenoma on the Upper Lip
- A Case of Multiple Cutaneous Metastases from Metastasizing PleomorphicAdenoma of the Submandibular Gland
- A Case of Carcinoma Ex Pleomorphic Adenoma in the Maxillary Sinus
- A Case of Salivary Duct Carcinoma Ex Pleomorphic Adenoma of Parotid Gland