J Korean Med Sci.
2011 Jun;26(6):844-847. 10.3346/jkms.2011.26.6.844.
Atypical Supernumerary Phantom Limb and Phantom Limb Pain in Two Patients with Pontine Hemorrhage
- Affiliations
-
- 1Department of Physical Medicine & Rehabilitation, College of Medicine Kyung Hee University, Seoul, Korea. pure0111@hotmail.com
- KMID: 1785976
- DOI: http://doi.org/10.3346/jkms.2011.26.6.844
Abstract
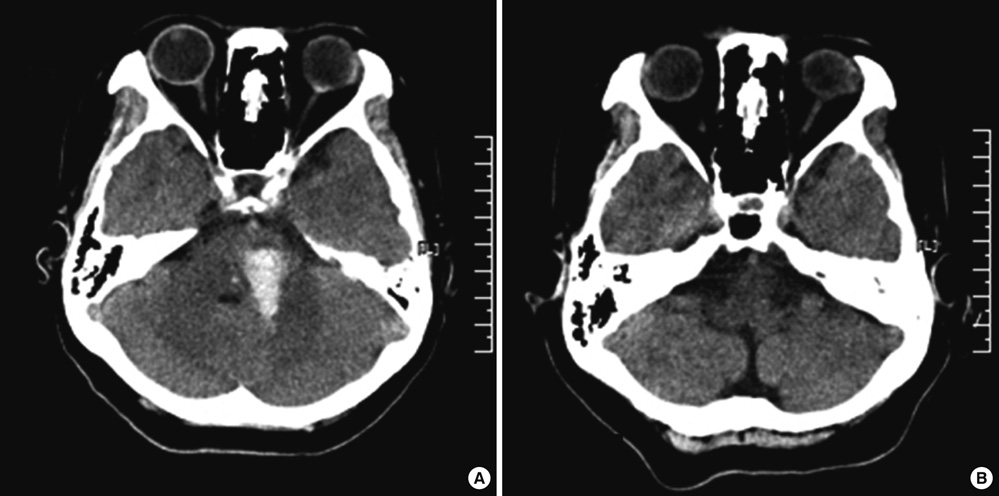
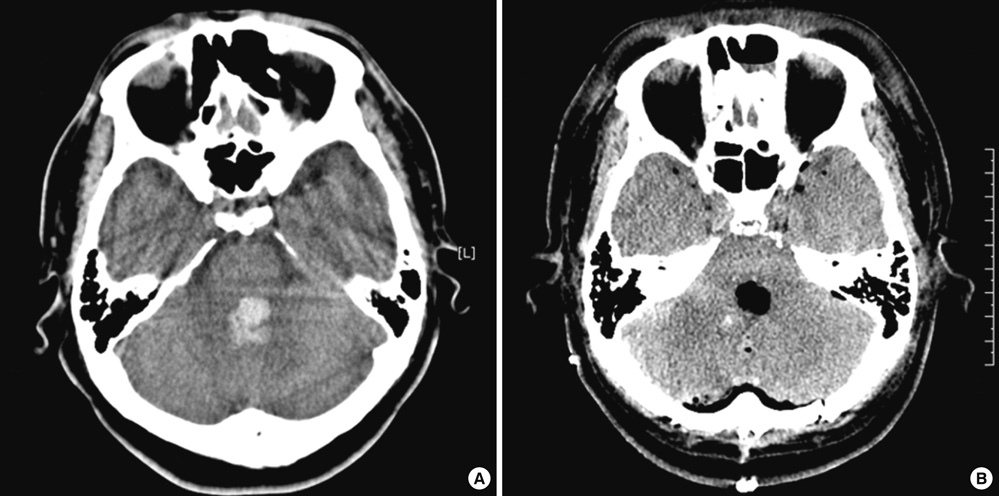
- Phantom limbs are usually observed after amputation of extremities. In patients after a stroke, a similar but rarely occurring phenomenon consisting of the patient experiencing the presence of an additional limb has been described. This phenomenon, generally called supernumerary phantom limb (SPL), may be caused by lesions in the right or left cerebral hemisphere, but has been predominantly reported in patients who have had a right hemispheric stroke. We report two cases of atypical SPL and phantom limb pain (PLP) after pontine hemorrhage. The patients were treated conservatively and their symptoms lasted more than 1 month. This is the first report of SPLs after left pontine hemorrhage, and phantom perception and pain lasted longer than those in previously observed cases. Our results indicate that SPL may be more common than reported; therefore, thorough examinations are essential for the care of stroke patients.
MeSH Terms
Figure
Reference
-
1. Srivastava A, Taly AB, Gupta A, Murali T, Noone ML, Thirthahalli J, Gangadhar BN, Kumar JK, Jayakumar PN. Stroke with supernumerary phantom limb: case study, review of literature and pathogenesis. Acta Neuropsychiatr. 2008. 20:256–264.2. McGlynn SM, Schacter DL. Unawareness of deficits in neuropsychological syndromes. J Clin Exp Neuropsychol. 1989. 11:143–205.3. Brion S, Jedynak CP. Disorders of interhemispheric transfer (callosal disonnection). 3 cases of tumor of the corpus callosum. The strange hand sign. Rev Neurol (Paris). 1972. 126:257–266.4. Critichley M. The parietal lobes. 1953. New York: Hafner;243–244.5. Melzack R. Phantom limbs and the concept of a neuromatrix. Trends Neurosci. 1990. 13:88–92.6. Fredericks J. FREDERICKS J, editor. Phantom limb and phantom limb pain. Handbook of clinical neurology. 1985. Vol. 1. Amsterdam: Elsiever;373–393.7. Cutting J. Reynolds E, Trimble M, editors. Body image disturbances in neuropsychiatry. The bridge between neurology and psychiatry. 1989. Edinburgh: Churchill Livingstone.8. Miyazawa N, Hayashi M, Komiya K, Akiyama I. Supernumerary phantom limbs associated with left hemisphere stroke: case report and review of the literature. Neurosurgery. 2004. 54:228–231.9. Frederiks JA. Occurrence and nature of phantom limb phenomena following amputation of body parts and following lesions of the central and peripheral nervous system. Psychiatr Neurol Neurochir. 1963. 66:73–97.10. Canavero S, Bonicalzi V, Castellano G, Perozzo P, Massa-Micon B. Painful supernumerary phantom arm following motor cortex stimulation for central poststroke pain. Case report. J Neurosurg. 1999. 91:121–123.11. Canavero S. Dynamic reverberation. A unified mechanism for central and phantom pain. Med Hypotheses. 1994. 42:203–207.12. Fisher K, Hanspal RS. Phantom pain, anxiety, depression, and their relation in consecutive patients with amputated limbs: case reports. BMJ. 1998. 316:903–904.13. Halligan PW, Marshall JC, Wade DT. Three arms: a case study of supernumerary phantom limb after right hemisphere stroke. J Neurol Neurosurg Psychiatry. 1993. 56:159–166.14. Halligan PW, Marshall JC. Supernumerary phantom limb after right hemispheric stroke. J Neurol Neurosurg Psychiatry. 1995. 59:341–342.15. McGonigle DJ, Hänninen R, Salenius S, Hari R, Frackowiak RS, Frith CD. Whose arm is it anyway? An fMRI case study of supernumerary phantom limb. Brain. 2002. 125:1265–1274.16. Donnet A, Schmitt A, Poncet M, Graziani N, Grisoli F. Hallucinations of supernumerary limbs, left hemineglect and hypersexuality in a case of right capsulo-lenticular hematoma. Rev Neurol (Paris). 1997. 153:587–590.17. Nasreddine ZS, Saver JL. Pain after thalamic stroke: right diencephalic predominance and clinical features in 180 patients. Neurology. 1997. 48:1196–1199.18. Bogaert LV. Sur la pathologie de l'image de soi. Ann Med Psychol. 1934. 92:519–536.19. Pinéas H. Ein Fall von phantomähnlichen Erscheinungen ("Phantomarm") bei hemiplegischer Lähmung. Nervenarzt. 1932. 5:233–236.20. Antoniello D, Kluger BM, Sahlein DH, Heilman KM. Phantom limb after stroke: an underreported phenomenon. Cortex. 2009. 46:1114–1122.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Letter to the Editor: The Supernumerary Phantom Limb and Phantom Limb Pain-Important Facts
- Mirror Therapy for Phantom Limb Pain
- The Author Response: The Supernumerary Phantom Limb and Phantom Limb Pain in Stroke: Localization and Management Concerns
- Effect of Epidural Block with Meperidine in Patient with Phantom Limb Pain: A case report
- Phantom Phenomena in Traumatic Amputation