Neurointervention.
2011 Aug;6(2):78-83. 10.5469/neuroint.2011.6.2.78.
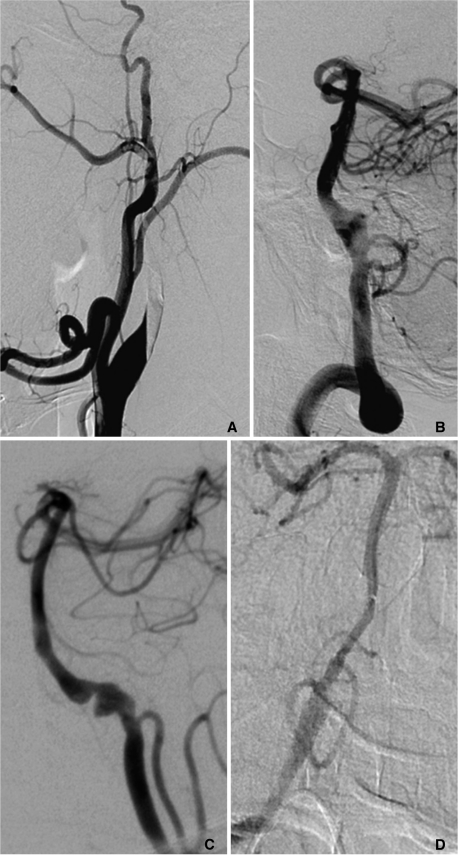
Cerebral Artery Dissection: Spectrum of Clinical Presentations Related to Angiographic Findings
- Affiliations
-
- 1Department of Radiology and Research Institute of Radiology, University of Ulsan, College of Medicine, Asan Medical Center, Seoul, Korea. dcsuh@amc.seoul.kr
- 2Department of Internal Medicine, University of Ulsan, College of Medicine, Asan Medical Center, Seoul, Korea.
- 3Department of Radiology, Konkuk University College of Medicine, Seoul 143-729, Korea.
- KMID: 1783987
- DOI: http://doi.org/10.5469/neuroint.2011.6.2.78
Abstract
- PURPOSE
Cerebral arterial dissections are recognized as a common cause of stroke. However, few studies have reported on the distribution of cerebral arterial dissection and angiographic pattern related to the presenting clinical symptom pattern. We analyzed the distribution of cerebral artery dissection along with angiographic and clinical presenting a pattern as depicted on angiograms.
MATERIALS AND METHODS
From January 2000 to January 2007, 133 arterial dissection patients admitted to our institutes were retrospectively reviewed. The characteristic angiographic findings of all cerebral arteries were carefully evaluated on 4-vessel angiograms. The male-female ratio was 77: 56 and the mean age was 51 years. According to the angiographic finding depicting the location of the dissection plane in the arterial wall, we categorized to steno-occlusive, aneurysmal, combined and unclassifiable pattern. In each dissection pattern, we evaluated presenting symptoms and presence of infarction or hemorrhage.
RESULTS
The most common symptom on presentation was headache (47%), followed by motor weakness of arm or leg (31%), dysarthria/aphasia (19%) and vertigo (16%). The most common angiographic pattern was steno-occlusive (46%), followed by combined (steno-occlusive and aneurismal) (27%) and aneurysmal (22%) patterns. Steno-occlusive pattern was most commonly related to infarction (33/61, 54%) in contrast that aneurysmal pattern was most frequently related to subarachnoid hemorrhage (SAH) (7/29, 24%). The most frequent abnormality in patients with dissection of the intradural vertebral arteries including posterior cerebral artery (PCA) was SAH (23/70, 33%), followed by infarction. Infarction was the most common abnormality in patients with the extradural and intradural carotid arteries, and the extradural vertebral artery.
CONCLUSION
In contrast that the extradural arterial dissections tended to result in ischemia with steno-occlusive pattern, the intradural arterial dissections tended to result in SAH with aneurysmal type, especially in the vertebral artery. Dissection requires combined analysis of angiographic pattern and type of stroke depending on the location.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Clinical Manifestation and Radiologic Patterns of Spontaneous Cervicocephalic Dissection According to the Anatomic Location: A Single-Center Analysis in Korean Patients
Yunsun Song, Sang Ik Park, Pepi Budianto, Boseong Kwon, Dae Chul Suh
Neurointervention. 2022;17(2):78-86. doi: 10.5469/neuroint.2022.00143.
Reference
-
1. Ducrocq X, Lacour JC, Debouverie M, Bracard S, Girard F, Weber M. Accidents vasculaares cérébraux ischémiques du sujet jeune. Étude prospective de 296 patients âgés de 16 à 45 ans. Rev Neurol. 1999; 155:575–582. PMID: 10486847.3. Krings T, Choi IS. The many faces of intracranial arterial dissections. Interv Neuroradiol. 2010; 16:151–160. PMID: 20642889.
Article4. Shin JH, Suh DC, Choi CG, Leei HK. Vertebral artery dissection: spectrum of imaging findings with emphasis on angiography and correlation with clinical presentation. Radiographics. 2000; 20:1687–1696. PMID: 11112824.
Article5. Hart RG, Easton JD. Dissections of cervical and cerebral arteries. Neurol Clin. 1983; 1:155–182. PMID: 6680158.
Article6. Touzé E, Randoux B, Méary E, Arquizan C, Meder JF, Mas JL. Aneurysmal forms of cervical artery dissection : associated factors and outcome. Stroke. 2001; 32:418–423. PMID: 11157176.7. Li S, Yan B, Kaye A, Mitchell P, Dowling R, Collins M, et al. Prognosis of intracranial dissection relates to site and presenting features. J Clin Neurosci. 2011; 18:789–793. PMID: 21507658.
Article8. Silbert PL, Mokri B, Schievink WI. Headache and neck pain in spontaneous internal carotid and vertebral artery dissections. Neurology. 1995; 45:1517–1522. PMID: 7644051.
Article9. Bogousslavsky J, Regli F. Ischemic stroke in adults younger than 30 years of age. Cause and prognosis. Arch Neurol. 1987; 44:479–482. PMID: 3579657.10. Lucas C, Moulin T, Deplanque D, Tatu L, Chavot D. Stroke patterns of internal carotid artery dissection in 40 patients. Stroke. 1998; 29:2646–2648. PMID: 9836779.
Article11. Strong KC. A study of the structure of the media of the distributing arteries by the method of microdissection. The Anatomical Record. 1938; 72:151–167.
Article12. Kocaeli H, Chaalala C, Andaluz N, Zuccarello M. Spontaneous intradural vertebral artery dissection: a single-center experience and review of the literature. Skull Base. 2009; 19:209–218. PMID: 19881901.
Article13. Jang YG, Ryu CW, Kim JS, Cha EY, Pyun HW, Kim DY, et al. Dissecting aneurysm of the basilar arterial trunk presenting with pontine infarction: coil obliteration of the dissecting aneurysm including the diseased basilar arterial segment. Interv Neuroradiol. 2007; 13:381–384. PMID: 20566107.14. Mizutani T, Miki Y, Kojima H, Suzuki H. Proposed classification of nonatherosclerotic cerebral fusiform and dissecting aneurysms. Neurosurgery. 1999; 45:253–259. PMID: 10449069.
Article15. In HS, Lee HY, Park JY, Kim SY, Jung JH, Kim JS, et al. Intracranial stenting in patients with atherosclerotic stenosis associated with various aneurysms in the same diseased arterial segment. AJNR Am J Neuroradiol. 2010; 31:1895–1898. PMID: 20671060.
Article16. Yonas H, Agamanolis D, Takaoka Y, White RJ. Dissecting intracranial aneurysms. Surg Neurol. 1977; 8:407–415. PMID: 594878.17. Yamada SM, Nakane M, Aoki M, Nakayama H. Dissecting aneurysm of the anterior cerebral artery with severe subarachnoid hemorrhage during treatment for cerebral infarction. Intern Med. 2003; 42:433–435. PMID: 12793716.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Reversible Cerebral Vasoconstriction Syndrome with Concurrent Anterior Cerebral Artery Dissection
- Angiographic Analysis of Middle Cerebral Artery Bifurcation Aneurysm
- Post-Traumatic Middle Cerebral Artery Dissection: A Case Report
- A Case bilateral Persistent Primitive Trigeminal Artery Combined with Cerebral Rete Mirabile
- Two Cases of Cerebral Infarctions from Vertebral Artery Dissection Induced by Severe Coughing