J Periodontal Implant Sci.
2012 Aug;42(4):127-135. 10.5051/jpis.2012.42.4.127.
Clinical evaluation of a biphasic calcium phosphate grafting material in the treatment of human periodontal intrabony defects
- Affiliations
-
- 1Department of Periodontology, Chosun University School of Dentistry, Gwangju, Korea. sjyu78@chosun.ac.kr
- KMID: 1783648
- DOI: http://doi.org/10.5051/jpis.2012.42.4.127
Abstract
- PURPOSE
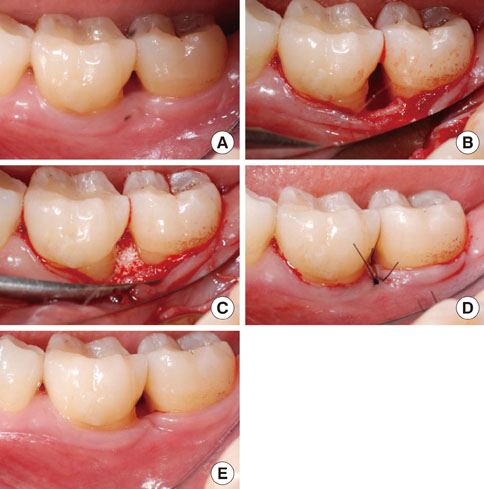
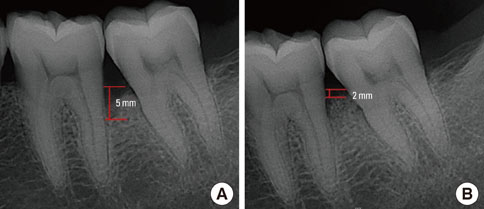
The aim of this study was to compare the clinical outcome of open flap debridement (OFD) with a biphasic calcium phosphate (BCP) graft to that of OFD without BCP graft for the treatment of intrabony periodontal defects (IBDs).
METHODS
The study included 25 subjects that had at least one intrabony defect of 2- or 3-wall morphology and an intrabony component> or =4 mm as detected radiographically. Subjects were randomly assigned to treatment with (BCP group, n=14) or without BCP (OFD group, n=11). Clinical parameters were recorded at baseline and 6 months after surgery and included the plaque index, gingival index, probing depth (PD), clinical attachment level (CAL), and gingival recession (REC). A stringent plaque control regimen was enforced for all of the patients during the 6-month observation period.
RESULTS
In all of the treatment groups, significant PD reductions and CAL gains occurred during the study period (P<0.01). At 6 months, patients in the BCP group exhibited a mean PD reduction of 3.7+/-1.2 mm and a mean CAL gain of 3.0+/-1.1 mm compared to the baseline. Corresponding values for the patients treated with OFD were 2.5+/-0.8 mm and 1.4+/-1.0 mm, respectively. Compared to OFD group, the additional CAL gain was significantly greater in the patients in BCP group (P=0.028). The additional PD reduction was significant for the BCP group (P=0.048). The REC showed a significant increase in both groups, and the amount of recession was significantly smaller in the BCP group than OFD group (P=0.023). In radiographic evaluation, the height of the bone fill in the BCP group was significantly greater than OFD group.
CONCLUSIONS
The clinical benefits of BCP found in this study indicate that BCP may be an appropriate alternative to conventional graft materials.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Dental alloplastic bone substitutes currently available in Korea
Jeong-Kui Ku, Inseok Hong, Bu-Kyu Lee, Pil-Young Yun, Jeong Keun Lee
J Korean Assoc Oral Maxillofac Surg. 2019;45(2):51-67. doi: 10.5125/jkaoms.2019.45.2.51.Regenerative potential of biphasic calcium phosphate and enamel matrix derivatives in the treatment of isolated interproximal intrabony defects: a randomized controlled trial
Pritish Chandra Pal, Ashish Bali, Ramanarayana Boyapati, Sangita Show, Kanikanti Siva Tejaswi, Sourabh Khandelwal
J Yeungnam Med Sci. 2022;39(4):322-331. doi: 10.12701/jyms.2022.00325.
Reference
-
1. Tonetti MS, Prato GP, Cortellini P. Factors affecting the healing response of intrabony defects following guided tissue regeneration and access flap surgery. J Clin Periodontol. 1996. 23:548–556.
Article2. Machtei EE. The effect of membrane exposure on the outcome of regenerative procedures in humans: a meta-analysis. J Periodontol. 2001. 72:512–516.
Article3. Stahl SS, Froum SJ, Kushner L. Healing responses of human intraosseous lesions following the use of debridement, grafting and citric acid root treatment. II. Clinical and histologic observations: one year postsurgery. J Periodontol. 1983. 54:325–338.
Article4. Froum SJ, Kushner L, Stahl SS. Healing responses of human intraosseous lesions following the use of debridement, grafting and citric acid root treatment. I. Clinical and histologic observations six months postsurgery. J Periodontol. 1983. 54:67–76.
Article5. Bowers GM, Chadroff B, Carnevale R, Mellonig J, Corio R, Emerson J, et al. Histologic evaluation of new attachment apparatus formation in humans. Part II. J Periodontol. 1989. 60:675–682.
Article6. Camelo M, Nevins ML, Schenk RK, Simion M, Rasperini G, Lynch SE, et al. Clinical, radiographic, and histologic evaluation of human periodontal defects treated with Bio-Oss and Bio-Gide. Int J Periodontics Restorative Dent. 1998. 18:321–331.
Article7. Camargo PM, Lekovic V, Weinlaender M, Nedic M, Vasilic N, Wolinsky LE, et al. A controlled re-entry study on the effectiveness of bovine porous bone mineral used in combination with a collagen membrane of porcine origin in the treatment of intrabony defects in humans. J Clin Periodontol. 2000. 27:889–896.
Article8. Caplanis N, Lee MB, Zimmerman GJ, Selvig KA, Wikesjo UM. Effect of allogeneic freeze-dried demineralized bone matrix on regeneration of alveolar bone and periodontal attachment in dogs. J Clin Periodontol. 1998. 25:801–806.
Article9. Yildirim M, Spiekermann H, Biesterfeld S, Edelhoff D. Maxillary sinus augmentation using xenogenic bone substitute material Bio-Oss in combination with venous blood. A histologic and histomorphometric study in humans. Clin Oral Implants Res. 2000. 11:217–229.
Article10. Sartori S, Silvestri M, Forni F, Icaro Cornaglia A, Tesei P, Cattaneo V. Ten-year follow-up in a maxillary sinus augmentation using anorganic bovine bone (Bio-Oss). A case report with histomorphometric evaluation. Clin Oral Implants Res. 2003. 14:369–372.
Article11. Dori F, Arweiler N, Gera I, Sculean A. Clinical evaluation of an enamel matrix protein derivative combined with either a natural bone mineral or beta-tricalcium phosphate. J Periodontol. 2005. 76:2236–2243.
Article12. Kim SK, Choi EH, Lee JS, Kim TG, Choi SH, Cho KS, et al. Evaluating intra- and inter-examiner reproducibility in histometric measurement: one-wall intrabony periodontal defects in beagle dogs. J Periodontal Implant Sci. 2010. 40:172–179.
Article13. Yukna RA, Harrison BG, Caudill RF, Evans GH, Mayer ET, Miller S. Evaluation of durapatite ceramic as an alloplastic implant in periodontal osseous defects. II. Twelve month reentry results. J Periodontol. 1985. 56:540–547.
Article14. Nery EB, LeGeros RZ, Lynch KL, Lee K. Tissue response to biphasic calcium phosphate ceramic with different ratios of HA/beta TCP in periodontal osseous defects. J Periodontol. 1992. 63:729–735.
Article15. Loe H. The gingival index, the plaque index and the retention index systems. J Periodontol. 1967. 38:Suppl:610–Suppl:616.
Article16. Wang HL, Burgett FG, Shyr Y, Ramfjord S. The influence of molar furcation involvement and mobility on future clinical periodontal attachment loss. J Periodontol. 1994. 65:25–29.
Article17. Cortellini P, Prato GP, Tonetti MS. The simplified papilla preservation flap. A novel surgical approach for the management of soft tissues in regenerative procedures. Int J Periodontics Restorative Dent. 1999. 19:589–599.
Article18. Cortellini P, Prato GP, Tonetti MS. The modified papilla preservation technique. A new surgical approach for interproximal regenerative procedures. J Periodontol. 1995. 66:261–266.
Article19. Pradeep AR, Thorat MS. Clinical effect of subgingivally delivered simvastatin in the treatment of patients with chronic periodontitis: a randomized clinical trial. J Periodontol. 2010. 81:214–222.20. Nasr HF, Aichelmann-Reidy ME, Yukna RA. Bone and bone substitutes. Periodontol 2000. 1999. 19:74–86.21. Hanes PJ. Bone replacement grafts for the treatment of periodontal intrabony defects. Oral Maxillofac Surg Clin North Am. 2007. 19:499–512. vi
Article22. Froum SJ, Ortiz M, Witkin RT, Thaler R, Scopp IW, Stahl SS. Osseous autografts III Comparison of osseous coagulum-bone blend implants with open curetage. J Periodontol. 1976. 47:287–294.
Article23. Daculsi G, LeGeros RZ, Nery E, Lynch K, Kerebel B. Transformation of biphasic calcium phosphate ceramics in vivo: ultrastructural and physicochemical characterization. J Biomed Mater Res. 1989. 23:883–894.
Article24. Zaner DJ, Yukna RA. Particle size of periodontal bone grafting materials. J Periodontol. 1984. 55:406–409.
Article25. Galgut PN, Waite IM, Brookshaw JD, Kingston CP. A 4-year controlled clinical study into the use of a ceramic hydroxylapatite implant material for the treatment of periodontal bone defects. J Clin Periodontol. 1992. 19:570–577.
Article26. Yukna RA, Callan DP, Krauser JT, Evans GH, Aichelmann-Reidy ME, Moore K, et al. Multi-center clinical evaluation of combination anorganic bovine-derived hydroxyapatite matrix (ABM)/cell binding peptide (P-15) as a bone replacement graft material in human periodontal osseous defects. 6-month results. J Periodontol. 1998. 69:655–663.
Article27. Kasaj A, Rohrig B, Zafiropoulos GG, Willershausen B. Clinical evaluation of nanocrystalline hydroxyapatite paste in the treatment of human periodontal bony defects--a randomized controlled clinical trial: 6-month results. J Periodontol. 2008. 79:394–400.
Article28. Froum SJ, Weinberg MA, Tarnow D. Comparison of bioactive glass synthetic bone graft particles and open debridement in the treatment of human periodontal defects. A clinical study. J Periodontol. 1998. 69:698–709.
Article29. Nevins ML, Camelo M, Nevins M, King CJ, Oringer RJ, Schenk RK, et al. Human histologic evaluation of bioactive ceramic in the treatment of periodontal osseous defects. Int J Periodontics Restorative Dent. 2000. 20:458–467.
Article30. Kim CK, Kim HY, Chai JK, Cho KS, Moon IS, Choi SH, et al. Effect of a calcium sulfate implant with calcium sulfate barrier on periodontal healing in 3-wall intrabony defects in dogs. J Periodontol. 1998. 69:982–988.
Article31. Laurell L, Gottlow J, Zybutz M, Persson R. Treatment of intrabony defects by different surgical procedures. A literature review. J Periodontol. 1998. 69:303–313.
Article32. Zafiropoulos GG, Hoffmann O, Kasaj A, Willershausen B, Weiss O, Van Dyke TE. Treatment of intrabony defects using guided tissue regeneration and autogenous spongiosa alone or combined with hydroxyapatite/beta-tricalcium phosphate bone substitute or bovine-derived xenograft. J Periodontol. 2007. 78:2216–2225.
Article33. Stein JM, Fickl S, Yekta SS, Hoischen U, Ocklenburg C, Smeets R. Clinical evaluation of a biphasic calcium composite grafting material in the treatment of human periodontal intrabony defects: a 12-month randomized controlled clinical trial. J Periodontol. 2009. 80:1774–1782.
Article34. Rosen PS, Reynolds MA, Bowers GM. The treatment of intrabony defects with bone grafts. Periodontol 2000. 2000. 22:88–103.
Article35. Dybvik T, Leknes KN, Boe OE, Skavland RJ, Albandar JM. Bioactive ceramic filler in the treatment of severe osseous defects: 12-month results. J Periodontol. 2007. 78:403–410.
Article36. Shirakata Y, Setoguchi T, Machigashira M, Matsuyama T, Furuichi Y, Hasegawa K, et al. Comparison of injectable calcium phosphate bone cement grafting and open flap debridement in periodontal intrabony defects: a randomized clinical trial. J Periodontol. 2008. 79:25–32.
Article37. Ellegaard B, Löe H. New attachment of periodontal tissues after treatment of intrabony lesions. J Periodontol. 1971. 42:648–652.
Article38. Hiatt WH, Schallhorn RG. Intraoral transplants of cancellous bone and marrow in periodontal lesions. J Periodontol. 1973. 44:194–208.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Histometrical evaluation of biphasic calcium phosphate in surgically created 1-wall periodontal intrabony defects in dogs
- Histologic evaluation of macroporous biphasic calcium phosphate(MBCP(R)) and flouorohydrxyapatite(Algipore(R)) in surgically created 1-wall periodontal intrabony defects of minipigs
- The Effect of Calcium Sulfate on the Periodontal Healing of 2-Wall Intrabony Defects in Dogs
- The Effect of Recombinant Human Bone Morphogenetic Protein-2/Macroporous Biphasic Calcium Phosphate Block system on Bone Formation in Rat Calvarial Defects
- Maxillary Sinus Augmentation Using Macroporous Biphasic Calcium Phosphate (MBCP(TM)): Three Case Report With Histologic Evaluation