J Korean Med Sci.
2009 Dec;24(6):1071-1077. 10.3346/jkms.2009.24.6.1071.
Endocrine Complications after Hematopoietic Stem Cell Transplantation during Childhood and Adolescence
- Affiliations
-
- 1Department of Pediatrics, College of Medicine, The Catholic University of Korea, Seoul, Korea. chobinkr@catholic.ac.kr
- KMID: 1783135
- DOI: http://doi.org/10.3346/jkms.2009.24.6.1071
Abstract
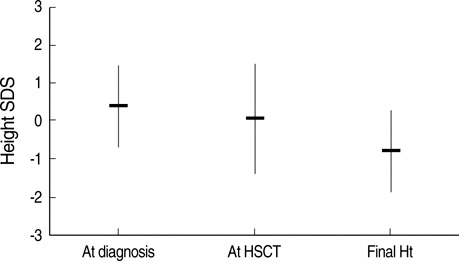
- Long-term survivors of hematopoietic stem cell transplantation (HSCT) during childhood and adolescence are at risk of developing endocrine complications. The purpose of this study was to evaluate the long-term endocrine complications and their associated risk factors among such patients. We reviewed the data from 111 patients (59 males and 52 females) who underwent HSCT at the mean age of 8.3+/-4.1 yr. Thirty patients (27.0%) had growth impairment, and seven (21.2%) out of 33 patients who attained final height reached final height below 2 standard deviation (SD). The final height SD score of the patients conditioned with total body irradiation (TBI) was significantly lower than that of the patients conditioned without TBI (-1.18+/-1.14 vs. -0.19+/-0.78, P=0.011). Thirteen patients (11.7%) developed hypothyroidism (11 subclinical, 2 central) 3.8+/-1.8 (range 1.6-6.2) yr after HSCT. Nineteen (65.5%) out of 29 females had evidence of gonadal dysfunction, and 18 (64.3%) out of 28 males had evidence of gonadal dysfunction. The risk for gonadal dysfunction was significantly higher in females conditioned with busulfan/cyclophosphamide (P=0.003). These results suggest that the majority of patients treated with HSCT during childhood and adolescence have one or more endocrine complications. Therefore, multiple endocrine functions should be monitored periodically after HSCT until they reach adult age.
Keyword
MeSH Terms
-
Adolescent
Adult
Body Height
Child
Child, Preschool
Endocrine System Diseases/*etiology/physiopathology
Female
Gonadal Disorders/etiology
Growth Disorders/etiology
Hematopoietic Stem Cell Transplantation/*adverse effects
Humans
Infant
Male
Thyroid Diseases/etiology
Transplantation Conditioning/adverse effects
Whole-Body Irradiation/adverse effects
Figure
Reference
-
1. Thomas ED. History of haemopoietic cell transplantation. Br J Haematol. 1999. 105:330–339.2. Goldman JM, Schmitz N, Niethammer D, Gratwohl A. Allogeneic and autologous transplantation for haematological disease, solid tumors and immune disorders: current practice in Europe in 1998. Accreditation Sub-Committee of the European Group for Blood and Marrow Transplantation. Bone Marrow Transplant. 1998. 21:1–7.3. Hows JM, Passweg JR, Tichelli A, Locasciulli A, Szydlo R, Bacigalupo A, Jacobson N, Ljungman P, Cornish J, Nunn A, Bradley B, Socié G. IMUST Study Participating Centers. Late Effects Working Party of the European Group for Blood and Marrow Transplantation (EBMT). Comparison of long-term outcomes after allogeneic hematopoietic stem cell transplantation from matched sibling and unrelated donors. Bone Marrow Transplant. 2006. 38:799–805.
Article4. Mayer EI, Dopfer RE, Klingebiel T, Scheel-Walter H, Ranke MB, Niethammer D. Longitudinal gonadal function after bone marrow transplantation for acute lymphoblastic leukemia during childhood. Pediatr Transplant. 1999. 3:38–44.
Article5. Moon JS, Lee SY, Nam CM, Choi JM, Choe BK, Seo JW, Oh K, Jang MJ, Hwang SS, Yoo MH, Kim YT, Lee CG. 2007 Korean National Growth Charts: review of developmental process and outlook. Korean J Pediatr. 2008. 51:1–25.6. Tanner JM, Whitehouse RH. Clinical longitudinal standards for Ht, weight, Ht velocity, and stages of puberty. Arch Dis Child. 1976. 51:170–179.7. Greulich WW, Pyle SI. Radiograhic atlas of skeletal development of the hand and wrist. 1959. 2nd ed. Stanford: Stanford University Press.8. Shalitin S, Phillip M, Stein J, Goshen Y, Carmi D, Yaniv I. Endocrine dysfunction and parameters of the metabolic syndrome after bone marrow transplantation during childhood and adolescence. Bone Marrow Transplant. 2006. 37:1109–1117.
Article9. Berger C, Le-Gallo B, Donadieu J, Richard O, Devergie A, Galambrun C, Bordigoni P, Vilmer E, Plouvier E, Perel Y, Michel G, Stephan JL. Late thyroid toxicity in 13 long-term survivors of allogeneic bone marrow transplantation for acute lymphoblastic leukemia. Bone Marrow Transplant. 2005. 35:991–995.10. Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, Gordon DJ, Krauss RM, Savage PJ, Smith SC Jr, Spertus JA, Costa F. American Heart Association. National Heart, Lung, and Blood Institute. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Insititute Scientific Statement. Circulation. 2005. 112:2735–2752.11. Mayer EI, Dopfer RE, Klingebiel T, Scheel-Walter H, Ranke MB, Niethammer D. Longitudinal gonadal function after bone marrow transplantation for acute lymphoblastic leukemia during childhood. Pediatr Transplant. 1999. 3:38–44.
Article12. Chemaitilly W, Sklar CA. Endocrine complications of hematopoietic stem cell transplantation. Endocrinol Metab Clin North Am. 2007. 36:983–998.
Article13. Cohen A, Rovelli A, Bakker B, Uderzo C, van Lint MT, Esperou H, Gaiero A, Leiper AD, Dopfer R, Cahn JY, Merlo F, Kolb HJ, Socié G. Final height of patients who underwent bone marrow transplantation for hematological disorders during childhood: a study by the Working Party for Late Effects-EBMT. Blood. 1999. 93:4109–4115.14. Clement-De Boers A, Oostdijk W, Van Weel-Sipman MH, Van den Broeck J, Wit JM, Vossen JM. Final height and hormonal function after bone marrow transplantation in children. J Pediatr. 1996. 129:544–550.15. Brennan BM, Shalet MS. Endocrine late effects after bone marrow transplantation. Br J Haematol. 2002. 118:58–66.16. Chemaitilly W, Boulad F, Heller G, Kernan NA, Small TN, O'Reilly RJ, Sklar CA. Final height in pediatric patients after hyperfractionated total body irradiation and stem cell transplantation. Bone Marrow Transplant. 2007. 40:29–35.
Article17. Bakker B, Oostdijk W, Geskus RB, Stokvis-Brantsma WH, Vossen JM, Wit JM. Patterns of growth and body proportion after total body irradiation and hematopoietic stem cell transplantation during childhood. Pediatr Res. 2006. 59:259–264.18. Sanders JE, Guthrie KA, Hoffmeister PA, Woolfrey AE, Carpenter PA, Appelbaum FR. Final adult height of patients who received hematopoietic cell transplantation in childhood. Blood. 2005. 105:1348–1354.
Article19. Holm K, Nysom K, Rasmussen MH, Hertz H, Jacobsen N, Skakkebaek NE, Krabbe S, Müsller J. Growth, growth hormone and final height after BMT. Possible recovery of irradiation-induced growth hormone insufficiency. Bone Marrow Transplant. 1996. 18:163–170.20. Ogilvy-Stuart AL, Clark DJ, Wallace WH, Gibson BE, Stevens RF, Shalet SM, Donaldson MD. Endocrine deficit after fractionated total body irradiation. Arch Dis Child. 1992. 67:1107–1110.
Article21. Couto-Silva AC, Trivin C, Esperou H, Michon J, Fischer A, Brauner R. Changes in height, weight and plasma leptin after bone marrow transplantation. Bone Marrow Transplant. 2000. 26:1205–1210.
Article22. Glatstein E, McHardy-Young S, Brast N, Eltringham JR, Kriss JP. Alterations in serum thyrotropin (TSH) and thyroid function following radiotherapy in patients with malignant lymphoma. J Clin Endocrinol Metab. 1971. 32:833–841.23. Sklar C, Whitton J, Mertens A, Stovall M, Green D, Marina N, Greffe B, Wolden S, Robison L. Abnormalities of the thyroid in survivors of Hodgkin's disease: data from the childhood cancer survivor study. J Clin Endocrinol Metab. 2000. 85:3227–3232.24. Boulad F, Bromley M, Black P, Heller G, Sarafoglou K, Gillio A, Papadopoulos E, Sklar C. Thyroid dysfunction following bone marrow transplantation using hyperfrationated radiation. Bone Marrow Transplant. 1995. 15:71–76.25. Toubert ME, Socié G, Gluckman E, Aractingi S, Espérou H, Devergie A, Ribaud P, Parquet N, Schlageter MH, Beressi JP, Rain JD, Vexiau P. Short and long-term follow-up of thyroid dysfunction after allogeneic bone marrow transplantation without the use of preoperative total body irradiation. Br J Haematol. 1997. 98:453–457.26. Slatter MA, Gennery AR, Cheetham TD, Bhattacharya A, Crooks BN, Flood TJ, Cant AJ, Abinun M. Thyroid dysfunction after bone marrow transplantation for primary immunodeficiency without the use of total body irradiation in conditioning. Bone Marrow Transplant. 2004. 33:949–953.
Article27. Sarafoglou K, Boulad F, Gillio A, Sklar C. Gonadal dysfunction after bone marrow transplantation for acute leukemia during childhood. J Pediatr. 1997. 130:210–216.28. Matsumoto M, Shinohara O, Ishiguro H, Shimizu T, Hattori K, Ichikawa M, Yabe H, Kubota C, Yabe M, Kato S. Ovarian function after bone marrow transplantation before menarche. Arch Dis Child. 1999. 80:452–454.29. Michel G, Socié G, Gebhard F, Bernaudin F, Thuret I, Vannier JP, Demeocq F, Leverger G, Pico JL, Rubie H, Mechinaud F, Reiffers J, Gratecos N, Troussard X, Jouet JP, Simonin G, Gluckman E, Maraninchi D. Late effects of allogeneic bone marrow transplantation for children with acute myeloblastic leukemia in first complete remission: the impact of conditioning regimen without total-body irradiation-a report from the Societe Francaise de Greffe de Moelle. J Clin Oncol. 1997. 15:2238–2246.30. Sanders JE, Hawley J, Levy W, Gooley T, Buckner CD, Deeg HJ, Doney K, Storb R, Sullivan K, Witherspoon R, Appelbaum FR. Pregnancies following high-dose cyclophosphamide with or without high-dose busulfan or total-body irradiation and bone marrow transplantation. Blood. 1996. 87:3045–3052.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Opening the era of in vivo xenotransplantation model for hematopoietic stem cell transplantation
- Hematopoietic stem cell transplantation: overview for general pediatrician
- Hematopoietic Stem Cell Transplantation
- Hematopoietic Stem Cell Transplantation in Inborn Error of Metabolism
- The Strategies for the Prevention of Chronic GVHD in Hematopoietic Stem Cell Transplantation