J Korean Med Sci.
2008 Oct;23(5):753-761. 10.3346/jkms.2008.23.5.753.
Venous Air Embolism during Surgery, Especially Cesarean Delivery
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Anesthesia and Pain Research Institute, Yonsei University College of Medicine, Seoul, Korea. kkj6063@yuhs.ac
- 2Department of Anesthesia and Perioperative Care, University of California, San Francisco, USA.
- 3Department of Obstetrics and Gynecology, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 1783056
- DOI: http://doi.org/10.3346/jkms.2008.23.5.753
Abstract
- Venous air embolism (VAE) is the entrapment of air or medical gases into the venous system causing symptoms and signs of pulmonary vessel obstruction. The incidence of VAE during cesarean delivery ranges from 10 to 97% depending on surgical position or diagnostic tools, with a potential for life-threatening events. We reviewed extensive literatures regarding VAE in detail and herein described VAE during surgery including cesarean delivery from background and history to treatment and prevention. It is intended that present work will improve the understanding of VAE during surgery.
Keyword
MeSH Terms
-
Anesthesia, Obstetrical/adverse effects
Cesarean Section/*adverse effects
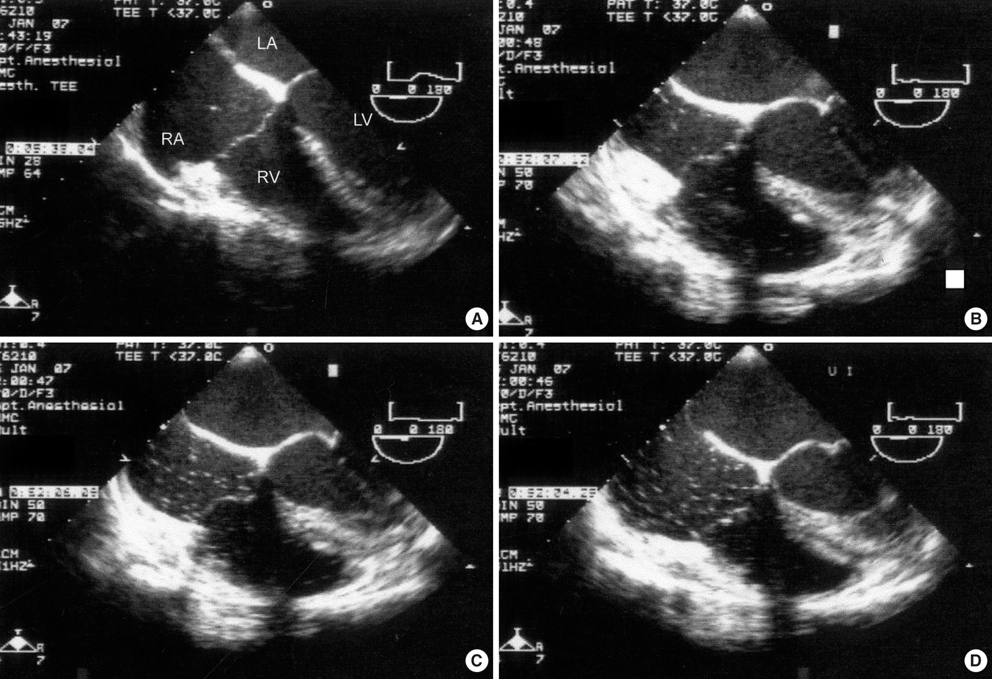
Echocardiography, Transesophageal/methods
Embolism, Air/*diagnosis/prevention & control/*ultrasonography
Female
Humans
Intraoperative Complications/ultrasonography
Monitoring, Intraoperative/methods
Obstetrics/methods
Pregnancy
Risk Factors
Ultrasonography, Doppler/methods
Figure
Cited by 3 articles
-
Carbon Dioxide Embolism during Laparoscopic Surgery
Eun Young Park, Ja-Young Kwon, Ki Jun Kim
Yonsei Med J. 2012;53(3):459-466. doi: 10.3349/ymj.2012.53.3.459.Incidence of Venous Air Embolism during Myomectomy: The Effect of Patient Position
Jiwon An, Seo Kyung Shin, Ja-Young Kwon, Ki Jun Kim
Yonsei Med J. 2013;54(1):209-214. doi: 10.3349/ymj.2013.54.1.209.Venous Air Embolism Not Amniotic Fluid Embolism
Charles Her
Korean J Crit Care Med. 2016;31(1):68-70. doi: 10.4266/kjccm.2016.31.1.68.
Reference
-
1. Mommerot A, Perrault LP. Carbon dioxide embolism induced by endoscopic saphenous vein harvesting during coronary artery bypass grafting. J Thorac Cardiovasc Surg. 2006. 132:1502.
Article2. Staffieri F, Lacitignola L, De Siena R, Crovace A. A case of spontaneous venous embolism with carbon dioxide during laparoscopic surgery in a pig. Vet Anaesth Analg. 2007. 34:63–66.
Article3. Kama NA. Influence of nitrous oxide anesthesia on venous gas embolism with carbon dioxide and helium during pneumoperitoneum. Surg Endosc. 2001. 15:1237–1238.
Article4. Cottin V, Viale JP, Bouffard Y, Delafosse B. Severe nitrous oxide embolism during venous stripping. Intensive Care Med. 1997. 23:1287–1288.
Article5. Boussuges A, Blanc F, Carturan D. Hemodynamic changes induced by recreational scuba diving. Chest. 2006. 129:1337–1343.
Article6. Risberg J, Englund M, Aanderud L, Eftedal O, Flook V, Thorsen E. Venous gas embolism in chamber attendants after hyperbaric exposure. Undersea Hyperb Med. 2004. 31:417–429.7. Mitchell SJ, Benson M, Vadlamudi L, Miller P. Cerebral arterial gas embolism by helium: an unusual case successfully treated with hyperbaric oxygen and lidocaine. Ann Emerg Med. 2000. 35:300–303.
Article8. Papadopoulos G, Kuhly P, Brock M, Rudolph KH, Link J, Eyrich K. Venous and paradoxical air embolism in the sitting position. A prospective study with transoesphageal echocardiography. Acta Neurochir (wien). 1994. 126:140–143.9. Losasso TJ, Muzzi DA, Dietz NM, Cucchiara RF. Fifty percent nitrous oxide does not increase the risk of venous air embolism in neurosurgical patients operated upon in the sitting position. Anesthesiology. 1992. 77:21–30.
Article10. Albin MS, Carroll RG, Maroon JC. Clinical considerations concerning detection of venous air embolism. Neurosurgery. 1978. 3:380–384.
Article11. Michel R. Air embolism in hip surgery. Anaesthesia. 1980. 35:858–862.
Article12. Schmandra TC, Mierdl S, Bauer H, Gutt C, Hanisch E. Transoesophageal echocardiography shows high risk of gas embolism during laparoscopic hepatic resection under carbon dioxide pneumoperitoneum. Br J Surg. 2002. 89:870–876.
Article13. Maddukuri P, Downey BC, Blander JA, Pandian NG, Patel AG. Echocardiographic diagnosis of air embolism associated with central venous catheter placement: case report and review of the literature. Echocardiography. 2006. 23:315–318.
Article14. Rabe C, Balta Z, Wüllner U, Heller J, Hammerstingl C, Tiemann K, Sommer T, Schepke M, Fischer HP, Sauerbruch T. Biliary metal stents and air embolism: a note of caution. Endoscopy. 2006. 38:648–650.
Article15. Cuvelier A, Muir JF. Images in clinical medicine: venous air embolism. N Engl J Med. 2006. 354:e26.16. Ho AM, Ling E. Systemic air embolism after lung trauma. Anesthesiology. 1999. 90:564–575.
Article17. Southern DA, Arramovic J, Fitzsimmons K. Air embolism following abdominal stab-wound. Anaesth Intensive Care. 1996. 24:623.18. Cormack JR. The entrance of air by the open mouths of the veins, considered as cause of danger and death after parturition. London Med J. 1850. 2:928.19. Durant TM, Long J, Oppenheimer MJ. Pulmonary venous air embolism. Am Heart J. 1947. 33:269–281.
Article20. Waldrop GS. Fatal air embolism during term labor and the puerperium. Obstet Gynecol. 1953. 1:454–459.21. Merrill DG, Samuels SI, Silverberg GD. Venous air embolism of uncertain etiology. Anesth Analg. 1982. 61:65–66.
Article22. Younker D, Rodriguez V, Kavanagh J. Massive air embolism during cesarean section. Anesthesiology. 1986. 65:77–79.
Article23. Fong J, Gadalla F, Gimbel AA. Precordial Doppler diagnosis of haemodynamically compromising air embolism during caesarean section. Can J Anaesth. 1990. 37:262–264.
Article24. Lang S. Precordial Doppler diagnosis of haemodynamically compromising air embolism during caesarean section. Can J Anaesth. 1991. 38:255–256.
Article25. Mushkat Y, Luxman D, Nachum Z, David MP, Melamed Y. Gas embolism complicating obstetric or gynecologic procedures. Case reports and review of the literature. Eur J Obstet Gynecol Reprod Biol. 1995. 63:97–103.
Article26. Epps SN, Robbins AJ, Marx GF. Complete recovery after near-fatal venous air embolism during cesarean section. Int J Obstet Anesth. 1998. 7:131–133.
Article27. Kostash MA, Mensink F. Lethal air embolism during cesarean delivery for placenta previa. Anesthesiology. 2002. 96:753–754.
Article28. Nims M, Hallonguist H, Camann W. Coronary arterial air embolus occurring during cesarean delivery. Int J Obstet Anesth. 2006. 15:166–169.
Article29. Malinow AM, Naulty JS, Hunt CO, Datta S, Ostheimer GW. Precordial ultrasonic monitoring during cesarean delivery. Anesthesiology. 1987. 66:816–819.
Article30. Fong J, Gadalla F, Pierri MK, Druzin M. Are Doppler-detected emboli during cesarean section air emboli? Anesth Analg. 1990. 71:254–257.31. Karuparthy VR, Downing JW, Husain FJ, Knape KG, Blanchard J, Solomon D. Incidence of venous air embolism during cesarean section is unchanged by the use of a 5 to 10o head-up tilt. Anesth Analg. 1989. 69:620–623.32. Fong J, Gadalla F, Druzin M. Venous emboli occurring caesarean section: the effect of patient position. Can J Anaesth. 1991. 38:191–195.33. Handler JS, Bromage PR. Venous air embolism during cesarean delivery. Reg Anesth. 1990. 15:170–173.34. Vartikar JV, Johnson MD, Datta S. Precordial Doppler monitoring and pulse oximetry during cesarean delivery: detection of venous air embolism. Reg Anesth. 1989. 14:145–148.35. Lew TW, Tay DH, Thomas E. Venous air embolism during cesarean section: more common than previously thought. Anesth Analg. 1993. 77:448–452.
Article36. Kaunitz AM, Hughes JM, Grimes DA, Smith JC, Rochat RW, Kafrissen ME. Causes of maternal mortality in the united states. Obstet Gynecol. 1985. 65:605–612.
Article37. Maroon JC, Goodman JM, Horner TG, Campbell RL. Detection of minute venous air emboli with ultrasound. Surg Gynecol Obstet. 1968. 127:1236–1238.38. Butler BD, Hills BA. The lung as a filter for microbubbles. J Appl Physiol. 1979. 47:537–543.
Article39. Butler BD, Hills BA. Transpulmonary passage of venous air emboli. J Appl Physiol. 1985. 59:543–547.
Article40. Nelson PK. Pulmonary gas embolism in pregnancy and the puerperium. Obstet Gynecol Surv. 1960. 15:449–481.
Article41. Hlastala MP, Bobertson HT, Ross BK. Gas exchange abnormalities produced by venous gas emboli. Respir Physiol. 1979. 36:1–17.
Article42. Deem S, McKinney S, Polissar NL, Hedges RG, Swenson ER. Hemodilution during venous gas embolization improves gas exchange, without altering V(A)/Q or pulmonary blood flow distributions. Anesthesiology. 1999. 91:1861–1872.
Article43. Souders JE. Pulmonary air embolism. J Clin Monit Comput. 2000. 16:375–383.44. Verstappen FT, Bernards JA, Kreuzer F. Effects of pulmonary gas embolism on circulation and respiration in the dog. IV. Origin of arterial hypoxemia during pulmonary gas embolism. Pflugers Arch. 1977. 370:71–75.45. Wang D, Ki MH, Hsu K, Shen CY, Chen HI, Lin YC. Air embolism induced lung injury in isolated rat lungs. J Appl Physiol. 1992. 72:1235–1242.46. Albertine KH, Wiener-Kronish JP, Koike K, Staub NC. Quantification of damage by air emboli to lung microvessels in anesthetized sheep. J Appl Physiol. 1984. 57:1360–1368.
Article47. Ohkuda K, Nakahara K, Binder A, Staub NC. Venous air emboli in sheep: reversible increase in lung microvascular permeability. J Appl Physiol. 1981. 51:887–894.
Article48. Furuya H, Suzuki T, Okumura F, Kishi Y, Uefuji T. Detection of air embolism by transesophageal echocardiography. Anesthesiology. 1983. 58:124–129.
Article49. Milani RV, Lavie CJ, Gilliland YE, Cassidy MM, Bernal JA. Overview of transesophageal echocardiography for the chest physician. Chest. 2003. 124:1081–1089.
Article50. Gibby GL. Precordial Doppler is not obsolete for venous air embolism monitoring. Anesthesiology. 1988. 68:829.
Article51. Gildenberg PL, O'Brien RP, Britt WJ, Frost EA. The efficacy of Doppler monitoring for the detection of venous air embolism. J Neurosurg. 1981. 54:75–78.
Article52. Schubert A, Deogaonkar A, Drummond JC. Precordial Doppler probe placement for optimal detection of venous air embolism during craniotomy. Anesth Analg. 2006. 102:1543–1547.
Article53. Matjasko J, Petrozza P, Mackenzie CF. Sensitivity of end-tidal nitrogen in venous air embolism detection in dogs. Anesthesiology. 1985. 63:418–423.
Article54. Russell GB, Richard RB, Snider MT. Detection of venous air embolism in dogs by emission spectrometry. J Clin Monit. 1990. 6:18–23.
Article55. Drummond JC, Prutow RJ, Scheller MS. A comparison of the sensitivity of pulmonary artery pressure, end-tidal carbon dioxide, and end-tidal nitrogen in the detection of venous air embolism in the dog. Anesth Analg. 1985. 64:668–692.
Article56. Matjasko MJ, Hellman J, Mackenzie CF. Venous air embolism, hypotension, and end-tidal nitrogen. Neurosurgery. 1987. 21:378–382.
Article57. Losasso TJ, Black S, Muzzi DA, Michenfelder JD, Cucchiara RF. Detection and hemodynamic consequences of venous air embolism. Does nitrous oxide make a difference? Anesthesiology. 1992. 77:148–152.58. Burton A, Camann W. Electrocardiographic changes during cesarean section: a review. Int J Obstet Anesth. 1996. 5:47–53.
Article59. Mathew JP, Fleisher LA, Rinehouse JA, Sevarino FB, Sinatra RS, Nelson AH, Prokop EK, Rosenbaum SH. ST segment depression during labor and delivery. Anesthesiology. 1992. 77:635–641.
Article60. Williamson JA, Helps SC, Westhorpe RN, Mackay P. Crisis management during anaesthesia: embolism. Qual Saf Health Care. 2005. 14:e17.
Article61. Giebler R, Kollenberg B, Pohlen G, Peters J. Effect of positive end-expiratory pressure on the incidence of venous air embolism and on the cardiovascular response to the sitting position during neurosurgery. Br J Anaesth. 1998. 80:30–35.
Article62. Zasslow MA, Pearl RG, Larson CP, Silverberg G, Shuer LF. PEEP does not affect left atrial-right atrial pressure difference in neurosurgical patients. Anesthesiology. 1988. 68:760–763.
Article63. Clarke NR, Timperley J, Kelion AD, Banning AP. Transthoracic echocardiography using second harmonic imaging with Valsalva manoeuvre for the detection of right to left shunts. Eur J Echocardiogr. 2004. 5:176–181.
Article64. Meyer PG, Cuttaree H, Charron B, Jarreau MM, Perie AC, Sainte-Rose C. Prevention of venous air embolism in paediatric neurosur-gical procedures performed in the sitting position by combined use of MAST suit and PEEP. Br J Anaesth. 1994. 73:795–800.
Article65. Butler BD, Conkin J, Luehr S. Pulmonary hemodynamics, extravascular lung water and residual gas bubbles following low dose venous gas embolism in dogs. Aviat Space Environ Med. 1989. 60:1178–1182.66. Martin JT. Neuroanesthetic adjuncts for surgery in the sitting position. II. The antigravity suit. Anesth Analg. 1970. 49:588–593.67. Tinker JH, Vandam LD. How effective is the G suit in neurosurgical operations? Anesthesiology. 1972. 36:609–611.
Article68. Oppenheimer MJ, Durant TM, Lynch P. Body position in relation to venous air embolism and the associated cardiovascular-respiratory changes. Am J Med Sci. 1953. 225:362–373.
Article69. Geissler HJ, Allen SJ, Mehlhorn U, Davis KL, Morris WP, Butler BD. Effect of body repositioning after venous air embolism. An echocardiographic study. Anesthesiology. 1997. 86:710–717.70. Butler BD, Luehr S, Katz J. Venous gas embolism: time course of residual pulmonary intravascular bubbles. Undersea Biomed Res. 1989. 16:21–29.71. Kyttä J, Tanskanen P, Randell T. Comparison of the effects of controlled ventilation with 100% oxygen, 50% oxygen in nitrogen, and 50% oxygen in nitrous oxide on responses to venous air embolism in pigs. Br J Anaesth. 1996. 77:658–661.
Article72. Roberts MW, Mathiesen KA, Ho HS, Wolfe BM. Cardiopulmonary responses to intravenous infusion of soluble and relatively insoluble gases. Surg Endosc. 1997. 11:341–346.
Article73. Knüttgen D, Stölzle U, Köning W, Müller MR, Doehn M. Air embolism in the sitting position. Oxygen/nitrogen versus oxygen/laughing gas. Anaesthesist. 1989. 38:490–497.74. Adornato DC, Gildenberg PL, Ferrario CM, Smart J, Frost EA. Pathophysiology of intravenous air embolism in dogs. Anesthesiology. 1978. 49:120–127.
Article75. Bowdle TA, Artru AA. Positioning the air aspiration pulmonary artery catheter introducer sheath by intravascular electrocardiography. Anesthesiology. 1988. 69:276–279.
Article76. Calvin JE Jr. Acute right heart failure: pathophysiology, recognition, and pharmacological management. J Cardiothorac Vasc Anesth. 1991. 5:507–513.
Article77. Vlahakes GJ, Turley K, Hoffman JI. The pathophysiology of failure in acute right ventricular hypertension: hemodynamic and biochemical correlations. Circulation. 1981. 63:87–95.
Article78. Angle MR, Molloy DW, Penner B, Jones D, Prewitt RM. The cardiopulmonary and renal hemodynamic effects of norepinephrine in canine pulmonary embolism. Chest. 1989. 95:1333–1337.
Article79. Monrad ES, Baim DS, Smith HS, Lanoue AS. Milrinone, dobutamine, and nitroprusside: comparative effects on hemodynamics and myocardial energetics in patients with severe congestive heart failure. Circulation. 1986. 73:III168–III174.80. Jardin F, Genevray B, Brun-Ney D, Margairaz A. Dobutamine: a hemodynamic evaluation in pulmonary embolism shock. Crit Care Med. 1985. 13:1009–1012.
Article81. Nayagam J, Ho KM, Liang J. Fatal systemic air embolism during endoscopic retrograde cholangio-pancreatography. Anaesth Intensive Care. 2004. 32:260–264.
Article82. Murphy BP, Harford FJ, Cramer FS. Cerebral air embolism resulting from invasive medical procedures. Treatment with hyperbaric oxygen. Ann Surg. 1985. 201:242–245.
Article83. Russell GB, Snider MT, Richard RB, Loomis JL. Venous air emboli with 15N2: pulmonary excretion and physiologic responses in dogs. Undersea Biomed Res. 1991. 18:37–45.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Fatal Venous Air Embolism during Lung Surgery
- Incidence of Venous Air Embolism Ddetected by Ultrasonic Doppler during Cesarean Section
- Massive Intraventricular Air Embolism after Contrast-enhanced CT: Report of Two Cases
- Venous air embolism during hepatic resection in a patient with liver cirrhosis: A case report
- A Case of Systemic Air Embolism in a Child after Thoracic Blunt Trauma